- IB Style Question Banks with Solution
- IB DP Biology SL- IB Style Practice Questions with Answer-Topic Wise-Paper 1
- IB DP Biology HL- IB Style Practice Questions with Answer-Topic Wise-Paper 1
- IB DP Biology SL- IB Style Practice Questions with Answer-Topic Wise-Paper 2
- IB DP Biology HL- IB Style Practice Questions with Answer-Topic Wise-Paper 2
6.6 Hormones, Homeostasis and Reproduction
Essential Idea:
Hormones are used when signals need to be widely distributed
Understandings:
- Insulin and glucagon are secreted by β and α cells of the pancreas respectively to control blood glucose concentration
- Thyroxin is secreted by the thyroid gland to regulate the metabolic rate and help control body temperature
- Leptin is secreted by cells in adipose tissue and act on the hypothalamus of the brain to inhibit appetite
- Melatonin is secreted by the pineal gland to control circadian rhythms
- A gene on the Y chromosome causes embryonic gonads to develop as testes and secrete testosterone
- Testosterone causes pre-natal development of male genitalia and both sperm production and development of male secondary sexual characteristics during puberty
- Estrogen and progesterone cause pre-natal development of female reproductive organs and female secondary sexual characteristics during puberty
- The menstrual cycle is controlled by negative and positive feedback mechanisms involving ovarian and pituitary hormones
Applications:
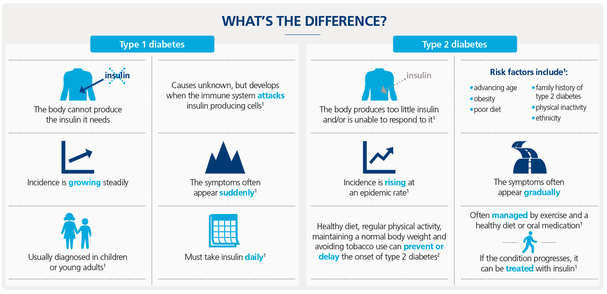
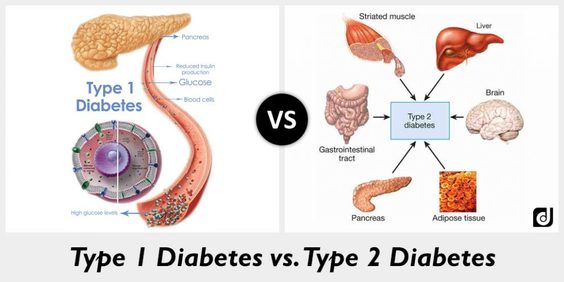
- Causes and treatment of Type I and Type II diabetes
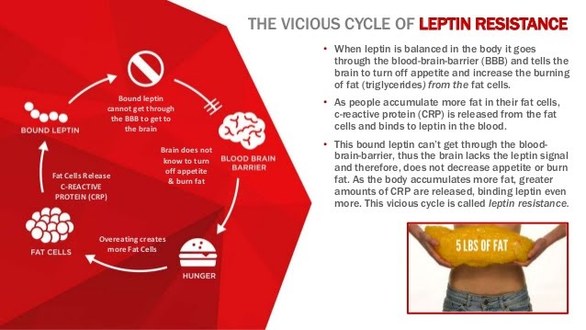
- Testing of leptin on patients with clinical obesity and reasons for the failure to control the disease
- Causes of jet lag and use of melatonin to alleviate it
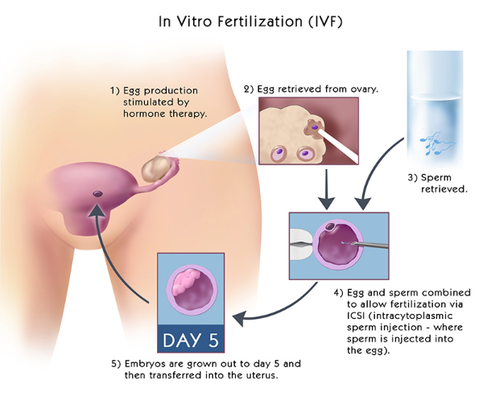
- The use in IVF of drugs to suspend the normal secretion of hormones, followed by the use of artificial doses of hormones to induce superovulation and establish a pregnancy
- William Harvey’s investigation of sexual reproduction in deer
Skills:
- Annotate diagrams of the male and female reproductive system to show names of structures and their functions
- Explain the control of blood glucose concentration, including the roles of glucagon, insulin and the alpha and beta cells in the pancreatic islets.
- Describe the structure and function of thyroxin.
- Outline thyroxin’s role in body temperature regulation.
- List symptoms of thyroxin deficiency.
- State that leptin is a protein hormone.
- Outline the mechanism of action of leptin.
- Describe the role and discovery of the ob allele in obese mice.
- Define circadian rhythm.
- Describe the secretion and action of melatonin.
- Outline the mechanism that regulates melatonin secretion in response to the day-night cycle.
- Describe the mechanism by which the SRY gene regulates embryonic gonad development.
- Outline role of testosterone in prenatal development of male genitalia.
- State testosterone’s role in stimulating the primary sexual characteristic of males.
- List secondary sexual characteristics triggered by testosterone at puberty.
- State the sources of estrogen and progesterone used in embryonic development.
- Describe prenatal development of female reproductive organs.
- List secondary sexual characteristics triggered by estrogen and progesterone at puberty.
- Outline events occurring during the follicular and luteal phases of the menstrual cycle.
- State the source and location of action of hormones in the menstrual cycle, including FSH (follicle stimulating hormone), LH (luteinising hormone), estrogen and progesterone.
- Outline the role of hormones in the menstrual cycle, including FSH (follicle stimulating hormone), LH (luteinising hormone), estrogen and progesterone.
- Describe the negative feedback loops that regulates secretion of FSH.
- Describe the positive feedback loop that regulates secretion of estrogen.
- Annotate a graph showing hormone levels in the menstrual cycle, illustrating the relationship between changes in hormone levels and follicular development, ovulation, changes to the corpus luteum, menstruation and the thickening of the endometrium.
- Distinguish between causes of type I and type II diabetes.
- Distinguish between treatment of type I and type II diabetes.
- Explain the double blind study that tested the effect of leptin treatment on human obesity.
- Outline role of leptin resistance in human obesity.
- State symptoms of jet lag.
- Outline the biological cause of jet lag.
- Describe use of melatonin in treatment for jet lag.
- Define in vitro fertilization.
- Outline the process of in vitro fertilisation including down-regulation, superovulation, harvesting, fertilization and implantation.
