- IB Style Question Banks with Solution
- IB DP Biology SL- IB Style Practice Questions with Answer-Topic Wise-Paper 1
- IB DP Biology HL- IB Style Practice Questions with Answer-Topic Wise-Paper 1
- IB DP Biology SL- IB Style Practice Questions with Answer-Topic Wise-Paper 2
- IB DP Biology HL- IB Style Practice Questions with Answer-Topic Wise-Paper 2
6.2 The Blood System
Essential Idea:
The blood system continuously transports substances to cells and simultaneously collects waste products
Understandings:
- Arteries convey blood at high pressure from the ventricles to the tissues of the body
- Arteries have muscle cells and elastic fibres in their walls
- The muscle and elastic fibres assist in maintaining blood pressure between pump cycles
- Blood flows through tissues in capillaries
- Capillaries have permeable walls that allow exchange of material between cells in the tissue and the blood in the capillary
- Veins collect blood at low pressure from the tissues of the body and return it to the atria of the heart
- Valves in veins and the heart ensure circulation of blood by preventing backflow
- There is a separate circulation for the lungs
- The heart beat is initiated by a group of specialised muscle cells in the right atrium called the sinoatrial node
- The sinoatrial node acts as a pacemaker
- The sinoatrial node sends out an electrical signal that stimulates contraction as it is propagated through the walls of the atria and then the walls of the ventricles
- The heart rate can be increased or decreased by impulses brought to the heart through two nerves from the medulla of the brain
- Epinephrine increases the heart rate to prepare for vigorous physical activity
Applications:
- William Harvey’s discovery of the circulation of blood with the heart acting as a pump
- Pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle
- Causes and consequences of occlusion of the coronary arteries
Skills:
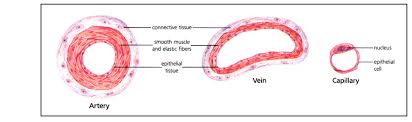
- Identification of blood vessels as arteries, capillaries or veins from the structure of their walls
- Recognition of the chambers and valves of the heart and the blood vessels connected to it in dissected hearts or in diagrams of heart structure
- State the function of arteries.
- Outline the role of elastic and muscle tissue in arteries.
- State the reason for toughness of artery walls.
- Describe the structure and function of the three layers of artery wall tissue.
- Describe the mechanism used to maintain blood flow in arteries between heartbeats.
- Define systolic and diastolic blood pressure.
- Define vasoconstriction and vasodilation.
- Describe the structure and function of capillaries.
- Describe the cause and effect of diffusion of blood plasma into and out of a capillary network.
- State the function of veins.
- Outline the roles of gravity and skeletal muscle pressure in maintaining flow of blood through a vein.
- Outline the structure and function of a pocket valve.
- Draw a diagram to illustrate the double circulation system in mammals.
- Compare the circulation of blood in fish to that of mammals.
- Explain the flow of blood through the pulmonary and systemic circulations.
- Explain why the mammalian heart must function as a double pump.
- Define myogenic contraction.
- Outline the role of cells in the sinoatrial node.
- State the reason why the sinoatrial node is often called the pacemaker.
- Describe the propagation of the electrical signal from the sinoatrial node through the atria and ventricles.
- Outline the structures and functions of nervous tissue that can regulate heart rate.
- Describe factors that will increase heart rate.
- Describe factors that will decrease heart rate.
- Outline conditions that will lead to epinephrine secretion.
- Explain the effect of epinephrine on heart rate.
- Outline William Harvey’s role in discovery of blood circulation.
- Describe the cause and consequence of atherosclerosis.
- Outline the effect of a coronary occlusion on heart function.
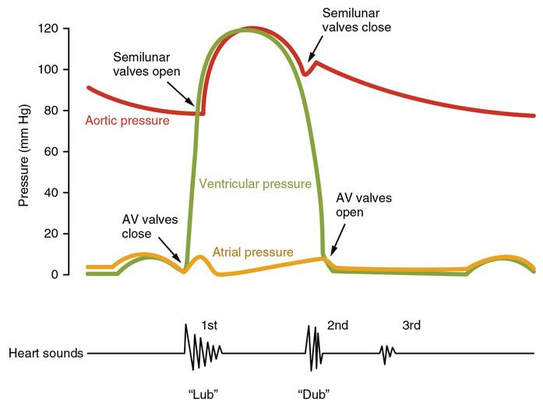
- Explain the pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle.
- Explain the relationship between atrial and ventricular pressure and the opening and closing of heart valves.
- Explain the atrial, ventricular and arterial pressure changes as illustrated on a graph of pressure changes during the cardiac cycle.
- Identify the time of opening and closing of heart valves on a graph o f pressure changes during the cardiac cycle.
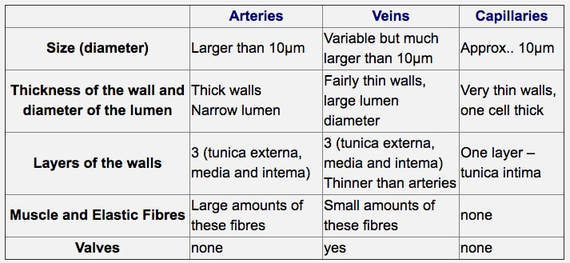
- Compare the diameter, relative wall thickness, lumen diameter, number of wall layers, abundance of muscle and elastic fibres and presence of valves in arteries, capillaries and veins.
