Topic 11: Animal physiology (HL)
11.4 Sexual and reproduction
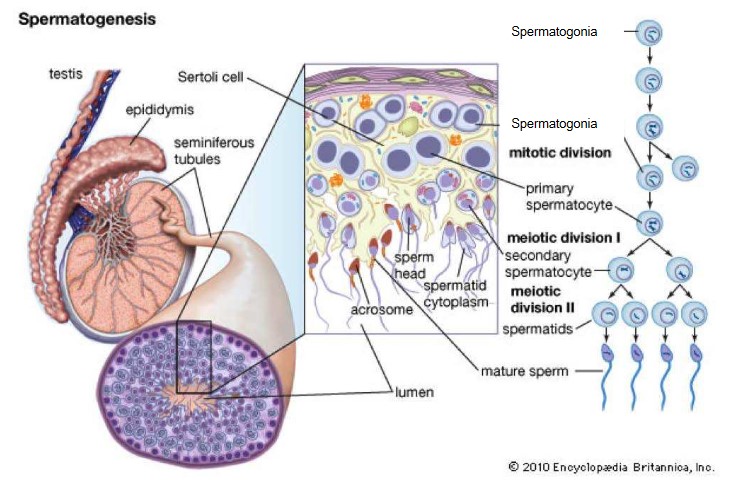
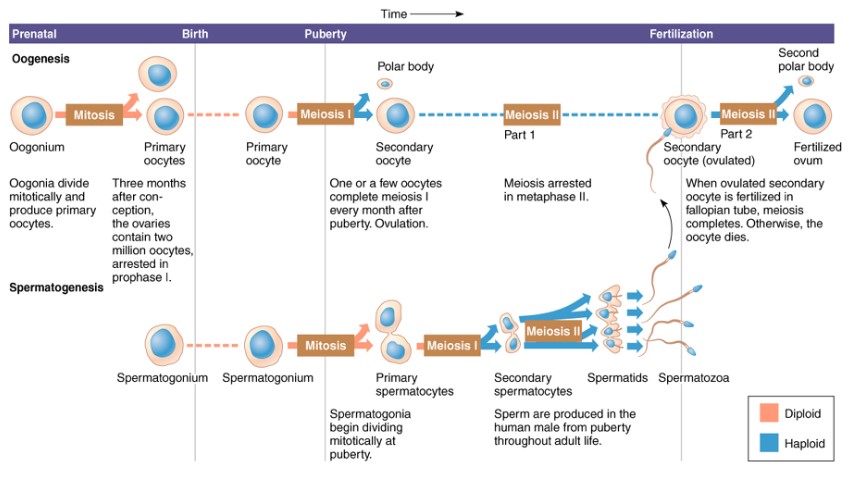
Spermatogenesis:
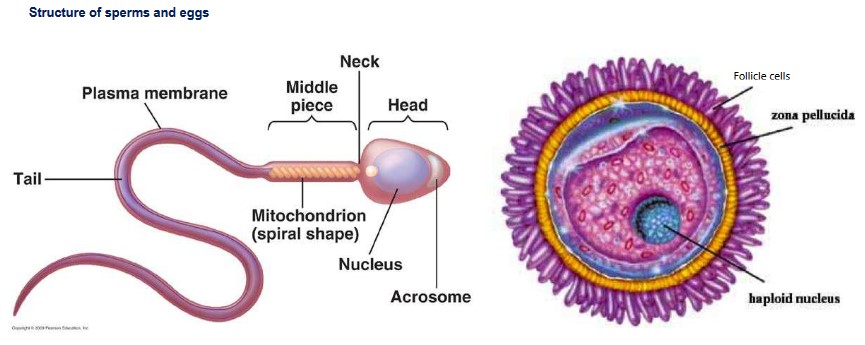
- Spermatogenesis is basically the production of sperm (male gametes) through meiosis.
- Occurs in the testes of male
- Spermatogonia (stem cells of the sperm – 2n) are located at the periphery of each seminiferous tubules.