- Outline Harvey’s methods of studying reproduction.
- State Harvey’s discovery about reproduction.
- Label a diagram of the male reproductive system, including the bladder, sperm duct, penis (with foreskin and erectile tissue), urethra, testis, scrotum, epididymis, prostate gland and seminal vesicle.
- Outline the function of the following male reproductive structures: testis, scrotum, epididymis, sperm duct, seminal vesicle, prostate gland, urethra and penis.
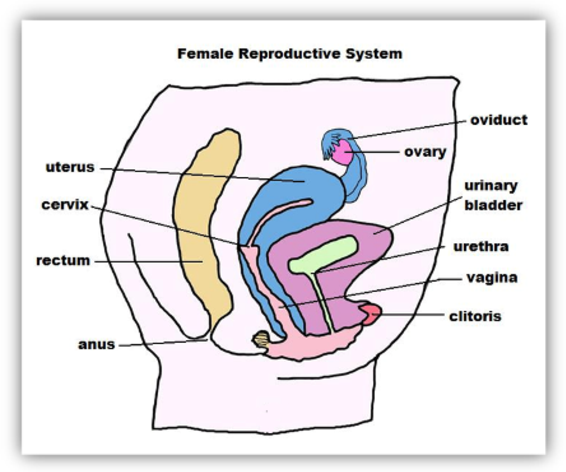
- Label a diagram of the female reproductive system, including the ovary, uterus, bladder, urethra, vulva, vagina, cervix and oviduct.
- Outline the function of the following female reproductive structures: ovary, oviduct, uterus, cervix, vagina, and vulva.
- Describe what Harvey was and was not able to observe in his reproduction research given the tools available at the time.
Topic 6.6: Hormones, Homeostasis and reproduction
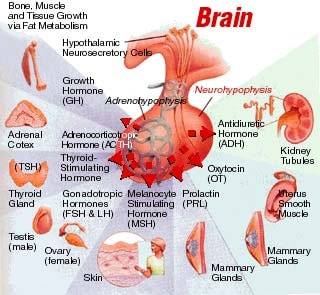
In the unit of Hormones, Homeostasis and Reproduction we will learn how the internal environment of the body must remain constant despite changes that occur in the external environment. Hormones are used in feedback mechanism to help control this environment. We will look at how these hormones can control blood glucose, our metabolic rate, our body temperature, our appetite and sleep cycles. We will also look at how hormones are used in reproduction.
This unit will last 4 school days.
Essential idea:
- Hormones are used when signals need to be widely distributed. 6.6
Nature of science:
- Developments in scientific research follow improvements in apparatus—William Harvey was hampered in his observational research into reproduction by lack of equipment. The microscope was invented 17 years after his death. (1.8)
- Describe what Harvey was and was not able to observe in his reproduction research given the tools available at the time.
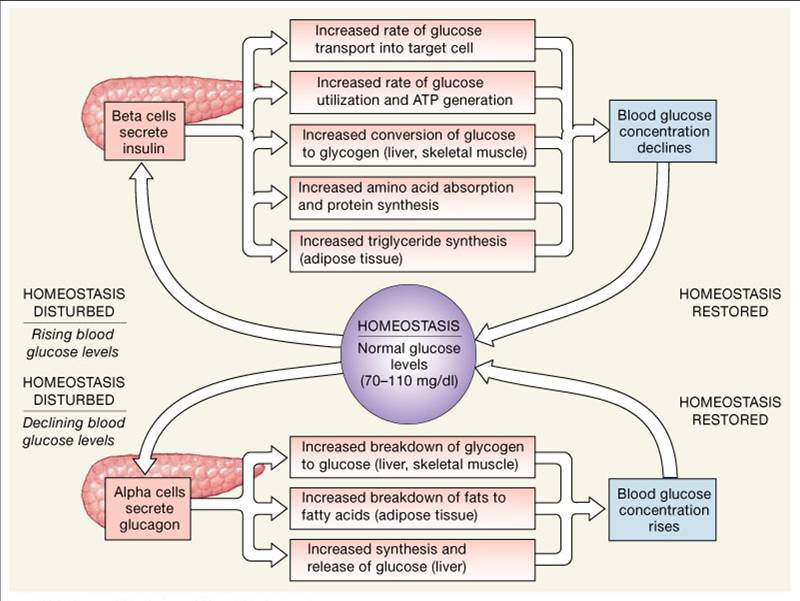
6.6.U1 Insulin and glucagon are secreted by β and α cells of the pancreas respectively to control blood glucose concentration.
- Explain the control of blood glucose concentration, including the roles of glucagon, insulin and the alpha and beta cells in the pancreatic islets.
The body needs glucose to make ATP (via cell respiration), however the amount required will fluctuate according to demand. High levels of glucose in the blood can damage cells (creates hypertonicity) and hence glucose levels must be regulated
- Blood glucose concentration is carefully monitored by negative feedback mechanisms.
- Cellular respiration is constantly lowering blood glucose levels.
- Receptors in the pancreas sense when the blood glucose level is too low.
- Alpha (α) cells in the islets of Langerhans in the pancreas secrete glucagon into the bloodstream.
- Glucagon stimulates the liver to breakdown stored glycogen into glucose which is released into the bloodstream.
- Blood glucose levels rise back to their normal limits.
- After a person eats, digestion breaks large carbohydrates into glucose molecules.
- Glucose levels rise in the blood.
- If the glucose levels get too high, receptors sense the increased glucose levels causing the pancreas to secrete insulin by the Beta cells (β) of the islets Langerhans.
- Insulin stimulates the absorption of glucose from the blood into skeletal muscles and fat tissue, and thus allowing the liver to convert glucose into glycogen (animal carbohydrate storage molecule).
- Glucose levels decrease back to the normal range.
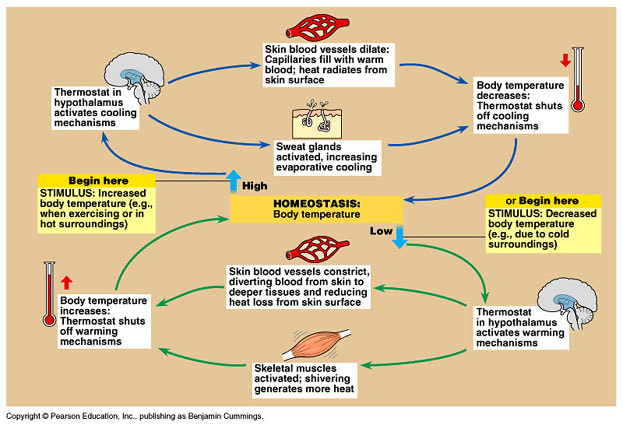
6.6.U2 Thyroxin is secreted by the thyroid gland to regulate the metabolic rate and help control body temperature.