- Given a micrograph, identify a blood vessel as an artery, capillary or vein.
- Label a diagram of the heart with the following structure names: superior vena cava, inferior vena cava, pulmonary semilunar valve, aorta, pulmonary artery, pulmonary veins, aortic semilunar valve, left atrioventricular valve, left ventricle, septum, right ventricle, left atrium, right atrium and right atrioventricular valve.
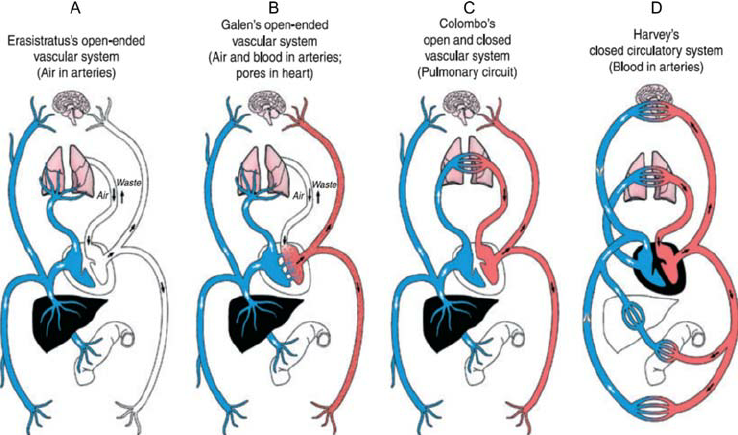
- Outline Galen’s description of blood flow in the body.
- Describe how Harvey was able to disprove Galen’s theory.
Topic 6.2: the blood system
In the Blood System unit we we learn about how our blood system provides a delivery and collection service for the whole body. The heart, blood and blood vessels make up a most efficient transport system that reaches all cells, bringing the substances they need and taking away their waste. You will also learn that humans and other mammals have what is known as a closed circulatory system with blood contained inside a network of arteries, veins and capillaries.
This unit will last 4 school days
Essential idea:
- The blood system continuously transports substances to cells and simultaneously collects waste products.
Nature of science:
- Theories are regarded as uncertain—William Harvey overturned theories developed by the ancient Greek philosopher Galen on movement of blood in the body. (1.9)
- Outline Galen’s description of blood flow in the body.
- Describe how Harvey was able to disprove Galen’s theory.
6.2.U1 Arteries convey blood at high pressure from the ventricles to the tissues of the body.
- State the function of arteries.
- Outline the role of elastic and muscle tissue in arteries.
- State the reason for toughness of artery walls.
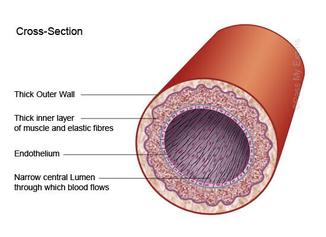
- They have a narrow lumen (relative to wall thickness) to maintain a high blood pressure (~ 80 – 120 mmHg)
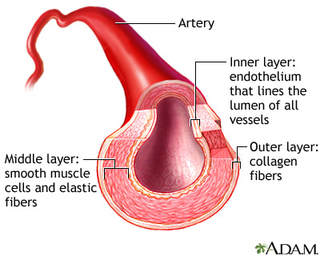
- They have a thick wall containing an outer layer of collagen to prevent the artery from rupturing under the high pressure
- Very thick wall of smooth muscle tissue surrounding arteries makes them strong and elastic in nature with a narrow lumen (area where the blood flows).
- Elastin fibres store energy when they are stretched by the flow of blood. As they recoil the blood is further propelled through the artery.
- The thick smooth muscle layer in the arteries can be used to help regulate blood pressure by changing the diameter of the arteries.
6.2.U2 Arteries have muscle cells and elastic fibres in their walls.
- Describe the structure and function of the three layers of artery wall tissue.
Tunica media– thick layer containing smooth muscle and elastin fibres
Tunica intima– endothelium layer that lines the inside of the artery
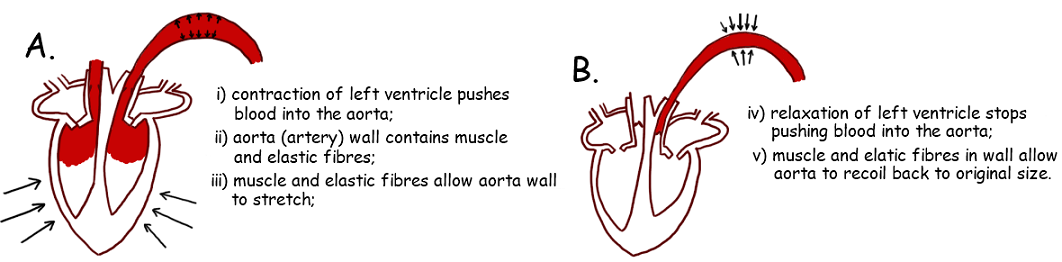
6.2.U3 The muscle and elastic fibres assist in maintaining blood pressure between pump cycles.