- Developing sperm move towards the central opening of the tubule (lumen) as they undergo meiosis and differentiation.
- Mature sperm will be stored in epididymis.
- Spermatogonia is first divided by mitosis to form more 2n cells, called primary spermatocytes.
- Primary spermatocytes undergo meiosis I to form two secondary spermatocytes.
- Two secondary spermatocytes undergo meiosis II to form four early spermatids.
- Early spermatids will go through cell differentiation and form mature sperms.
- Sperms are released into the lumen of the seminiferous tubules where they are transported to the epididymis. The sperm attain full motility in the epididymis.
- Cells in between the developing spermatocytes called Leydig cells, which produce testosterone in the presence of LH (luteinizing hormone) to aid in the development of the sperm
- Sertoli cells nourish the spermatids as they mature and differentiate into sperms
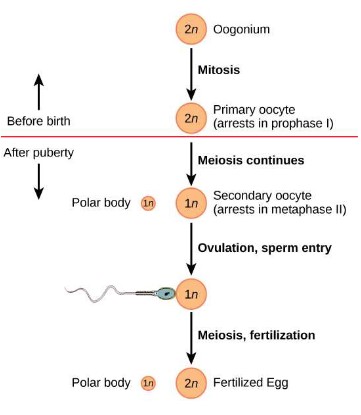
Oogenesis:
- Oogenesis is basically the production of female eggs (female gametes) through meiosis.
- Germ cells (2n) in the fetal ovary divide by mitosis to produce many 2n germ cells called oogonia.
- Oogonia will grow in the cortex until they are large enough and ready to go through meiosis; they are called primary oocytes.
- The primary oocytes begin to go through the first division of meiosis, which is arrested (stopped) in prophase I
- This is called the primary oocytes (about 400,000 in a female when she is born).
- These oocytes remain in the first stage of meiosis until the girl reaches puberty and begins her menstrual cycle.
- Every month a primary follicle finishes meiosis I to form two haploid (n) cells (one haploid cell is much larger than the other cell). This development is stimulate by FSH.
- The large cell is a secondary oocyte and the small cell is called the polar body.
- The secondary oocyte develops inside what is known as the mature follicle
- As the large secondary oocyte begins to go through the second meiotic division, it is released from the ovary.
- It will not complete the second meiotic division unless the oocyte is fertilized.
- When meiosis II is complete you have an ovum and another polar body.
- Follicle cells are providing nourishment.
Fertilisation:
- Fertilization is the combining of the male and female gametes to produce a zygote.
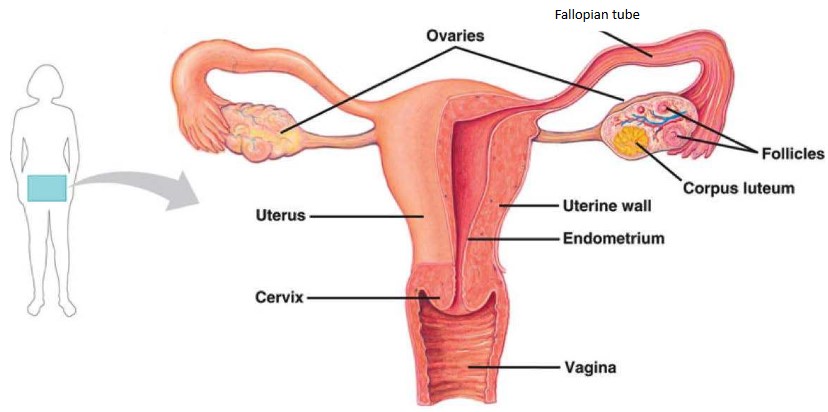
- Sperm are ejaculated into the vagina of a female and are stimulated to swim by calcium ions in the vaginal fluids.
- The sperm follow chemical signals produced by the egg, until they reach the fallopian tubes, which is where the majority of fertilizations take place.