- Describe the structure and function of thyroxin.
- Outline thyroxin’s role in body temperature regulation.
- List symptoms of thyroxin deficiency.
Thyroxin is a hormone secreted by the thyroid gland of the endocrine system
- Thyroxin contains iodine; therefore, prolonged deficiency to iodine in the diet prevents the production of thyroxin
- Thyroxin is important in the regulation of the body’s metabolic rate
- The body’s metabolic rate is the amount of energy a body uses at rest; combination of the catabolic and anabolic reactions
- Since thyroxin causes an increase in the body’s metabolic rate, there is an increase in oxygen consumption and the hydrolysis of ATP; thereby causing an increase in the body’s temperature
- Increase in thyroxin stimulates the breakdown of lipids and the oxidation of fatty acids
- Thyroxin also stimulates carbohydrate metabolism, including the uptake of glucose and the breakdown of glycogen into free glucose
- In a regular person, if the bodies temperature drops, a release in thyroxin will stimulate heat production causing the body’s temperature to rise
- If there is an excessive amount of thyroxin in the body, hyperthyroidism can occur
- If there is an insufficient amount of thyroxin in the body, hypothyroidism can occur
- Some of the symptoms of hypothyroidism are weight gain, loss of energy, feeling cold all the time, forgetfulness and depression
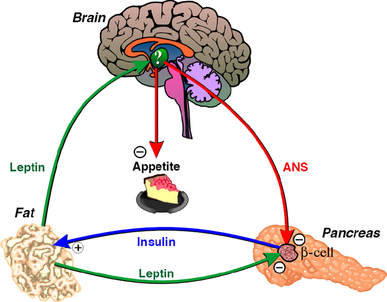
6.6.U3 Leptin is secreted by cells in adipose tissue and acts on the hypothalamus of the brain to inhibit appetite.
- State that leptin is a protein hormone.
- Outline the mechanism of action of leptin.
- Describe the role and discovery of the ob allele in obese mice
If the amount of adipose tissue in an individual increases, then their concentrations of leptin also increases, leading to long term suppression of appetite and reduced food intake
In obese individuals a decreased sensitivity to leptin can occur, resulting in an inability the recognize when they are full
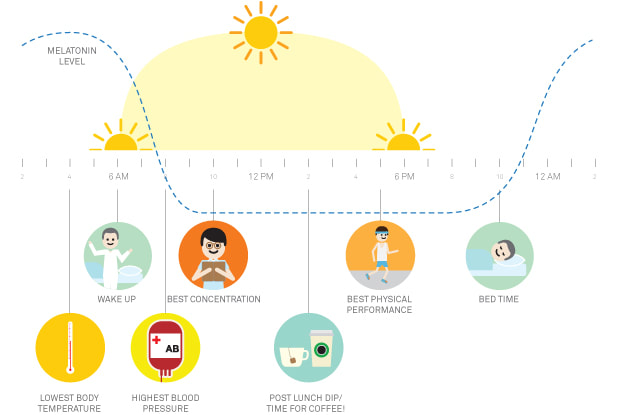
6.6.U4 Melatonin is secreted by the pineal gland to control circadian rhythms.
- Define circadian rhythm.
- Describe the secretion and action of melatonin.
- Outline the mechanism that regulates melatonin secretion in response to the day-night cycle.
Melatonin is a hormone produced by the pineal gland within the brain in response to changes in light
- The secretion of melatonin by the pineal gland is controlled by cells in the hypothalamus
- Light exposure to the retina is relayed to the suprachiasmatic nucleus (SCN) of the hypothalamus. These fibers from the hypothalamus relay a message to the nerve ganglia of the spinal cord which is relayed back to the pineal gland to release melatonin.
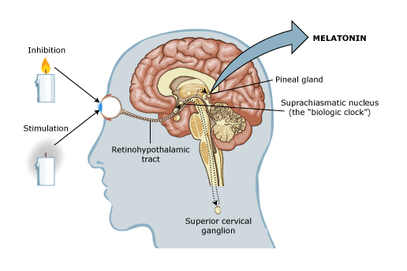
- Melatonin helps control your sleep and wake cycles (circadian rhythms).
- Very small amounts of melatonin are found in foods such as meats, grains, fruits, and vegetables.
- An internal 24- hour clock controls your natural cycle of sleeping and waking hours.
- Melatonin levels generally begin to rise in the mid to late evening, remaining high for most of the night, and then drop in the early morning hours.
- Light from the sun can also affect how much melatonin your body produces. During the shorter days of the winter months, your body may produce melatonin either earlier or later in the day than usual. This change can lead to symptoms of seasonal affective disorder (SAD), or winter depression.
- Natural melatonin levels slowly drop with age. Some older adults make very small amounts of it or none at all.
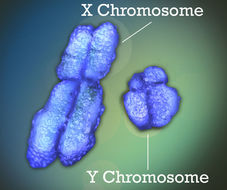
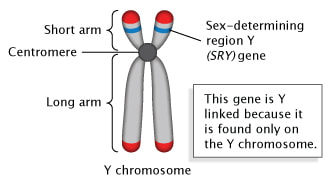
6.6.U5 A gene on the Y chromosome causes embryonic gonads to develop as testes and secrete testosterone.
- Describe the mechanism by which the SRY gene regulates embryonic gonad development.
Humans have 46 chromosomes in all diploid somatic cells – 22 pairs are autosomes and the 23rd pair are the sex chromosomes.
- Females possess two copies of the X chromosome (XX), while males possess one X and a shorter Y chromosome (XY)
- The Y chromosome (small one below) has a gene called the SRY gene that causes the embryonic gonads to become testes and begin secreting testosterone
- SRY codes for a protein called TDF (testis-determining factor) that stimulates the expression of other genes located on the Y chromosome that cause testis development
- If there are two X chromosomes, the gonads develop as ovaries
 |  |
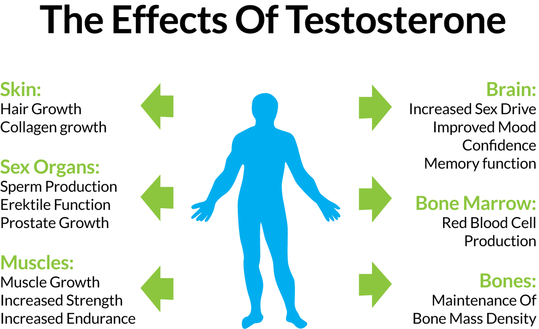
6.6.U6 Testosterone causes pre-natal development of male genitalia and both sperm production and development of male secondary sexual characteristics during puberty.
