CIE AS/A Level Biology -10.2 Antibiotics- Study Notes- New Syllabus
CIE AS/A Level Biology -10.2 Antibiotics- Study Notes- New Syllabus
Ace A level Biology Exam with CIE AS/A Level Biology -10.2 Antibiotics- Study Notes- New Syllabus
Key Concepts:
- outline how penicillin acts on bacteria and why antibiotics do not affect viruses
- discuss the consequences of antibiotic resistance and the steps that can be taken to reduce its impact
Action of Penicillin and Antibiotics on Microbes
🌱 Overview
Penicillin is an antibiotic that targets bacterial infections. Antibiotics do not affect viruses because of fundamental differences in their structure and metabolism.
1. How Penicillin Acts on Bacteria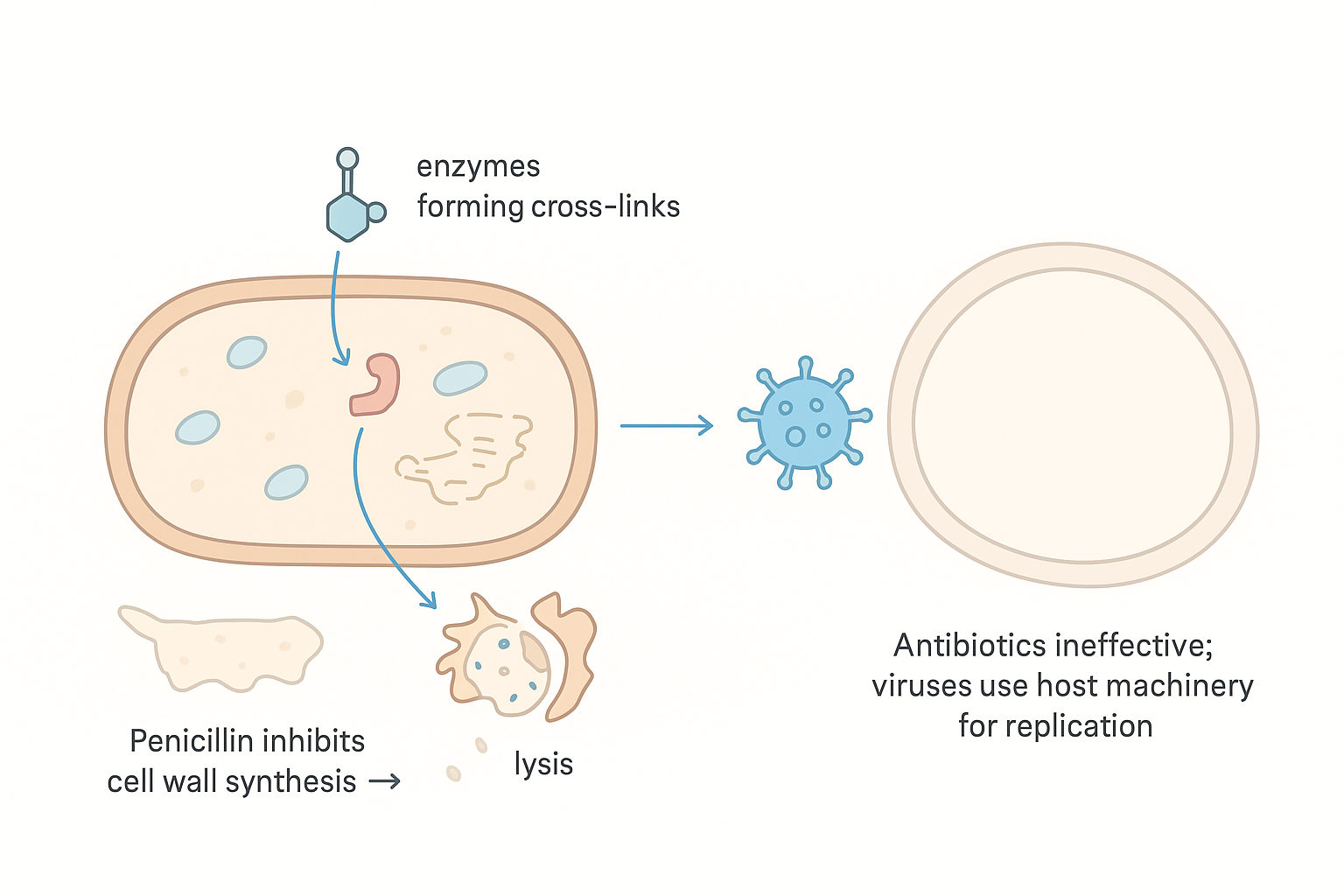
- Target: Bacterial cell wall (peptidoglycan layer).