- Describe the mechanism used to maintain blood flow in arteries between heartbeats.
- Define systolic and diastolic blood pressure.
- Define vasoconstriction and vasodilation.
- The muscle fibres help to form a rigid arterial wall that is capable of withstanding the high blood pressure without rupturing. Muscle fibres can also contract to narrow the lumen, which increases the pressure between pumps and helps to maintain blood pressure throughout the cardiac cycle
- The elastic fibres allow the arterial wall to stretch and expand upon the flow of a pulse through the lumen. The pressure exerted on the arterial wall is returned to the blood when the artery returns to its normal size (elastic recoil). The elastic recoil helps to push the blood forward through the artery as well as maintain arterial pressure between pump cycles
When the ventricles of the heart contract (systole), the blood leaves the heart through the arteries at a very high pressure.
6.2.U4 Blood flows through tissues in capillaries. Capillaries have permeable walls that allow exchange of materials between cells in the tissue and the blood in the capillary.
- Describe the structure and function of capillaries.
- Describe the cause and effect of diffusion of blood plasma into and out of a capillary network.
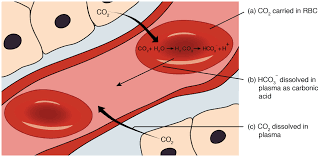
- Capillaries have a very narrow diameter (10 µm) with thin surrounding endothelium cells to allow the shortest distance for O2 to diffuse into the blood from the alveoli in the lungs and from the blood into the body tissues. CO2 also can easily diffuse out of the blood into the alveoli in the lungs and from the tissue into the blood after respiration.
- The walls have pores, making them very permeable allowing plasma to leak out and form tissue fluid, which contains oxygen, glucose and all other substances contained in the blood plasma, except proteins (too large to fit through the pores in the capillary wall)
- Highly branched networks of capillaries increase the surface area, maximizing the amount of nutrients and gases that can move in and out of the capillaries.
- Because they are highly branched, the blood slows down to allow efficient transfer of O2 and CO2 into and out of the capillaries.
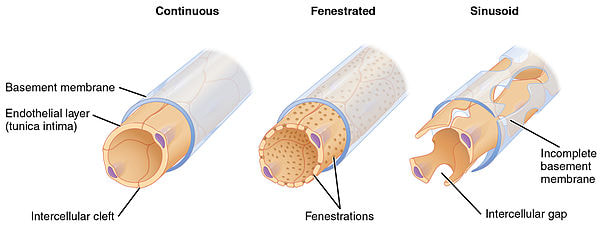
- Below are examples what capillaries look like. The pores or holes that allow certain substances to leave get larger from left to right, with Sinusoid capillaries having the largest openings. Specific names of these types of capillaries is not required.
Capillaries structure may vary depending on its location in the body and specific role:
- The capillary wall may be continuous with endothelial cells held together by tight junctions to limit permeability of large molecules
- In tissues specialised for absorption (e.g. intestines, kidneys), the capillary wall may be fenestrated (contains pores)
- Some capillaries are sinusoidal and have open spaces between cells and be permeable to large molcules and cells (e.g. in liver)
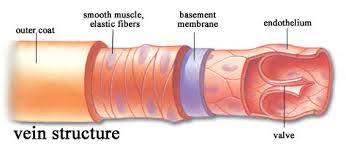
6.2.U5 Veins collect blood at low pressure from the tissues of the body and return it to the atria of the heart.
- State the function of veins.
- Outline the roles of gravity and skeletal muscle pressure in maintaining flow of blood through a vein.
- Transport blood back to the heart from the capillary beds in tissues.
- Very low blood pressure and therefore the walls can be thin. Blood is pushed back to the heart through the contraction of skeletal muscles. As the muscles contract, the veins are squeezed, pushing the blood back towards the heart
- Large lumen allows large amounts of blood to slowly return to the heart because the blood has to slow down as it passes through the capillary beds.
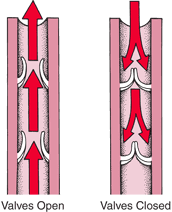
6.2.U6 Valves in veins and the heart ensure circulation of blood by preventing backflow.
- Outline the structure and function of a pocket valve.
- Valves are flaps of tissue that form pockets to prevent blood from flowing backwards in the wrong direction
- If the blood starts to flow backwards, it gets caught in the pocket valves causing that section of the vein to fill.
- When another contraction occurs and the blood starts to flow in the correct direction, the valves open allowing the blood to continue its movement towards the heart.
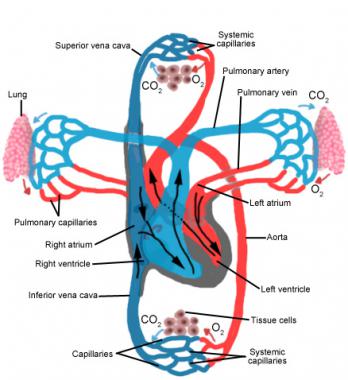
6.2.U7 There is a separate circulation for the lungs.
- Draw a diagram to illustrate the double circulation system in mammals.
- Compare the circulation of blood in fish to that of mammals.
- Explain the flow of blood through the pulmonary and systemic circulations.
- Explain why the mammalian heart must function as a double pump.