- Outline role of testosterone in prenatal development of male genitalia.
- State testosterone’s role in stimulating the primary sexual characteristic of males.
- List secondary sexual characteristics triggered by testosterone at puberty.
The main male reproductive hormone is testosterone, which is secreted by the testes and serves a number of roles:
- Secreted in the testes of males or the early stage testosterone-secreting cells that will become testes.
- Aid in the development and maturation of the male genitalia as a fetus at about the 8th to 9th week.
- During puberty, testosterone aids in the development of male secondary sexual characteristics such as pubic and facial hair, enlarged penis, broad shoulders, muscle mass, deepening of voice and bone density.
- Stimulates production of sperm and promotes the male libido (sex drive).
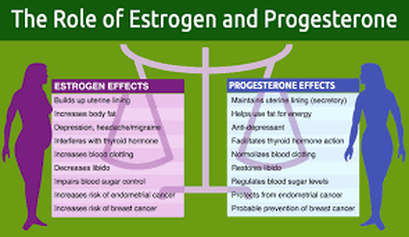
6.6.U7 Estrogen and progesterone cause pre-natal development of female reproductive organs and female secondary sexual characteristics during puberty.
- State the sources of estrogen and progesterone used in embryonic development.
- Describe prenatal development of female reproductive organs.
- List secondary sexual characteristics triggered by estrogen and progesterone at puberty.
The main female reproductive hormones (secreted by the ovaries) are estrogen and progesterone, which serve several roles:
- If the SRY gene on the Y chromosome is not present in the embryo, the gonads develop into ovaries
- Estrogen and progesterone which are secreted by the mother’s ovaries and then by the placenta, will cause the female reproductive organs to develop in the absence of testosterone
- During puberty, estrogen and progesterone cause the development of secondary sexual characteristics in females, including breast development, menstrual cycle and pubic and armpit hair
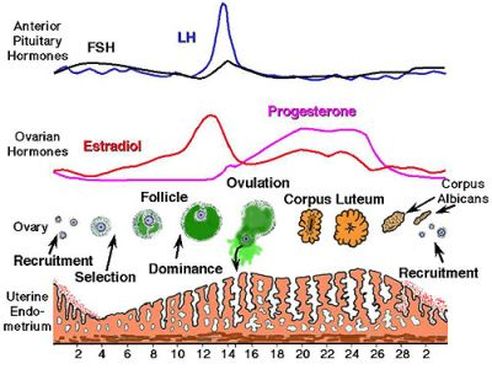
6.6.U8 The menstrual cycle is controlled by negative and positive feedback mechanisms involving ovarian and pituitary hormones [The roles of FSH, LH, estrogen and progesterone in the menstrual cycle are expected.]
- Outline events occurring during the follicular and luteal phases of the menstrual cycle.
- State the source and location of action of hormones in the menstrual cycle, including FSH (follicle stimulating hormone), LH (luteinising hormone), estrogen and progesterone.
- Outline the role of hormones in the menstrual cycle, including FSH (follicle stimulating hormone), LH (luteinising hormone), estrogen and progesterone.
- Describe the negative feedback loops that regulates secretion of FSH.
- Describe the positive feedback loop that regulates secretion of estrogen.
- Annotate a graph showing hormone levels in the menstrual cycle, illustrating the relationship between changes in hormone levels and follicular development, ovulation, changes to the corpus luteum, menstruation and the thickening of the endometrium.
The menstrual cycle describes recurring changes that occur within the female reproductive system to make pregnancy possible
FSH (Follicle stimulating hormone)
- Produced and secreted by the anterior pituitary gland.
- Stimulates the growth of the follicles in the ovaries to create a mature Graafian follicle.
- Promotes the thickening of the follicle wall.
- Stimulates the secretion of the hormone estrogen.
LH (luteinizing hormone)
- Produced and secreted by the anterior pituitary gland.
- Triggers the release of the egg (ovulation).
- Stimulates the growth of the corpus luteum (secretes estrogen and progesterone).
- Stimulates the secretion of hormone estrogen and progesterone.
Estrogen
- Produced by the developing follicles in the ovaries and the corpus luteum.
- Promotes the thickening of the uterine wall (endometrium) and the growth of blood vessels, in preparation of egg implantation.
- Inhibits FSH and LH when the estrogen levels are high (around same time as ovulation). This would prevent the development and release of another egg.
Progesterone
- Produced by the ovaries and the corpus luteum.
- Helps maintain the thickening of the uterine wall for egg implantation.
- Inhibit the production of FSH and LH.
6.6.A1 Causes and treatment of Type I and Type II diabetes.
- Distinguish between causes of type I and type II diabetes.
- Distinguish between treatment of type I and type II diabetes.
6.6.A2 Testing of leptin on patients with clinical obesity and reasons for the failure to control the disease.
- Explain the double blind study that tested the effect of leptin treatment on human obesity.
- Outline role of leptin resistance in human obesity.
Since most humans have quite a high leptin concentration, it was determined that the many of obesity cases where caused by a change in the receptor protein for leptin, not in the production of leptin. A double blind study was conducted by the biotech company Amgen, showed that injections of leptin to many of these individuals, since their receptors didn’t work, failed to control obesity. In individuals that experienced weight loss, there was a big discrepancy in the amount of weight that was lost. There also were other side effects such as skin irritation and swelling.
6.6.A3 Causes of jet lag and use of melatonin to alleviate it.
- State symptoms of jet lag.
- Outline the biological cause of jet lag.
- Describe use of melatonin in treatment for jet lag.
The SCN of the hypothalamus and the pineal gland continual set the circadian rhythm of the place the person is departing from. Therefore, when a person lands in a country that is many time zones different than the origin, they feel sleepy in the day and awake at night
Jet lag will only last a few days, as the body adjusts to the new times when the light is detected by the cells in the retina during a different time period
6.6.A4 The use in IVF of drugs to suspend the normal secretion of hormones, followed by the use of artificial doses of hormones to induce superovulation and establish a pregnancy.
- Define in vitro fertilization.
- Outline the process of in vitro fertilisation including down-regulation, superovulation, harvesting, fertilization and implantation.