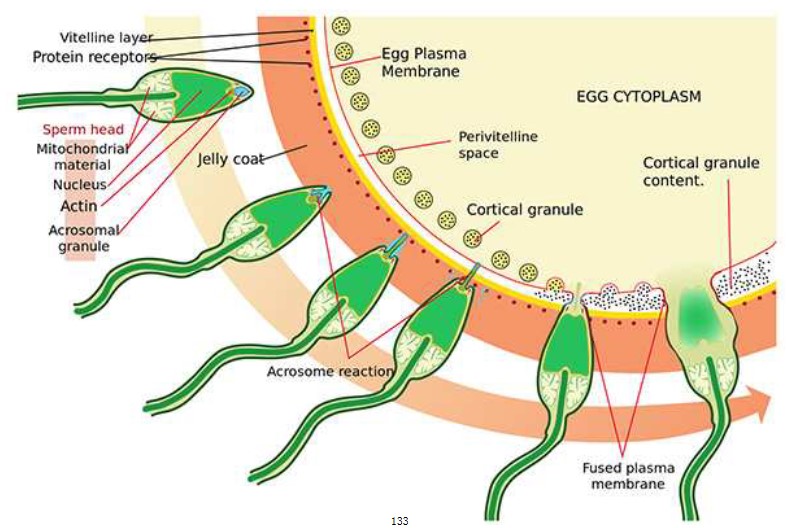
- When the sperm reaches the egg, a reaction called the acrosome reaction takes place that allows the sperm to break through the layer of glycoproteins.
- The acrosome in head of the sperm releases hydrolytic enzymes onto the glycoprotein layer surrounding the egg called the zona pellucida.
- This digests the layer allowing the sperm to force their way through the zona pellucida through vigorous tail beating.
- The first sperm that makes it through comes into contact and fuses with the egg’s membrane (The membrane at the tip of the sperm has special proteins
that can bind to the now exposed membrane of the egg), releasing the sperm’s nucleus into the egg cell. - The entry of sperm will stimulate meiosis II and release \(Ca^{2+}\) ions, which will stimulate the release of cortical granules.
- When the membranes fuse together, cortical granules near the surface of the egg membrane are released by exocytosis.
- The chemicals in the granules combine with the glycoproteins in the zona pellucida.This causes the glycoproteins in the zona pellucida to cross-link with each other, creating a hard layer impermeable to the other sperm.
- This prevents fertilization of an egg by more than one sperm.
Internal/external fertilisation:
- Without water to prevent drying out of the egg and sperm, terrestrial animals rely on internal fertilization
- This insures the close proximity of the sperm and egg in order to insure fertilization takes place
- Most aquatic organisms generally rely on external fertilization, which involves releasing the sperm and egg at a close proximity, into the water outside the female’s body
- External fertilization increases the risk of successfully creating offspring
- Several risks include predation and changes to the external environment (pH, pollution and temperature etc.)
Structure of the ovary
Embryonic development:
- After the male and the female gametes combine to form a zygote, the zygote divides by mitosis to form a two-cell embryo.
- They two cells grow and replicate their DNA, and undergo another cell division through mitosis to form a four-cell embryo.
- As the embryo is developing, it is moving along the fallopian tube towards the uterus.
- The four-cell embryo continues to divide by cell division until it reaches 16 cells; called the morula.
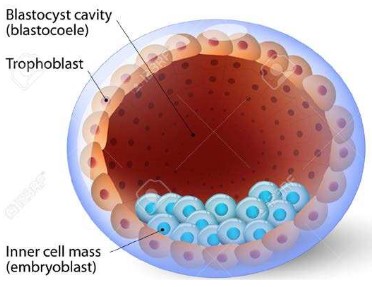
- After continued cell divisions a blastocyst consisting of 100 to 128 cells is formed and is ready for implantation into the endometrium.
- The blastocyst consists of an inner cell mass that will develop into the body of the embryo, a group of cells surrounding the embryo called the trophoblast that will develop into the placenta.