Pulmonary Circulation
- Blood flows from the right atrium into the right ventricle through the R.atrio-ventricular valve. The right atrium contracts right when the ventricle is almost full in order to push the rest of the blood into the ventricle.
- The right ventricle contracts sending the blood out of the ventricle (past a semi-lunar valve), through the pulmonary arteries to the lungs.
- The atrio-ventricular valve shuts preventing back flow into the atrium.
- The blood flows through capillaries obtaining oxygen from the lungs and returning to the heart by the pulmonary veins; which empty into the left atrium.
- This blood is actually returning to the heart from the lungs at the same time as the blood that returns to the right atrium from the rest of the body.
Systemic Circulation
- The blood then flows into the left ventricle through an L atrio-ventricular valve.
- The left ventricle contracts, sending the blood through another semi-lunar valve and out through the biggest artery in the body called the aorta.
- Again the atrio-ventricular valve shuts, preventing backflow into the atrium.
- The oxygenated blood flows to all the tissues and organs in the body to be used in aerobic respiration. (Arteries –> Arterioles –> Capillaries)
- Blood then flows from the capillaries to the numerous venules and then through the different veins in the body
- These will all eventually dump the blood into the inferior and superior vena cava
- Blood returns to the right atrium of the heart flowing from the inferior vena cava (blood from lower body) and the superior vena cava (blood coming upper body and head).
- Note: Both ventricles contract at the same time sending blood to the lungs and the other parts of the body.
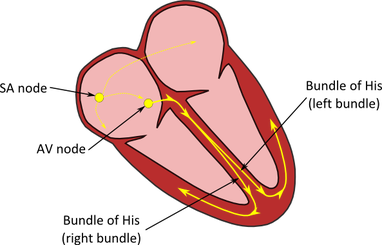
6.2.U8 The heartbeat is initiated by a group of specialized muscle cells in the right atrium called the sinoatrial node.
- Define myogenic contraction.
- Outline the role of cells in the sinoatrial node.
The contraction of the heart is myogenic. This means that the signal for cardiac compression arises within the heart tissue itself. In other words, the signal for a heartbeat is initiated by the heart muscle cells (cardiomyocytes) rather than from the brain:
- Membrane of the heart muscle cell depolarizes when the cell contracts, which then activates the adjacent cells so they contract
- Sinoatrial node: Group of small special muscle cells in the wall of the right atrium that beats at the fastest rate
- Cells have extensive membranes
- Sinoatrial node initiates each heartbeat because the cells depolarizes the first
6.2.U9 The sinoatrial node acts as a pacemaker.
- State the reason why the sinoatrial node is often called the pacemaker.
This cluster of cells are collectively called the sinoatrial node (SA node or SAN) sinoatrial node acts as a pacemaker. If defective, the sinoatrial node might be replaced by an artificial pacemaker
The electrical conduction of a heart beat occurs according to the following events:
- Sinoatrial node initiates a heartbeat by contracting and sending out an electrical signal that spreads through the walls of the atria.
- Electrical signal can spread because there are connections between adjacent fibers across which allows for the signal to be spread.
- The spread of the electrical signal causes the left and right atria to contract.
- After 0.1 seconds, electrical signal is passed to the ventricles
- Time delay allows for atria to pump blood into the ventricles
- Blood is then pumped from ventricles into the artery
- This second node – the atrioventricular node (AV node) – sends signals down the septum via a nerve bundle (Bundle of His).
- The Bundle of His innervates nerve fibres (Purkinje fibres) in the ventricular wall, causing ventricular contraction.
This sequence of events ensures there is a delay between atrial and ventricular contractions, resulting in two heart sounds – Lub Dub.
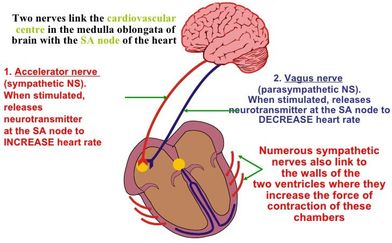
6.2.U11 The heart rate can be increased or decreased by impulses brought to the heart through two nerves from the medulla of the brain. (Oxford Biology Course Companion page 301)
- Outline the structures and functions of nervous tissue that can regulate heart rate.
- Describe factors that will increase heart rate.
- Describe factors that will decrease heart rate.
- The rate of the pacemaker can be affected by nerves connected to the medulla region of the brain.
- Low blood pressure, high levels of CO2 (low pH) and low levels of oxygen, stimulate the heart to increase its rate and therefore deliver more oxygen to the tissues and remove more carbon dioxide
- High blood pressure, low levels of CO2 (high pH) and high levels of oxygen, cause the heartrate to slow down.
- Cardiac nerves which are part of the sympathetic nervous system cause the heart rate to increase.
- The Vagus nerve that is part of the parasympathetic nervous system causes the heart rate to slow down
- The medulla of the brain controls most of the autonomic functions of the body such as breathing, heart rate and blood pressure.