IVF is the process of fertilization by extracting eggs, retrieving a sperm sample, and then manually combining an egg and sperm in a laboratory dish. The embryo(s) is then transferred to the uterus
- Generally, IVF treatment begins by taking drugs to halt the regular secretion of the hormones FSH and LH. This in turn stops the secretion of progesterone and estrogen and effectively allows the doctor to take control of the timing and egg production of the woman’s ovaries
- The woman is then injected with large amounts of FSH to induce the production of many Graafian follicles.
- LH is also injected to promote the release of many ovules (eggs)
- This is called superovulation, which can produce between 10 and 20 eggs
- The eggs are then stimulated to mature by an injections of HCG (Human Chorionic Gonadotrophin), a hormone usually secreted by the developing embryo
- The eggs are surgically removed from the ovary of the woman.
- Sperm is collected from the male individual.
- Many sperm (50,000-100,000) are mixed with the eggs in a petri dish.
- The sperm and eggs in the petri dish are incubated at 37ºC (body temperature).
- The eggs are analyzed for successful fertilization (two nuclei inside the egg).
- Healthy embryos are selected and are transferred into the female uterus for implantation (up to 3 healthy embryos are transferred into the uterus to increase chance of implantation).
6.6.A5 William Harvey’s investigation of sexual reproduction in deer. [William Harvey failed to solve the mystery of sexual reproduction because effective microscopes were not available when he was working, so fusion of gametes and subsequent embryo development remained undiscovered.]
- Outline Harvey’s methods of studying reproduction.
- State Harvey’s discovery about reproduction.
William Harvey was best known for his discovery of the circulation of the blood, also was interested in sexual reproduction and how life is formed.
Aristotle’s theory was called the seed and soil theory, which stated that the male produces a seed (sperm) which then forms an egg when it mixes with menstrual blood of the mother. The egg then develops into a fetus inside the mother and eventually “voila” you have a baby
Harvey studied the uterus of the deer during mating season by killing them and then dissecting them expecting to find eggs; however, Harvey only found signs of fetal development 2 to 3 months after mating season. He concluded that Aristotle’s theory of seed and soil was incorrect, but then he was also incorrect in stating that the fetus doesn’t come from the mixture of the male and female seeds. He knew he had not come up with the correct method of sexual reproduction
6.6.S1 Annotate diagrams of the male and female reproductive system to show names of structures and their functions.
- Label a diagram of the male reproductive system, including the bladder, sperm duct, penis (with foreskin and erectile tissue), urethra, testis, scrotum, epididymis, prostate gland and seminal vesicle.
- Outline the function of the following male reproductive structures: testis, scrotum, epididymis, sperm duct, seminal vesicle, prostate gland, urethra and penis.
- Label a diagram of the female reproductive system, including the ovary, uterus, bladder, urethra, vulva, vagina, cervix and oviduct.
- Outline the function of the following female reproductive structures: ovary, oviduct, uterus, cervix, vagina, and vulva.
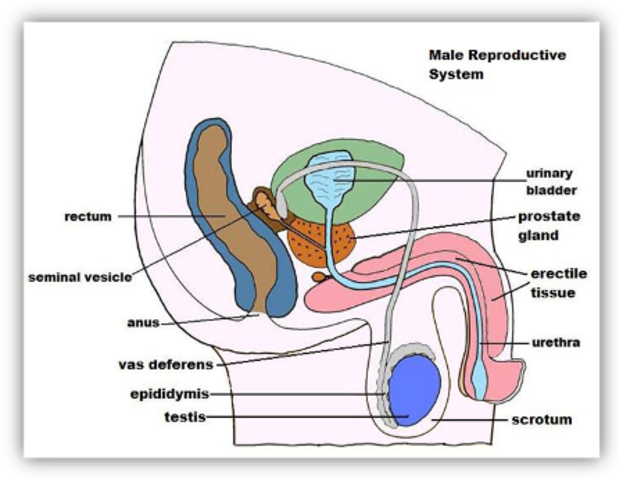 |  |
Human Reproduction
Table of Content
- Male Reproductive System
- Female Reproductive System
- Gametogenesis
- Spermatogenesis
- Oogenesis
- Menstrual Cycle
- Fertilization and Implantation
Humans are sexually reproducing animals. Human reproduction includes following processes:
- Formation of male and female gametes. This process is known as gametogenesis.
- Transfer of male gamete to female genital tract.
- Fusion of male and female gamete to form zygote. This process is known as fertilization.
- Attachment of zygote in the uterine wall. This is known as implantation.
- Embryo development.
- Parturition (delivery of baby outside the female body).
Male Reproductive System
It is in the pelvis region of the male body. Male reproductive system comprises of- a pair of testis, glands, accessary ducts, and male genitalia. The testis is located outside the abdominal cavity in a pouch-like structure known as scrotum. This location of testis is essential for proper development of sperms (male gamete) inside the testis. It helps to maintain a lower temperature than the body temperature needed for gametogenesis or spermatogenesis. Testis is divided into compartments known as testicular lobules.
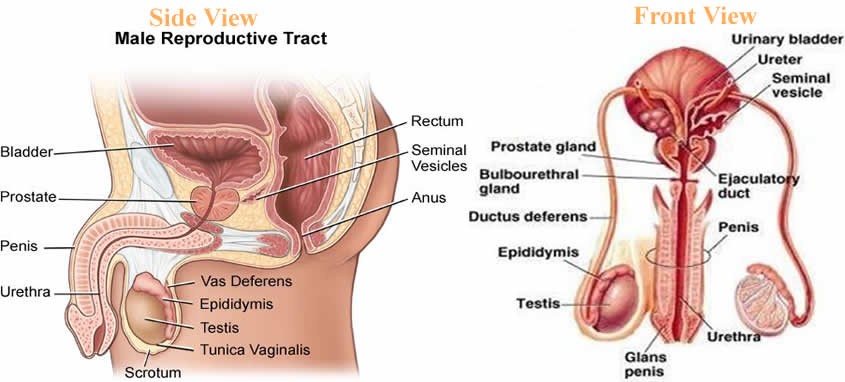
Fig.1. Parts of Male Reproductive System
Each testicular lobule consists of highly coiled structure known as seminiferous tubules. These are the site for sperm formation. Seminiferous tubules are lined by two types of cells known as- spermatogonia and sertoli cells. Spermatagonia also known as germ cells, give rise to sperms, the male gamete. Spermatogonia are diploid cells and they undergo meiosis to form sperms. Sertoli cells are elongated cells which nourishes the growing sperms. Outside the seminiferous tubule, the interstitial space contains cells known as leydig cells. Ledig cells are involved in synthesis of testicular hormone known as testosterone. Testosterone hormone is involved in development of secondary sexual characteristics such as moustaches and beard.
