CIE AS/A Level Biology -11.2 Antibodies and vaccination- Study Notes- New Syllabus
CIE AS/A Level Biology -11.2 Antibodies and vaccination- Study Notes- New Syllabus
Ace A level Biology Exam with CIE AS/A Level Biology -11.2 Antibodies and vaccination- Study Notes- New Syllabus
Key Concepts:
- relate the molecular structure of antibodies to their functions
- outline the hybridoma method for the production of monoclonal antibodies
- outline the principles of using monoclonal antibodies in the diagnosis of disease and in the treatment of disease
- describe the differences between active immunity and passive immunity and between natural immunity and artificial immunity
- explain that vaccines contain antigens that stimulate immune responses to provide long-term immunity
- explain how vaccination programmes can help to control the spread of infectious diseases
Antibodies: Structure and Function
🌱 Overview
Antibodies (immunoglobulins) are Y-shaped proteins produced by plasma cells in response to antigens.
Their molecular structure is directly related to their function in immune defense.
🔬 Molecular Structure of Antibodies
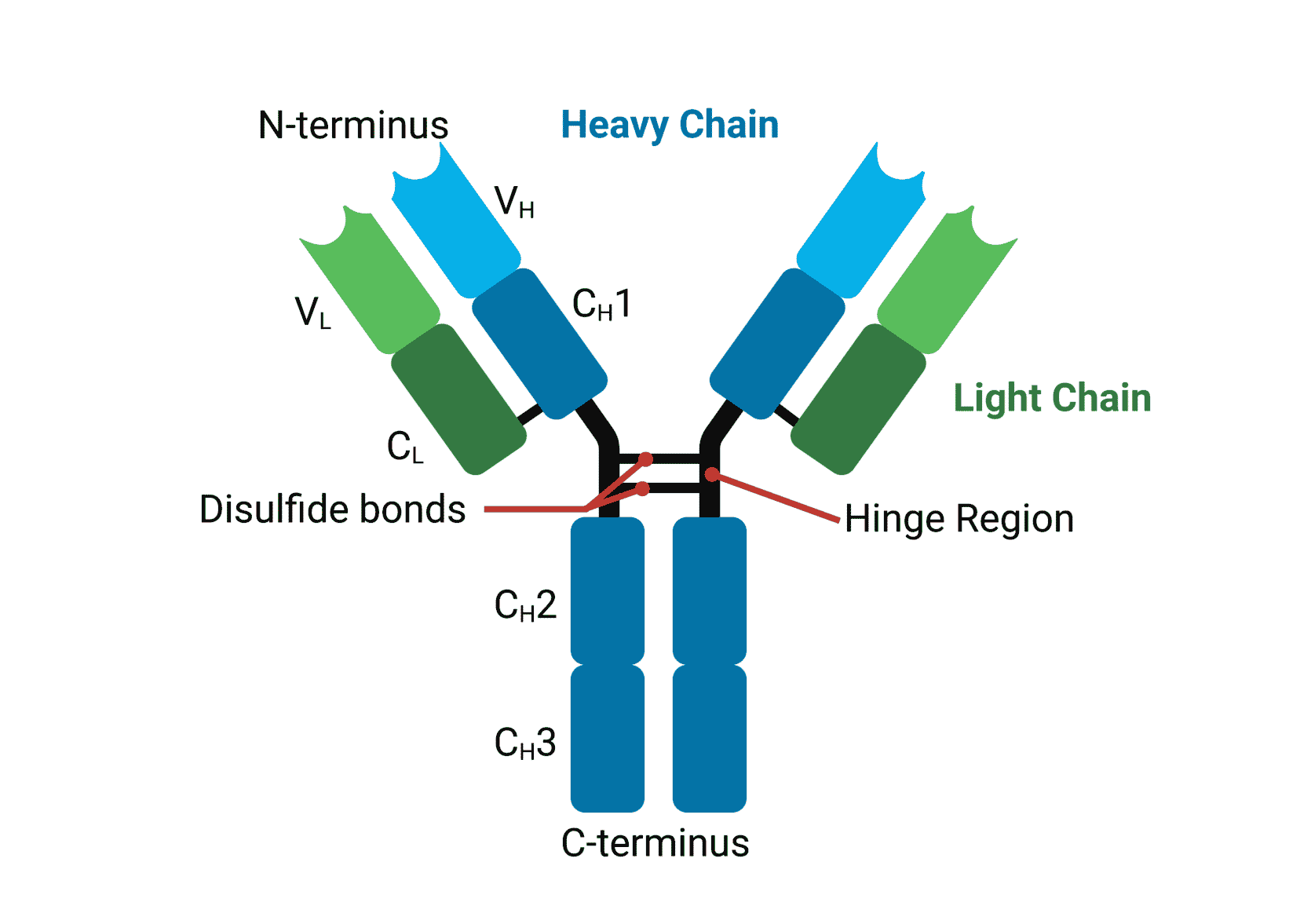
| Component | Description | Function Related to Structure |
|---|---|---|
| Two heavy chains | Long polypeptide chains forming the main Y structure | Provide stability and shape; contribute to antigen binding |
| Two light chains | Short polypeptide chains attached to heavy chains | Contribute to antigen-binding sites |
| Variable region (Fab) | Ends of the Y arms; unique for each antibody | Binds specifically to a complementary antigen |
| Constant region (Fc) | Stem of the Y; same in all antibodies of a class | Determines antibody class and interacts with immune cells |
| Hinge region | Flexible region between Fab and Fc | Allows movement of arms to bind antigens efficiently |
| Disulfide bonds | Connect chains | Maintain stability of structure |
🔬 Functions Related to Structure
- Specific antigen recognition: Variable regions allow each antibody to bind specifically to a particular antigen.