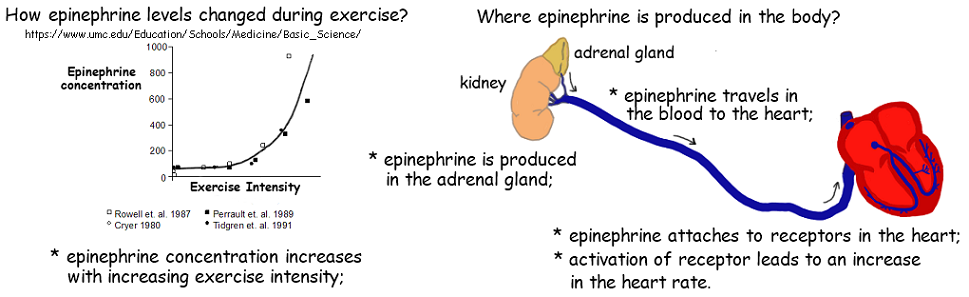
6.1.U12 Epinephrine increases the heart rate to prepare for vigorous physical activity
- Outline conditions that will lead to epinephrine secretion.
- Explain the effect of epinephrine on heart rate.
- Cardiac nerves also cause the release of norepinephrine (adrenalin) from the adrenal glands during strenuous physical activity or times of high levels of stress. This is also known as the fight or flight response
- The Vagus nerve causes the heart rate to slow down through the release of acetylcholine, which has an inhibitory action on the heartrate
6.2.A1 William Harvey’s discovery of the circulation of the blood with the heart acting as the pump.
- Outline William Harvey’s role in discovery of blood circulation.
6.2.A2 Pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle.
- Describe the cause and consequence of atherosclerosis.
- Outline the effect of a coronary occlusion on heart function.
Atrial Systole (0 to 0.1 s)
- Atria contract, pressure increases in the left and right atria, and the remaining blood is pumped into the ventricles (left atrium into left ventricle)
- Ventricle walls relaxed and therefore the pressure is low
- AV valves are open and semi-lunar valves are shut
Ventricular Systole (approx. 0.1 – 0.5 s)
- Ventricles contract and the pressure increases dramatically in the ventricles
- AV valves close (because of the pressure) preventing backflow and the semi-lunar valves open.
- Blood is pumped out of the left ventricle into the aorta through the left semi-lunar valve
- Pressure in the aorta increases
- Pressure falls in the atria
Atrial and Ventricular Diastole (approx. 0.5 to 0.8)
- Muscles in the walls of the ventricles and atria relax
- The semi-lunar valves close
- Since the pressure drops in the atria, blood flows into the left atrium from the pulmonary veins and into the right atrium via the vena cava
- AV valves also open as the pressure in the ventricles drops below the pressure in the atria and blood flows from the atria into the ventricles (left atrium into the left ventricle through the left AV valve)
- Pressure in the aorta drops but remains quite high throughout the cycle because of the elastic and muscle fibres in the walls
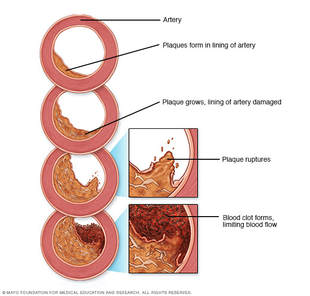
6.2.A3 Causes and consequences of occlusion of the coronary arteries.
- Explain the pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle.
- Explain the relationship between atrial and ventricular pressure and the opening and closing of heart valves.
- Explain the atrial, ventricular and arterial pressure changes as illustrated on a graph of pressure changes during the cardiac cycle.
- Identify the time of opening and closing of heart valves on a graph o f pressure changes during the cardiac cycle.
- Artery walls become damaged as fat (low-density lipoproteins) are deposited under the endothelium and fibrous tissue builds up
- Can result from a poor diet, over-eating, constant high blood glucose levels or smoking
- The flow of blood is impeded and the heart has to work harder to pump blood to the tissue, increasing blood pressure
- The smooth lining of the arteries begins to break down and form lesions called atherosclerotic plaques
- Platelets can bind to these lesions, causing an inflammatory response creating a blood clot
- The blood clot formed is called a thrombus and an embolus if it breaks free to travel through the bloodstream.
Consequences
- If an embolus breaks free, it can get stuck in a smaller arteriole and cause a blockage of blood supply to that tissue, eventually causing that tissue to die
- If this happens to the coronary arteries or arterioles in the heart, and enough of the tissue is deprived of oxygen, a myocardial infarction (heart attack) can occur
- If an embolus reaches the brain, and enough of the brain is deprived of oxygen and nutrients, a stroke can occur
- If coronary arteries are damaged, by-pass surgery can be performed, that takes an artery typically from a patient’s leg , replacing the damaged coronary artery
- Coronary Angioplasty (balloon angioplasty) can be an alternative to a by-pass operation. A catheter (with attached balloon) is inserted in the arm or the leg of a patient and is guided to the obstructed artery by x-ray and tv monitors
- A harmless dye is injected into the patient to determine exactly where is the blockage
- The balloon is inflated to reestablish blood flow stretching the arterial wall and squashing the plaques
6.2.S1 Identification of blood vessels as arteries, capillaries or veins from the structure of their walls. (Oxford Biology Course Companion page 294).
- Compare the diameter, relative wall thickness, lumen diameter, number of wall layers, abundance of muscle and elastic fibres and presence of valves in arteries, capillaries and veins.
- Given a micrograph, identify a blood vessel as an artery, capillary or vein.