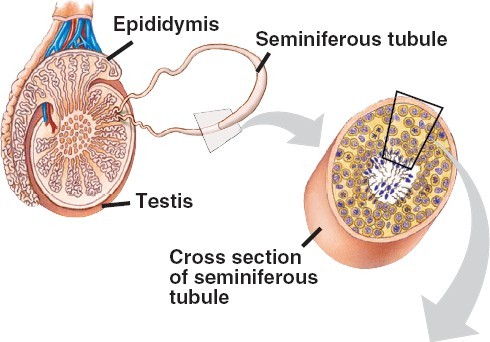
Fig.2. Section view of Seminiferous Tubule
Apart from these, male reproductive system consists of certain accessory ducts such as rete testis, vasa efferentia, epididymis and vas deferens. Rete testis are the network of tubules which are located in the hilum of the testis. It is a site where sperms are concentrated. Loss of this process leads to infertility.
Vasa efferentia are the small ducts that carry semen from the testis to the epididymis. It passes sperms to vas deferens. Vas deferens opens into urethra as the ejaculatory duct. The male external genitalia are known as penis. It facilitates insemination, that is, transfer of sperms to the female genitalia.
Male accessory glands include- prostate glands, seminal vesicle, and bulbourethral glands.
Seminal vesicles are paired glands that opens into the vas deferens near the junction with the urethra. Its secretion forms the part of semen. Semen is the fluid containing spermatozoa or sperm. The fluid of seminal vesicle is alkaline in nature. This alkaline nature helps in neutralization of alkalinity of the female vagina during insemination.
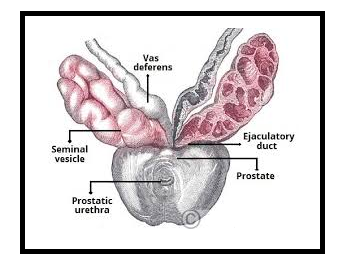
Fig.3. Accessory Glands
Prostate glands are in the neck of the urinary bladder. They secrete the fluid that makes up the semen and functions in nourishment as well as protection of the sperms.
Bulbourethral glands also known as Cowper’s glands. They are located inferior to the prostate gland. Their secretion is rich in glycoproteins. They also form a small component of semen.
Components of semen
Semen also known as seminal fluid contain sperms in it. It is made up of secretions from the prostate glands, bulbourethral gland, and seminal vesicle. It contains fructose, amino acids, citrate, proteins, proteolytic enzymes, calcium etc.
Female Reproductive System
The female reproductive system comprises of a pair of ovaries, uterus, cervix, vagina, and external genitalia. The primary female sex organ is a pair of ovaries. Ovaries produce female gamete known as ovum. It produces female hormones known as ovarian hormones such as estrogen, progesterone etc. Ovaries are located in the lower abdomen and they are 2 to 4 cm in length. The outermost layer is made up of germinal cells known as germinal epithelium. Each ovary is covered by a thin epithelium which encloses the ovarian stroma. The stroma is divided into outer cortex and inner medulla. The female accessory ducts consist of fallopian tubes, uterus and vagina.
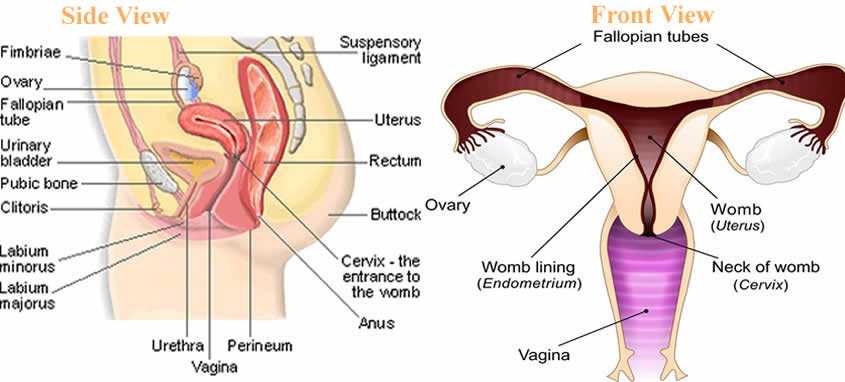
Fig.4. Female Reproductive System-side view and front view
Fallopian tubes also known as uterine tubes are fine tubes which are lined by ciliated epithelium. They lead from ovaries into the uterus. It allows the passage of egg from ovaries into the uterus. These tubes are also a site for fertilization.
Vagina is the tubular and muscular organ. It extends from the vulva to the cervix. It is covered by a membrane known as hymen. The vagina helps in sexual intercourse as well as child birth. The funnel shaped part closer to the ovary is known as infundibulum. Infundibulum contains finger-like projections known as fimbriae. They help in collection of ova after ovulation. Infundibulum opens into ampulla. The fallopian tube or oviduct ends at isthmus. Isthmus has a narrow lumen and it joins the uterus. The uterus appear pear shaped.
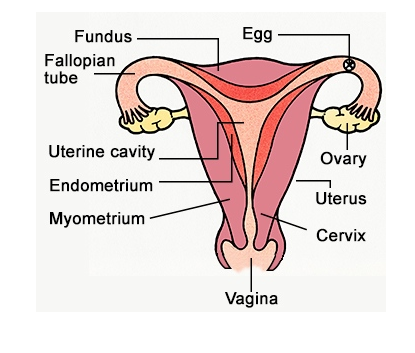
Fig.5. Diagrammatic section of Female Reproductive System
Uterus also known as womb is the site were fetus develop at the time of gestation. There are 3 layers of uterus- the external thin layer is known as perimetrium, middle layer made up of smooth layer is known as myometrium and the outer most layer which is glandular in nature is known as endometrium. It is the endometrium that lines the uterus. Myometrium brings about the contraction at the time of delivery of the baby.
The external female genitalia consist of – mons pubis, labia minora, hymen and clitoris. The fatty tissue that covers the pubic hair and skin is known as mons pubis. The folds that surround the vaginal opening is known as labia majora. The membrane that covers the opening of the vagina is known as hymen. The tiny finger-like projection that lies above the urethral opening is known as clitoris.
The characteristic feature of female mammal is the presence of mammary glands.