- Neutralization of pathogens: Binding to toxins or viruses prevents them from interacting with host cells.
- Opsonization: Fc region interacts with phagocytes, promoting phagocytosis of the pathogen.
- Activation of complement system: Fc region can trigger a cascade that destroys pathogens.
- Agglutination: Y-shaped structure allows cross-linking of multiple pathogens, forming clumps that are easier to phagocytose.
– Variable region = specificity to antigen → adaptive immunity.
– Constant region = interacts with immune system → effector functions.
– Overall structure ensures recognition, neutralization, and removal of pathogens.
Hybridoma Method for Production of Monoclonal Antibodies
🌱 Overview
Monoclonal antibodies (mAbs) are antibodies that are identical and specific to a single antigen.
The hybridoma method is used to produce large quantities of these antibodies in the lab.
🔬 Steps in the Hybridoma Method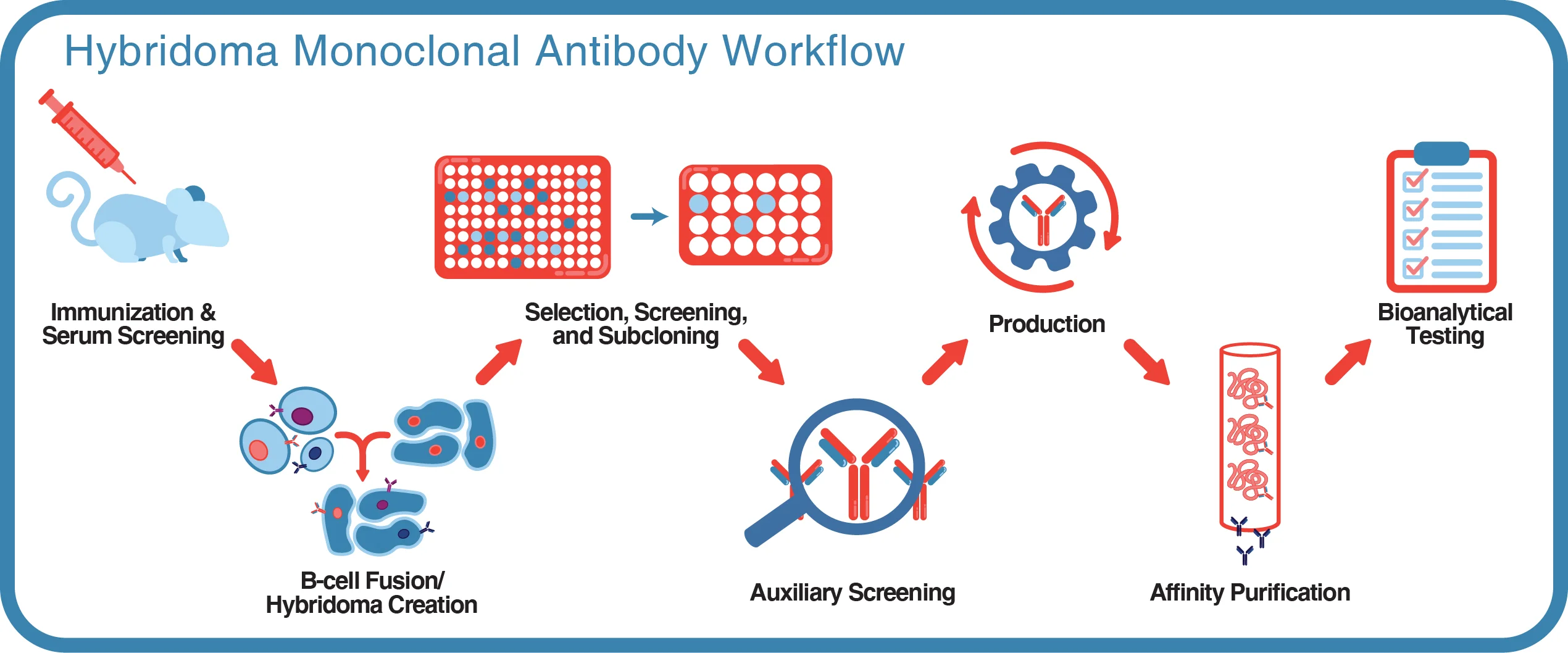
Immunization
- A mouse (or other suitable animal) is injected with the target antigen.