6.2.S2 Recognition of the chambers and valves of the heart and the blood vessels connected to it in dissected hearts or in diagrams of heart structure.
- Label a diagram of the heart with the following structure names: superior vena cava, inferior vena cava, pulmonary semilunar valve, aorta, pulmonary artery, pulmonary veins, aortic semilunar valve, left atrioventricular valve, left ventricle, septum, right ventricle, left atrium, right atrium and right atrioventricular valve.
Body Fluids and Circulation
Table of Content
- Blood
- Blood Groups
- Coagulation of Blood
- Lymph
- Circulatory Pathways
- Human Circulatory System
- Cardiac Cycle
- Heart Sound
Blood
It is a fluid connective tissue consists of matrix, plasma and formed elements.
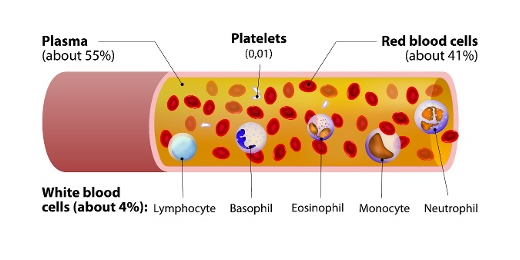
Fig. 1. Elements of the blood
Plasma
It is a straw colored, viscous fluid which constitutes about 55% of the blood plasma. The major proteins found in plasma are fibrinogen, globulins, and albumins. Fibrinogens functions during blood clotting. Albumins maintain osmotic balance in the body. Globulins are defensive in nature. Minerals such as Sodium Ions, Calcium Ions, Magnesium Ions, Bicarbonate Ions. Apart from this amino acid, glucose is also present in plasma.
Formed Elements
Formed Elements include erythrocytes, leucocytes, and blood platelets.
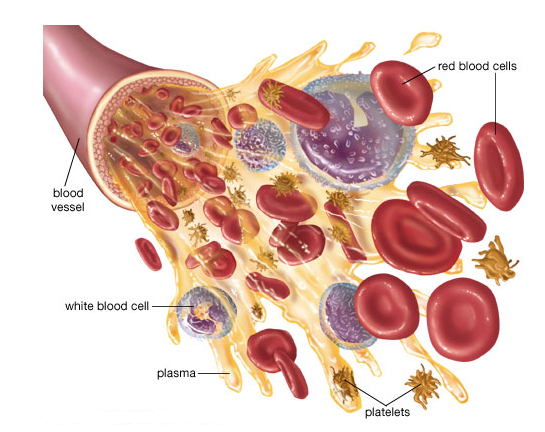
Fig. 2. Formed elements in blood
Erythrocytes also known as Red Blood Cells. They are the most abundant cells in the blood. They are formed in red bone marrow of adults. They are biconcave in shape and enucleated (without the nucleus). They carry iron containing protein known as Hemoglobin. Hemoglobin helps in the transport of oxygen and carbon-dioxide in blood. The average life span of RBCs is 120 days.
Leucocytes also known as White Blood Cells. They are nucleated cells which do not contain hemoglobin, so they appear colorless. They are of two types- granulocytes and agranulocytes.
Neutrophilsb, Basophils and Eosinophils are granulocytes. Lymphocytes and Monocytes are agranulocytes.
Neutrophils are known as Polymorphonuclear Leucocytes. Out of all the three granulocytes, neutrophils are most abundant. They are phagocytic cells.
Basophils are least in number in comparison to other granulocytes. They secrete serotonin, histamine, and basophils. So, basophils are involved in inflammatory reactions.
Eosinophils are involved in allergic reactions.
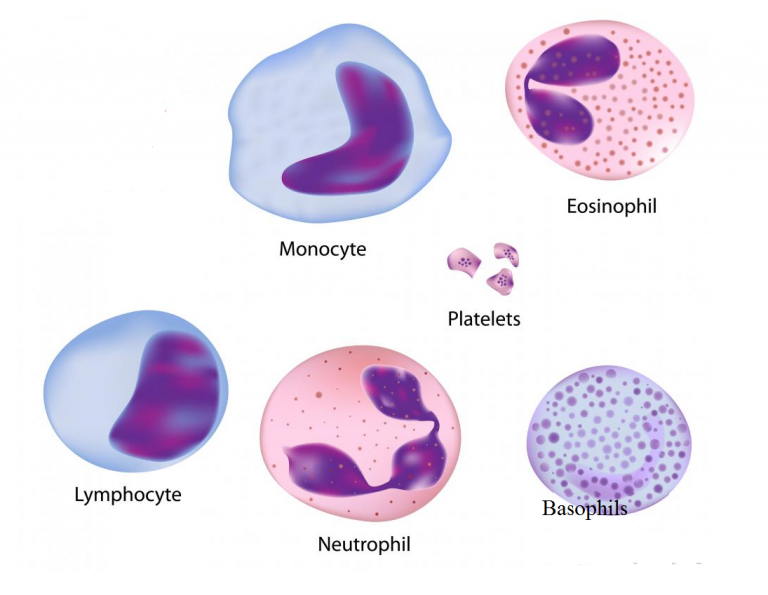
Fig. 3. White blood cells and platelets
Blood platelets are also known as Thrombocytes. They are involved in blood clotting. Decrease in the number of blood platelets can lead to loss of blood in the body.