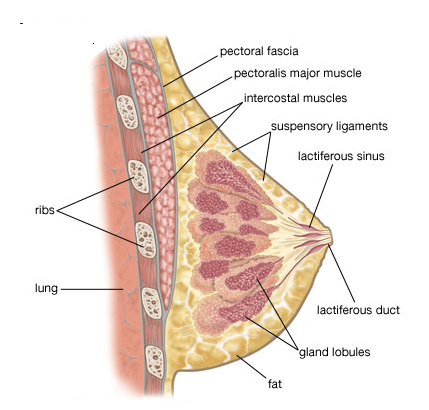
Fig.6. Mammary Glands
Mammary glands are paired structures that is made up of glandular tissue and fat. Glandular tissue comprises of mammary lobes that contain cells known as alveoli. The alveoli open into mammary tubules. These tubules then combines to form ducts.
Gametogenesis
The formation of male and female gametes, that is, sperms and ovum respectively is known as gametogenesis. Testis produce sperms in male whereas ovaries produces ovum or egg in females. The process of formation of sperms is known as spermatogenesis whereas formation of ova is known as testis.
Spermatogenesis
The process of spermatogenesis begins from diploid Spermatogonia in seminiferous tubules. Spermatogonia undergo mitotic divisions to increase their number. Some spermatogonia matures to form primary spermatocytes. Primary spermatocytes undergo meiosis to form secondary spermatocytes which are haploid in nature. One meiotic division of primary spermatocytes form two secondary spermatocytes. Now the second meiotic division begins, where secondary spermatocytes are converted into spermatids. The process of transformation of spermatids into sperm or spermatozoa is known as spermiogenesis. Then the sperms are finally released from seminiferous tubules by a process known as spermiation.
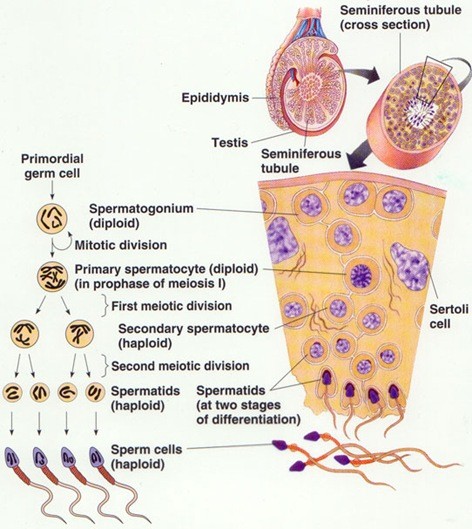
Fig. 7. Spermatogenesis
Sperm is uniflagellar structure which is motile in nature. They have a very short life span. Sperm is divided into head, middle piece, and the tail. Head contains the nucleus and it is surrounded by a structure known as acrosome. Acrosome contains the enzymes that degrades the wall of female ovum for fertilization. The middle piece contains the mitochondria that synthesizes ATP for the movement of the sperm into the female genital tract. The tail helps in movement of the sperm. It contains the flagella in it.
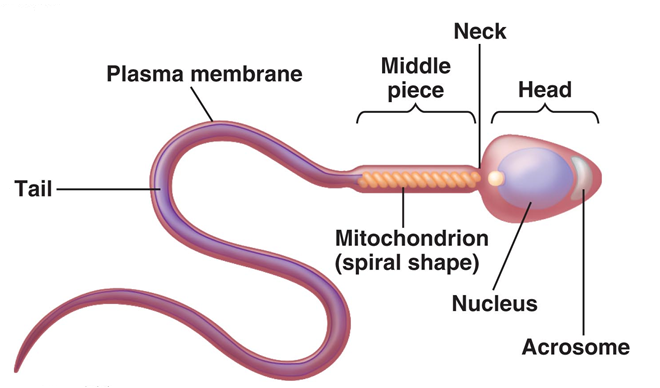
Fig. 8. Structure of the Sperm
Spermatogenesis is controlled by a gonadotropic hormone released from the hypothalamus. The two gonadotropins that are involved in spermatogenesis is luteinizing hormone and follicle stimulating hormone. Luteinizing hormone targets the leydig cells to secrete the male sex hormone known as testosterone. Follicle stimulating hormone targets the sertoli cells to nourish the sperms during spermatogenesis.
Oogenesis
The process of formation of female gamete or ovum is known as oogenesis. Oogenesis begins at the time of embryonic development of a female child. No oogonia or ovum is formed after the birth of a female child. These oogonia are arrested at prophase I of meiosis until a female child reaches the puberty. The oogonia which are arrested at prophase I of meiosis are known as primary oocytes.
Then the primary oocyte is surrounded by a layer of cells known as primary follicle.
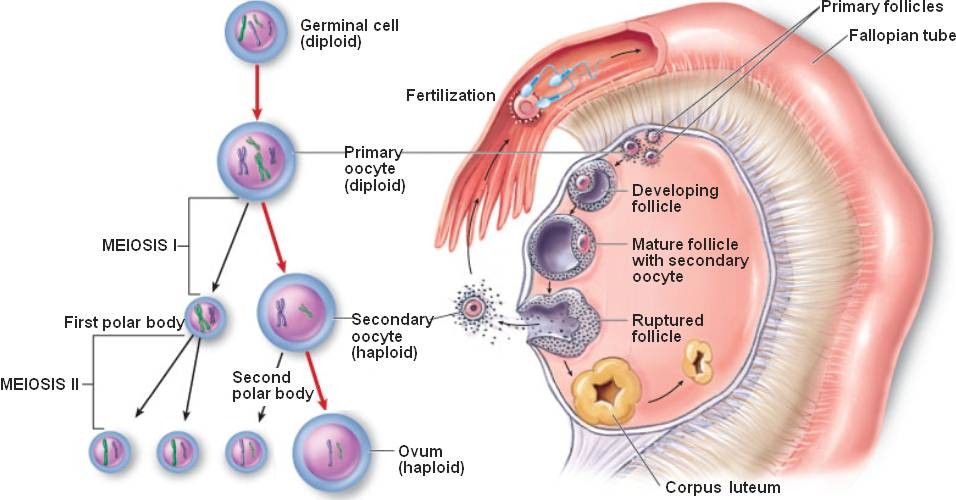
Fig. 9. Oogenesis
Primary follicle which are then later surrounded by a layer of cells is known as secondary follicles. The secondary follicle is transformed into tertiary follicle which is filled by a fluid known as antrum. At this stage the first meiotic division is complete. The first meiotic division forms a secondary oocyte and one small polar body. The secondary oocyte matures into graffian follicle. The graffian follicle is surrounded by a membrane known as zona pellucida. The graffian follicle then ruptures to release an oocyte from the ovary. The process of release of an oocyte from the ovary is known as ovulation.
