Question [Maximum marks: 13]
Haemoglobinopathies are inherited conditions linked to the structure and function of
haemoglobin. Sickle cell anaemia is one of these conditions in which the transport and
delivery of oxygen to tissues is less than normal.
An investigation was carried out to discover the effect of sickle cell anaemia on the ability of
blood to carry oxygen. Blood samples were taken from two people:
• person L without sickle cell anaemia
• person M with sickle cell anaemia.
The percentage saturation of haemoglobin with oxygen was determined over a range of
partial pressures of oxygen.
Fig. 3.1 shows oxygen haemoglobin dissociation curves for the two blood samples.
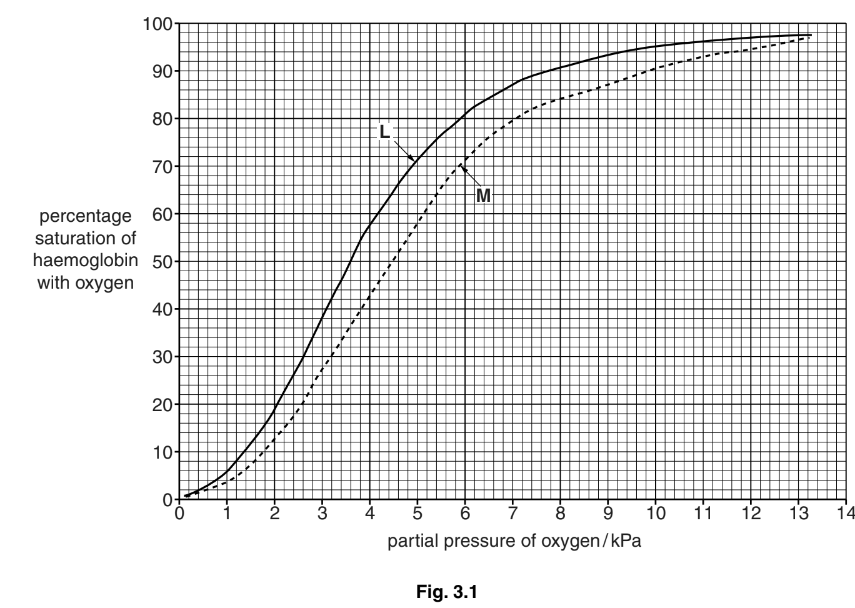
(a) P50 is the partial pressure of oxygen at which haemoglobin is 50% saturated with
oxygen. It is taken as a measurement of the affinity of haemoglobin for oxygen.
(i) State the P50 for the two blood samples, L and M.
(ii) With reference to Fig. 3.1, describe how the dissociation curve for person M differs from the dissociation curve for person L.
(b) Explain the advantage of the position of the dissociation curve for people with sickle cell
anaemia.
(c) The partial pressure of oxygen in the lungs at sea level is about 13.5 kPa. At an altitude
of 3000 metres the partial pressure of oxygen in the lungs is about 7.5 kPa.
When people move from sea level to high altitude they become adapted to the low
partial pressure of oxygen.
Describe and explain how humans become adapted to the low partial pressure of
oxygen at high altitude.
(d)Vaccination is used to control the spread of diseases, such as measles.
Explain why vaccination cannot be used to prevent sickle cell anaemia.