Blood Groups
Blood grouping is divided into- ABO blood group and Rh group.
ABO blood grouping
ABO blood grouping is done based the presence or absence of certain antigens on the surface of RBCs. The antigen present on the surface of RBCs can be A or B. There are 4 types of blood group are A, B, AB and O group.

Fig. 4. Blood groups and antigen on red blood cells
The above table depicts blood groups and donor compatibility. As O blood group do not have any antigen on their surface, they are said to be universal donor whereas AB are considered universal recipients as they contain both the antigen of their surface. Blood transfusion is done only based on blood group of the donor and recipients.
Rh grouping
Rh is also an antigen like rhesus monkeys. Individuals having Rh antigen on RBCs are considered as Rh positive. Those which are without Rh antigen are considered Rh negative. If Rh -ve person receives Rh +ve blood, the Rh -ve individual will start producing antibodies against it. So, Rh group should also be tested at the time of blood transfusion.
An important case of Rh mismatching has been observed between the Rh -ve blood of a pregnant mother with Rh +ve blood of the fetus. Rh antigens of the fetus do not get exposed to the Rh-ve blood of the mother in the first pregnancy, due to placenta. But during the delivery of the first child, there is a possibility of mixing of the blood of mother with child.
In such cases, mother starts to produce antibodies against the Rh antigen. So, in the next pregnancy, the Rh antibodies from the Rh -ve mother can leak into the blood of the Rh +ve fetus and can destroy the fetal RBCs. This leads to agglutination of red blood cells. This condition is known as Erythroblastosis Foetalis. Fetus will anemic and suffers from jaundice. This can be avoided by injecting anti-Rh antibodies to the mother instantly after the delivery of the first child.
Coagulation of Blood
Blood coagulation is also known as Blood Clotting. Blood responds by clotting or coagulation after any injury or trauma. This helps in preventing excess loss of blood. When we get injured, after some time reddish brown scum is formed at the site of injury. This is known as clot which is made up of network of threads known as Fibrils. This network contains dead and damaged formed elements of blood. Fibrils are formed from the conversion of inactive fibrinogen in presence of enzyme thrombin. Thrombin is also formed from inactive form known as Prothrombin. Thrombokinase is required for the conversion of prothrombin into thrombin.
Platelets release certain factors to begin blood clotting. Calcium ions play an important role duriBlood coagulationclotting.
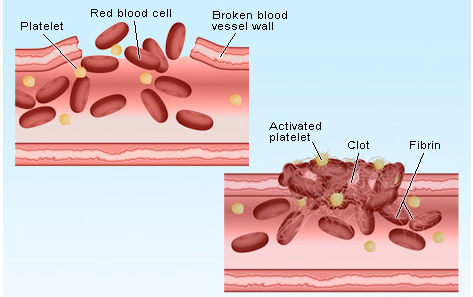
Fig. 5. Blood coagulation
Lymph
Blood circulates in blood capillaries in tissues. Some water along with some water-soluble substances leak out and enter the interstitial space. This is known as Tissue Fluid or Interstitial Fluid. Exchange of gases, nutrients between the blood and the cells occurs through this fluid.
A network of vessels that collects this fluid and drain it to major veins is known as Lymphatic System. Lymphatic system contains a fluid known as Lymph. Lymphocytes which are an important cell of the immune system are present in lymph.
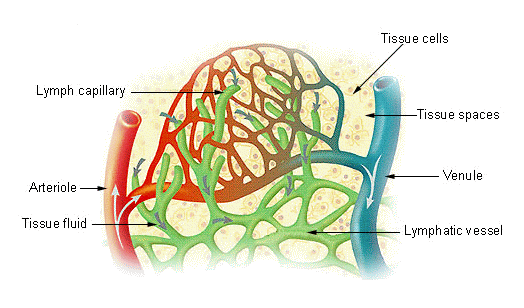
Fig. 6. Lymph
Circulatory Pathways
There are two types of circulatory system- Open Circulatory System and Closed Circulatory System.
When blood flow in open spaces known as Lacunae and Sinuses, it is known as Open Circulatory System it is present in molluscs, arthropods, etc.
When blood flow in closed vessels it is known as Closed Circulatory System. For Example, humans. Closed circulatory possess an advantage over open circulatory system, as blood can flow in a regulated manner in case of closed circulatory system.
Vertebrates have muscular, pumping organ known as Heart. Fishes have 2 chambered heart. Amphibians have 3 chambered heart except crocodiles (4 chambered heart). Birds, reptiles, and humans have 4 chambered heart.
Human Circulatory System
It includes heart, vessels, and blood. Heart is mesodermal in nature. It is located in the thoracic cavity, in between the two lungs.
The double membrane that surrounds the heart is known as Pericardium. Pericardium encloses the pericardial fluid. Heart is 4 chambers with 2 atria and 2 ventricles. A thin wall separates the left and the right atria is known as Intra-atrial Septum whereas left and right ventricle are separated by thick intra-ventricular septum.