- The mouse’s B-lymphocytes produce antibodies specific to the antigen.
Isolation of B-lymphocytes
- B-cells are collected from the spleen of the immunized mouse.
Fusion with Myeloma Cells
- B-cells are fused with cancerous myeloma cells (which can divide indefinitely).
- Fusion forms hybrid cells called hybridomas, which combine:
- Antibody production ability from B-cells
- Immortality from myeloma cells
Selection of Hybridomas
- Hybridomas are cultured in HAT medium, which allows only fused cells to survive.
Screening for Desired Antibody
- Hybridomas are tested to identify those producing the specific antibody against the target antigen.
Cloning and Mass Production
- Selected hybridomas are cloned to produce identical cells, all secreting the same monoclonal antibody.
- Antibodies are harvested from culture medium for use in research, diagnostics, or therapy.
📊 Summary Table: Hybridoma Method
| Step | Purpose |
|---|---|
| Immunization | Stimulate B-cells to produce target antibodies |
| Isolation of B-cells | Collect antibody-producing cells |
| Fusion with myeloma cells | Create immortal hybrid cells |
| Selection in HAT medium | Remove unfused cells |
| Screening | Identify hybridomas producing desired antibody |
| Cloning & production | Mass-produce monoclonal antibodies |
– Monoclonal antibodies are highly specific to a single antigen.
– Hybridoma cells are immortal, allowing continuous antibody production.
– Used in diagnostics, research, and therapies (e.g., cancer treatment, pregnancy tests).
Monoclonal Antibodies: Principles in Diagnosis and Treatment
🌱 Overview
Monoclonal antibodies (mAbs) are identical antibodies that bind specifically to a single antigen.
Their specificity allows them to be used in disease diagnosis and therapy.
1. Use in Diagnosis of Disease
| Principle | Explanation | Example |
|---|---|---|
| Specific binding to antigen | mAbs bind to antigens associated with pathogens or diseased cells | Detecting HIV antigens in blood tests |
| Labelling with markers | Antibodies are linked to enzymes, fluorescent dyes, or radioactive markers | ELISA test, immunofluorescence assays |
| Detection of antigen-antibody complexes | Produces a visible signal indicating presence of disease | Pregnancy tests detect hCG using mAbs |
Diagnosis relies on high specificity → low chance of false positives.
2. Use in Treatment of Disease
| Principle | Explanation | Example |
|---|---|---|
| Targeting specific cells | mAbs bind to antigens on diseased cells (e.g., cancer cells) | Rituximab targets B-cells in lymphoma |
| Neutralization of pathogens/toxins | mAbs bind and block harmful molecules | Antibodies neutralizing toxins or viruses |
| Delivery of drugs/radiation | mAbs can carry drugs or radioactive substances directly to target cells | Targeted cancer therapy |
| Immune system activation | Fc region of mAbs can trigger immune cells to destroy target cells | Antibody-dependent cellular cytotoxicity (ADCC) |
Key Point:
Therapy exploits specificity to reduce side effects and improve effectiveness.
– Diagnosis: Detect disease antigens with high specificity.
– Treatment: Target diseased cells or molecules, deliver drugs, or activate immune response.
– Monoclonal antibodies are powerful tools in modern medicine due to their precision.