Answer/Explanation
Answer: 3(a) (i) no mark if no units used at all
L – 3.6 kPa ; award the mark if units only used once
M – 4.5 kPa ; A in range 4.45 to 4.55
(ii) ignore any similarities
1 to the right / lower (affinity) / qualified ; e.g. lower percentage saturation
2 at, higher / lower, partial pressures, small(er) difference in percentage saturation (than others) ; A ora 3 comparative data quote ; must refer to L and M
allow ecf from (i)
3(b) 1 at partial pressures in the tissues ; where oxygen is unloaded from Hb
2 haemoglobin is less saturated (than L) ;
3 because, haemoglobin / Hb, dissociates more readily ;
A idea of unloading oxygen more readily even if Hb not mentioned
4 to compensate for, fewer / less effective, red blood cells / Hb ;
3(c) 1 haemoglobin less well saturated (in lungs at high altitude) ;
2 data quote from Fig. 3.1 ; A 80–90% saturated at ‘about 7.5 kPa’
3 produce more red blood cells / increase in number of RBCs ;
4 more haemoglobin ;
5 idea of compensates for, smaller volume of oxygen absorbed / lower saturation (of haemoglobin) ;
also accept the following adaptations
6 increase in haematocrit / AW / decrease in plasma volume ;
A increase in RBCs per unit volume
R decrease in blood volume
7 increase in, breathing rate / tidal volume / heart rate / stroke volume ;
8 increase in, capillary density / number of mitochondria / myoglobin / respiratory enzymes, in muscle ; 9 ref. to (increased) secretion of, erythropoietin / EPO ;
10 increase in (2,3), BPG / DPG, in red blood cells ; A rightward shift in curve [max 4]
3(d) 1 not caused by (named type of) pathogen / non-infectious / non-transmissible / non-
communicable / AW ; 2 genetic / inherited / AW, disease ; A caused by a mutation / AW
A ‘passed down from parent(s)’
R idea of congenital diseases
R ‘you get it from your mother’
3 ref. to, no immune response / no antigen(s) ;
4 affects all red blood cells so vaccine would lead to their destruction ; [max 2]
Question
Capillaries are known as exchange vessels. Substances are exchanged between blood and tissue fluid as the blood flows through the capillaries.
Fig. 1.1 is an electron micrograph of a section through a capillary with two red blood cells.
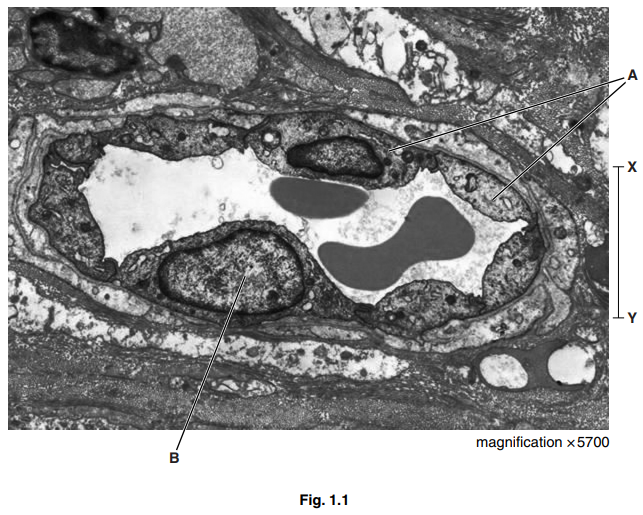
(a) (i) Name the cells labelled A and the structure labelled B.[2]
A
B
(ii) Calculate the actual distance X – Y on Fig. 1.1.
Show your working and give your answer to the nearest micrometre (μm).
answer μm [2]
(iii) Explain how capillaries are adapted for their function as exchange vessels.[2]
(b) Table 1.1 shows the composition of blood, tissue fluid and lymph.
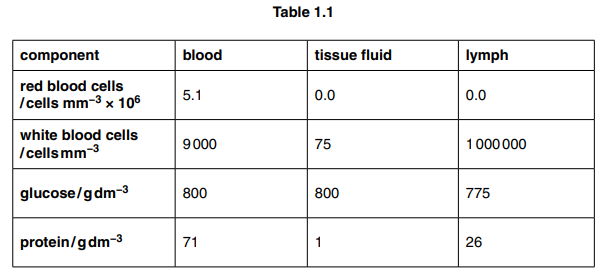
Explain the differences between the composition of blood, tissue fluid and lymph as shown in Table 1.1, for white blood cells, glucose and protein.[5]
white blood cells
glucose
protein
(c) Outline how red blood cells are involved in the transport of carbon dioxide.[3] [Total: 14]
Answer/Explanation
Ans:
1 (a) (i) A – endothelial/ squamous / epithelial (cell) ;
B – nucleus ;
(ii) 7 (µm) ;;
award two marks if correct answer given
award one mark if not rounded to nearest whole number
award one mark if given incorrect unit
if no answer given, award one mark if correct measurement
(38–41/ 3.8–4.1/38000–41000) is divided by 5700
(iii) for two marks – one structure and one function
only two functions = 1 mark
only two structures = 1 mark
1 (capillary) wall is, thin/ single layer of cells / one cell thick ;