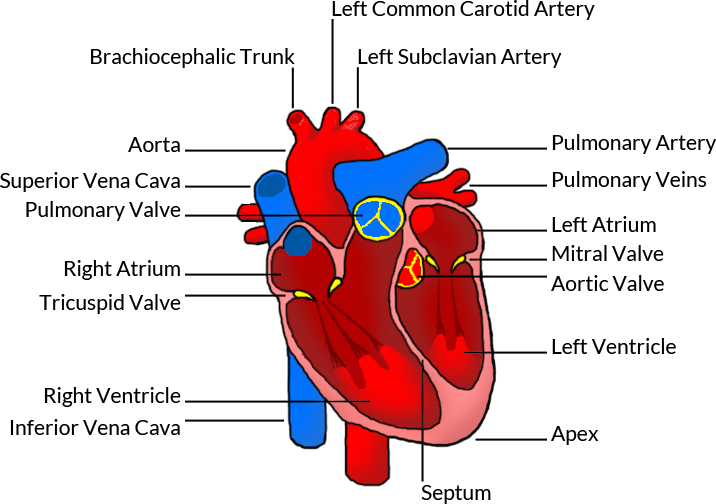
Fig. 7. Human heart
The opening between the right atrium and the right ventricle is guarded by a valve known as Tricuspid Valve, whereas a bicuspid or mitral valve guards the opening between the left atrium and the left ventricle. The openings of the right and the left ventricles into the pulmonary artery and the aorta respectively are provided with the semilunar valves. Valves in the heart allows the blood to flow in one direction and thus preventing backflow of blood.
Heart is a muscular organ and the muscles of the heart are known as cardiac muscles. A specialized cardiac musculature called the nodal tissue is also dispersed in the heart. One which is present in the upper right corner of the right atrium is known as Sinoatrial Node or SA Node. Another tissue is present in the upper left corner of the right atrium is known as Atrio-Ventricular Node or AV Node.
A bundle of nodal fibres, Atrioventricular Bundle (AV Bundle) continues from the AVN which passes through the atrio-ventricular septa and divides into a right and left bundle. These branches give rise to minute fibers known as Purkinje Fibers. SA node has the ability to get excited and generates the action potential. So, SA node is known as the Pacemaker of the Heart.
Cardiac Cycle
Sequence of electrical and mechanical events during every heart beat is known as Cardiac Cycle. It is divided into two phases – Diastole and Systole. During diastole heart ventricles relaxes due to which it is filled with blood. During systole, ventricles contract to pump the blood into the arteries.
Phases of Cardiac Cycle are as follows:
Atrial Systole includes contraction of the left and the right atria followed by electrical stimulation. This increases blood pressure in the both left and right atria. This allows blood to pump into the ventricles. During this AV valves are open and semilunar valves are closed. It takes about 0.1 seconds.
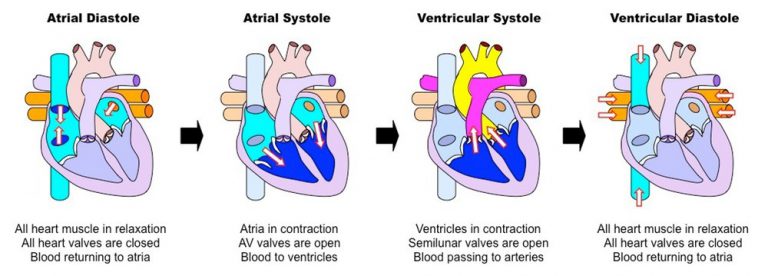
Fig. 8. Cardiac cycle
Ventricular Systole includes contraction of the left and right ventricles which is followed by electrical stimulation. During this AV valves are closed and semilunar valves are open. It takes about 0.3 seconds.
Cardiac diastole is a period when heart relaxes to fill the blood. When atria and ventricles are relaxing together, they form complete cardiac diastole. During ventricular diastole, pressure in the ventricles drops below the left atrial pressure, mitral valve opens and left ventricle gets filled with the blood. Similarly, when the pressure in the right ventricle drops below that in the right atrium, the tricuspid valve opens, and the right ventricle gets filled with blood. During diastole, the pressure within the left ventricle is lower than that in aorta, which allows the blood to circulate in the heart itself with the help of the coronary arteries.
Heart Sound
The heart sound is known as “lubb-dubb” sound. The first heart sound lubb is produced when mitral and tricuspid valves gets closed at the beginning of the ventricular systole. The second sound dubb is produced when aortic and pulmonary valves gets closed at the end of ventricular systole.
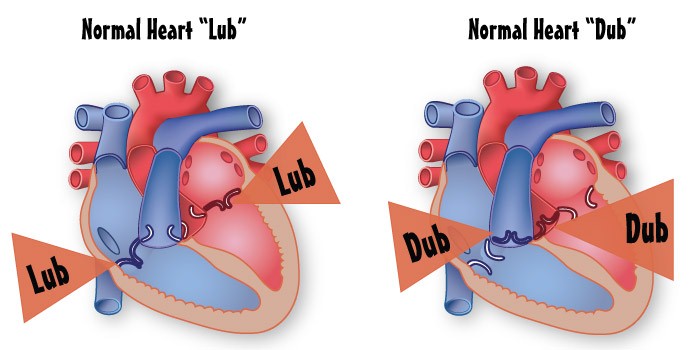
Fig. 9. Heart sound