- Mode of Action: Inhibits enzymes that form cross-links in the cell wall during bacterial growth. Weakens the cell wall → bacteria cannot withstand osmotic pressure → lysis (bursting) occurs.
- Effect: Kills actively dividing bacteria, preventing infection spread.
2. Why Antibiotics Do Not Affect Viruses
- Viruses lack cellular structures such as:
- Cell walls
- Ribosomes
- Metabolic machinery
- Reason: Antibiotics target bacterial structures and metabolic processes, which viruses do not have. Viruses replicate inside host cells using the host’s machinery.
- Implication: Viral infections (e.g., HIV, influenza) require antiviral drugs or immune response, not antibiotics.
📊 Summary Table: Penicillin and Antibiotic Action
| Feature | Bacteria | Viruses |
|---|---|---|
| Cell wall | Present (peptidoglycan) | Absent |
| Ribosomes/metabolism | Present | Absent; rely on host |
| Effect of penicillin | Cell wall synthesis inhibited → lysis | No effect |
| Treatment | Antibiotics effective | Require antivirals or immune response |
🧠 Key Points:
– Penicillin kills bacteria by disrupting cell wall formation.
– Antibiotics are ineffective against viruses due to the absence of target structures.
– Misuse of antibiotics can lead to antibiotic resistance in bacteria.
– Penicillin kills bacteria by disrupting cell wall formation.
– Antibiotics are ineffective against viruses due to the absence of target structures.
– Misuse of antibiotics can lead to antibiotic resistance in bacteria.
Antibiotic Resistance: Consequences and Control
🌱 Overview
Antibiotic resistance occurs when bacteria evolve mechanisms to survive exposure to antibiotics. It is a major public health concern, reducing the effectiveness of treatments.
🔬 Consequences of Antibiotic Resistance
| Consequence | Explanation |
|---|---|
| Treatment failure | Standard antibiotics no longer kill resistant bacteria → infections persist |
| Longer illness and recovery | Patients remain sick for longer, increasing complications |
| Increased healthcare costs | Requires more expensive or prolonged treatments |
| Spread of resistant bacteria | Resistant strains can infect others, leading to outbreaks |
| Higher mortality rates | Resistant infections are harder to treat → higher risk of death |
| Limited treatment options | Some bacteria become multi-drug resistant, leaving very few options |
🔬 Steps to Reduce the Impact of Antibiotic Resistance
| Step | Explanation |
|---|---|
| Rational use of antibiotics | Only prescribed when necessary; full course must be completed |
| Infection prevention and hygiene | Handwashing, sanitation, vaccination reduce spread of bacteria |
| Monitoring and surveillance | Track resistant strains to implement control measures |
| Development of new antibiotics | Research for novel drugs to treat resistant bacteria |
| Public education | Awareness campaigns to avoid misuse and self-medication |
| Restricting use in agriculture | Reduce antibiotics in livestock to prevent resistant strains entering humans |
🧠 Key Points:
– Antibiotic resistance threatens modern medicine, making common infections harder to treat.
– Prevention requires responsible antibiotic use, hygiene, vaccination, and research.
– Global cooperation is essential to control the spread of resistant bacteria.
– Antibiotic resistance threatens modern medicine, making common infections harder to treat.
– Prevention requires responsible antibiotic use, hygiene, vaccination, and research.
– Global cooperation is essential to control the spread of resistant bacteria.