A endothelium/ epithelium for wall
2 short diffusion, pathway / distance/AW ;
R ‘easy’ diffusion
3 (many have) endothelial pores / fenestrations / gaps / spaces / openings ;
4 to allow named, substance/ cell, to leave the blood ;
A idea of separation/ selection, of named substance(s) by size
5 small diameter/ small lumen/ diameter of red blood cells ;
6 slows down flow of red blood cells /(capillary / blood) close to cells ;
7 (capillaries have) large, surface area/ surface area to volume ratio ;
8 idea that allows more exchange ;
Ignore faster exchange
(b) white blood cells
1 (named) white blood cells can, leave capillaries / enter tissue fluid ;
A diapedesis /(suggestion that some) too large to leave the, blood/ capillaries
2 high number in, lymph nodes / thymus / bone marrow/ spleen ;
A stored/ produced
glucose
3 small (molecule) ;
4 filtered/ diffuses /leaves / leaks, from blood/ from capillaries / into tissue fluid ;
5 taken up / used, by cells in respiration ;
Ignore supply
protein
6 too large to, leave capillaries / enter lymph/ enter tissue fluid ;
7 (in lymph / tissue fluid) antibodies / proteins, from/ secreted by, lymphocytes / other cells ;
(c) accept hydrogen carbonate (ions)/ bicarbonate (ions)/HCO3– penalise HCO3 once only
1 carbon dioxide, reacts / combines, with (terminal amine/N terminal, of) haemoglobin ;
R carried by /reacts with, haem
2 to form carbaminohaemoglobin ;
3 carbonic anhydrase catalyses, formation of carbonic acid (H2CO3)/reverse reaction described (in the lungs) ;
4 (carbonic acid dissociates to) HCO3– /CHO3– / hydrogen carbonate (and H+) ;
5 hydrogen carbonate/HCO3–, diffuses /moves /AW, out (into plasma) ;
Question
Erythropoietin, also known as EPO, is a large glycoprotein synthesised by specialised cells in the kidney. These cells are very sensitive to changes in oxygen concentration in the blood passing through the kidney and respond to a low oxygen concentration by increasing the synthesis of EPO.
EPO acts at the surface of particular target cells, such as cells in the bone marrow. These bone marrow cells are stimulated to produce red blood cells.
(a) (i) A low oxygen concentration also leads to an increase in the quantity of mRNA in the specialised cells in the kidney.
Suggest and explain why there is this increase in the quantity of mRNA.[2]
(ii) EPO is stored in secretory vesicles before being released from the specialised kidney cells.
Outline how EPO is released from the cells.[2]
(b) All cells of the body are exposed to circulating blood plasma containing EPO, but only particular target cells respond.
(i) Suggest and explain how EPO acts on target cells and why other cells are not affected.[3]
(ii) EPO cannot pass through the cell surface membrane to enter the bone marrow cells. Suggest one reason why this is so.[1]
(c) Red blood cells originate from undifferentiated cells in the bone marrow that are capable of continuous mitotic cell division.
State the name of this type of undifferentiated cell.[1]
(d) As part of an investigation into the body’s response to EPO, a group of healthy young men were given injections of EPO every day for four weeks.
The haemoglobin (Hb) concentration for each subject was measured at the start of the investigation and then at intervals of one week for the next ten weeks. The first measurement was taken two weeks before the first EPO injection was given.
Fig. 3.1 shows the mean results for the subjects.