- Morula is the ball of totipotent stem cells, while blastocyst is already differentiated into inner cell mass and trophoblast, which is pluripotent stem cells.
- The blastocyst must implant into the endometrium to develop the placenta and continue growing.
- If the blastocyst implants into the fallopian tube, it will cause severe complication and even death for mother
HCG hormones:
- When a human embryo is implanted into the endometrium or the uterine lining, it starts to produce the hormone, HCG.
- We can test HCG level for pregnancy.
- HCG promotes the maintenance of the corpus luteum and prevents its disintegration.
- This allows for the continued production of progesterone and estrogen which is critical for pregnancy.
- Progesterone and estrogen will inhibit the production of FSH and LH, thereby stopping the release of new egg.
- Progesterone maintains the endometrium while blastocyst develops into placenta and embryo
- HCG might repel the immune cells of the mother thus protecting the fetus during early development.
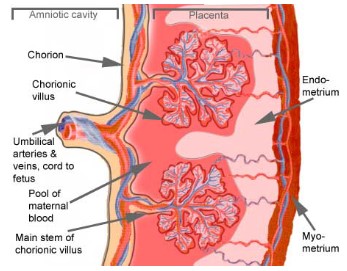
Placenta:
- The placenta develops from the trophoblast layer of the blastocyst.
- When developed three blood vessels contained within umbilical cord connect the placenta to the growing fetus.
- Two umbilical arteries carry deoxygenated blood and waste away from the fetus to the placenta.
- As maternal blood enters the placenta it leaves the arteries and enters the inter-villous space, where it pools and surrounds the placental villi.
- The placental villi are finger-like fetal tissues that have a large surface area for the exchange of materials such as gases, nutrients and wastes.
- Fetal blood that circulates in capillaries within the villi and microvilli isvery close to the surface, allowing for efficient exchange of materials between the fetal and maternal blood.
- Materials such as oxygen, nutrients and vitamins diffuse into the fetal capillaries from the maternal blood in the inter-villous space, while carbon dioxide and wastes diffuse out of the fetal capillaries into the inter-villous space.
- One umbilical vein carries oxygenated and nutrient rich blood back to the fetus from the placenta.
- The cells that separate the fetal and maternal blood form a semi-permeable placental barrier
- The placenta also starts to produce progesterone and estrogen after about 9 weeks taking over from the corpus luteum. The placenta produces enough of these steroids to maintain the pregnancy and the corpus luteum is no longer needed.
- These hormones are necessary to maintain the rich blood supply needed by the placenta.
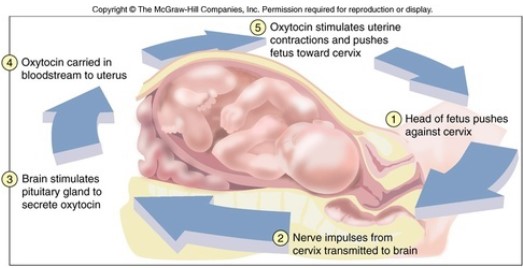
Giving birth
- When the pregnancy is at term, the fetus secretes hormones that signal the placenta to stop producing progesterone (progesterone inhibits the secretion of oxytocin by the pituitary gland).
- Baby’s head engages with the cervix
- The stretch receptors on the cervix will send signal to produce oxytocin
- Oxytocin secreted stimulates the muscle fibers in the uterus to begin to contract.
- As the muscles in uterus contract, stretch receptors sends stronger signal to produce more oxytocin.
- More oxytocin increases the frequency and intensity of the contractions, thus stimulating the production of even more oxytocin.
- This is an example of positive feedback.
- Contractions of the muscles of the uterus will cause the amniotic sac to break, releasing the amniotic fluid (This is when the “water breaks” in childbirth).
- Relaxation of the muscles in the cervix causes it to dilate, eventually allowing the increasing contractions to push the baby out through the vagina and the cervix.
- When baby gets out, umbilical cord is clamped and cut.
- The placenta is expelled “afterbirth” about 15 min after the baby is born