Menstrual Cycle
The reproductive cycle of female primates such as apes, monkeys, females etc. is known as menstrual cycle. The onset of menstruation at puberty is known as menarche. Single ovum is released in a single cycle of menstruation. Menstrual cycle is of 28 days. It is divided into following phases-
- Menstrual phase (from day 1 to 5) – The body discharge the blood vessels from the vagina in the form of menstrual fluid. About 10 to 80 ml blood is lost in case of normal menstrual cycle.
- Follicular phase (from day 1 to 13) – In this phase, an ovum matures or prepares itself for ovulation. The lining of the uterus known as endometrium gets thickened due to lining of blood vessels. The secretion of luteinizing hormone and follicular stimulation hormone increases in this phase.
- Ovulation phase (day 14)- It is the phase where ovum is released from the ovary.
- Luteal phase (day 15 to 28) – The released ovum remains in the fallopian tube for about 24 hours. If the sperm does not enter the body, the ovum degenerates. The ovum or matured graffian follicle converts into corpus luteum. If fertilization does not corpus luteum degenerates. If fertilization occurs, corpus luteum will secrete a pregnancy hormone known as progesterone, required to maintain pregnancy.
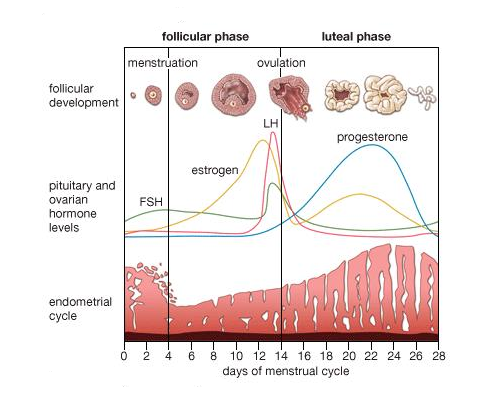
Fig. 10. Menstrual Cycle
Around 50 years the menstrual cycle ceases, this is known as menarche.
Fertilization and Implantation
The sperm that enters the female body via insemination, reaches to the female fallopian tube. The ovum released from the ovary also reaches the fallopian tube. Fallopian tube is a site where fertilization occurs. The process of fusion of male gamete, sperm with female gamete ovum is known as fertilization.
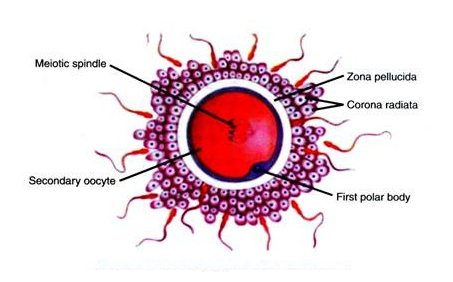
Fig. 11. Ovum surrounded by sperms during Fertilization
The sperm first meets zona pellucida layer of the ovum and induces membrane block to prevent entry of additional sperms. The secretions from the acrosome such as hyaluronidase enzyme help the sperm to enter the ovum. Now the second meiotic division of secondary oocyte is complete. This second meiotic division give rise to second polar body and an ovum.
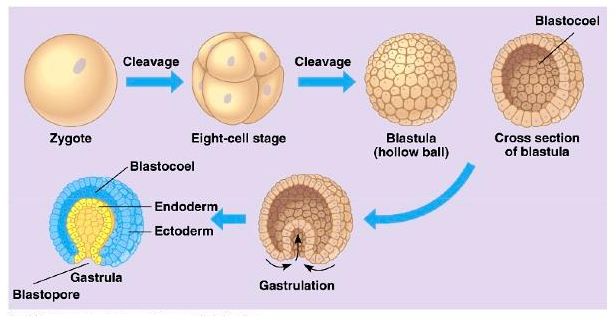
Fig.12. Embryo Development
Fertilization forms a diploid zygote. Zygote undergo various mitotic divisions to form cells known as blastomeres. These cells form a compact mass of cells known as morula (8-17 cells). Morula undergo further mitotic divisions to form blastocyst which moves further towards the uterus from the fallopian tube. The blastomeres of the blastocyst are arranged into an outer layer called trophoblast and an inner group of cells attached to trophoblast called the inner cell mass. The trophoblast layer will gets attached to the endometrium and the inner cell mass will differentiate as the embryo. The attachment of the blastocyst in the uterus is known as implantation. This marks the beginning of the pregnancy. Blastocyst then later transform into gastrula. It is the stage where 3 germ layers are formed- outermost ectoderm, middle mesoderm, and innermost ectoderm. These germ layers form different tissues and organs during embryonic development.
Pregnancy and Embryonic Development
After implantation, the uterine lining forms a structure known as placenta, for communication between the fetus and the maternal body. The placenta helps in the exchange of the nutrients and gases between the mother and the fetus. It also involved in removal of waste produced by the growing fetus. The placenta is connected to the fetus via umbilical cord. Placenta also produces different hormones needed during or after pregnancy. The hormones such as human chorionic gonadotropin (hCG), human placental lactogen (hPL), estrogens, progestogens, etc. In the later stages of pregnancy, a hormone called relaxin is also secreted by the ovary. This hormone helps in uterine contraction at the time of parturition.

Fig.13. The human fetus within the uterus
As shown from the above figure, amnion is the membrane that covers the embryo and the fluid filled in it is known as amniotic fluid. Amnion is protective in nature. It protects the growing embryo from mechanical shock or injury.
Parturition and Lactation
The process of delivery of the baby or better known as childbirth is known as parturition. There are various hormones that acts at the time of child birth such as – oxytocin and relaxin. Both promotes uterine contraction for the expulsion of the baby from the female external genital tract. During pregnancy, the mammary glands starts to produce milk. This process is known as lactation. Just after childbirth, the initial milk ejected from the maternal mammary glands is known as colostrum. The steps for the parturition are explained below in the form of the figure-
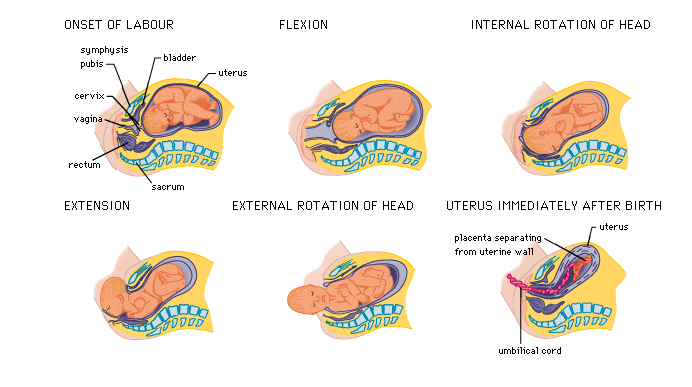
Fig.14. Parturition