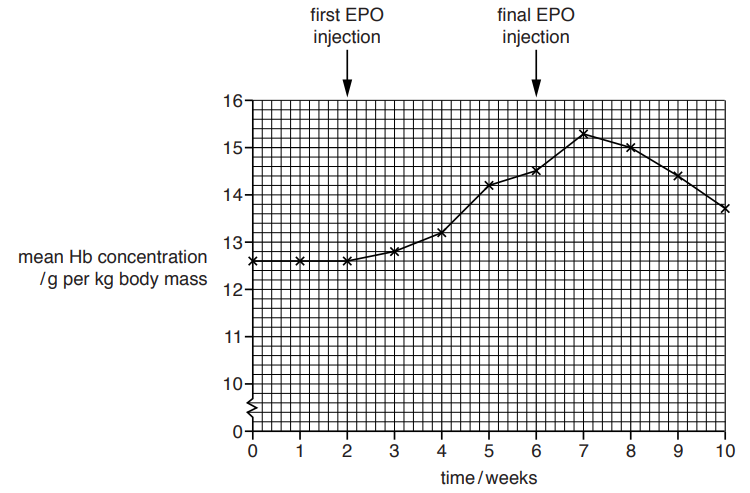
Describe the results shown in Fig. 3.1 and suggest explanations for these results.[4]
(e) The concentration of EPO in the blood plasma of a person will increase when travelling from sea level to a high altitude. This is in response to the decrease in oxygen partial pressure in the atmosphere.
Explain why an increase in EPO blood plasma concentration will be of benefit if the person remains at high altitude.[3] [Total: 16]
Answer/Explanation
Ans:
3 (a) (i) a gene codes for a protein/gene coding for EPO ;
ref. transcription ; A gene ‘switched on’
A increase gene expression
mRNA (required) for, EPO/ protein, synthesis
or
mRNA involved in translation ;
(ii) vesicles move to, cell (surface)/ plasma, membrane (via cytoskeleton) ;
(vesicles) fuse/merge, with cell (surface) membrane ;
exocytosis (occurs) ;
(movement of vesicle/ exocytosis) requires, energy /ATP ;
A active (process)
R active transport
(b) (i) EPO, binds to/ combines with/AW, receptors ;
receptors, complementary to/ specific shape for, EPO ;
A EPO fits into receptors
cell signalling/EPO binding leads to (specific) responses within the (target) cells /AW ;
I cells respond to EPO
only, target/ bone marrow, cells, have receptors, for EPO/ specific to EPO ; ora
A binding triggers responses only within, target/ bone marrow, cells
(ii) too large ;
ref. to shape, cannot pass through ;
(protein) is, hydrophilic /water soluble, and cannot cross hydrophobic core (of phospholipid bilayer)/AW ;
no specific membrane transport protein ;
(c) stem cell ; A haematopoietic stem cell
treat as neutral adult/non-embryonic / multipotent/ stromal
(d) max 3 if all description (D) or all explanation (E)
A Hb for haemoglobin and Hb concentration for mean Hb concentration
A g per kg/ gkg–1, for g per kg body mass
constant
D Hb concentration, remains constant/ of 12.6gkg–1, for first two weeks (of investigation)/ up to start of injections ;
E idea of regulation ;
e.g. sufficient oxygen so no requirement for increased EPO
increase then decrease description
D (then) increase in Hb concentration (from week 2) for 5 weeks /AW, then decrease (for last three weeks / to week 10) ;
D data quote/ manipulated data, to support ;
e.g. increase from 12.6gkg–1 (week 2) to15.3gkg–1 (week 7)
increases by 2.7gkg–1 (to week 7)
decrease from 15.3gkg–1 (week 7) to 13.7gkg–1 (week 10)
decreases by 1.6gkg–1 (to week 10)
increase explanation
E EPO increases production of red blood cells that contain Hb/AW ;
decrease explanation
E red blood cells, short life span/ die ;
E cell signalling stops /(target/ bone marrow) cells no longer stimulated/AW ;
A EPO, degraded/AW
increase after injections stop
D Hb concentration increases for 1 week after injections have finished ;
E idea of, time delay for red blood cell production to stop/ time for immature
red blood cells to mature and be released into blood stream ;
AVP ; e.g. steady increase as time required for, mitosis / cell
proliferation/ differentiation into red blood cells / production of haemoglobin
contributory factor for increase may be, accumulation/ increased concentration, of EPO with injections
(e) high altitudes and low oxygen partial pressure so
less oxygen in inhaled air/ less oxygen (would be) transported to tissue/AW ;
lower oxygen saturation of haemoglobin/ haemoglobin has lower oxygen affinity ;
body requires more red blood cells that contain haemoglobin/AW ;
A more red blood cells produced so more haemoglobin (to bind oxygen)
idea of compensation ; R idea of body getting more oxygen