Immunity: Active vs Passive, Natural vs Artificial
🌱 Active vs Passive Immunity
| Feature | Active Immunity | Passive Immunity |
|---|---|---|
| Definition | Immunity developed when the body’s own immune system produces antibodies after exposure to an antigen | Immunity obtained when ready-made antibodies are transferred into the body |
| How it develops | Through infection (natural) or vaccination (artificial) | Through maternal antibodies (natural) or injection of antibodies/serum (artificial) |
| Time taken | Slow (days–weeks) to develop | Immediate protection |
| Duration | Long-lasting (memory cells formed) | Short-term (no memory cells formed) |
| Example | Immunity after recovering from chickenpox | Antibodies passed from mother to baby via breast milk |
🌱 Natural vs Artificial Immunity
| Feature | Natural Immunity | Artificial Immunity |
|---|---|---|
| Definition | Immunity gained through normal life processes without medical intervention | Immunity gained through medical intervention |
| Example (Active) | Recovery from infection (e.g., measles) | Vaccination with weakened or killed pathogens |
| Example (Passive) | Maternal antibodies across placenta or in breast milk | Injection of antiserum or monoclonal antibodies |
– Active immunity = body makes its own antibodies → long-term, memory cells.
– Passive immunity = ready-made antibodies → immediate but short-term.
– Natural immunity = occurs without medical help.
– Artificial immunity = achieved with medical intervention (vaccines, antibody injections).
Vaccines and Long-Term Immunity
🌱 What is a Vaccine?
A vaccine is a preparation that contains antigens from a pathogen. These antigens may be:
- Inactivated (killed) pathogens
- Weakened (attenuated) pathogens
- Isolated antigens (proteins, toxoids)
- Recombinant antigens (produced by genetic engineering)
🔬 How Vaccines Work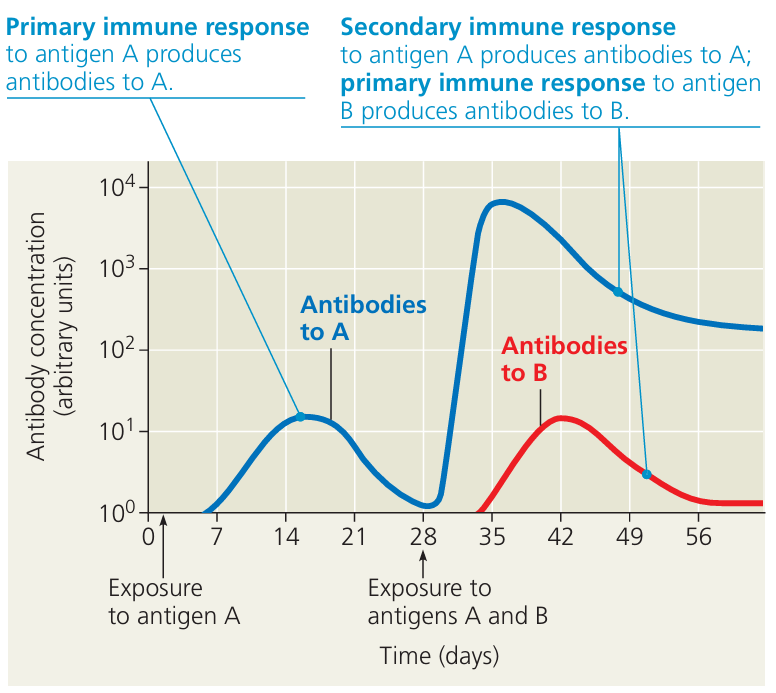
- Antigen Introduction: The vaccine introduces non-harmful antigens into the body. No actual disease is caused.
- Immune Response Triggered:
- Macrophages present antigens to lymphocytes.
- B-lymphocytes → form plasma cells → produce antibodies.
- T-helper cells stimulate B-cells.
- Some B- and T-lymphocytes differentiate into memory cells.
- Formation of Long-Term Immunity:
- On future exposure to the real pathogen: memory cells respond rapidly and strongly.
- More antibodies produced, faster.
- Pathogen destroyed before symptoms appear.
🧠 Key Idea:
Vaccines mimic infection → stimulate a primary immune response safely.
Immunity is long-term because memory cells remain in the body.
📌 Example
Polio vaccine → contains inactivated poliovirus. Provides long-term protection by generating immune memory without causing polio.
– Vaccines contain antigens, not active pathogens.
– They stimulate the immune system to produce antibodies and memory cells.
– Result = long-term immunity without illness.
Vaccination Programmes and Control of Infectious Diseases
🌱 How Vaccination Controls Disease Spread
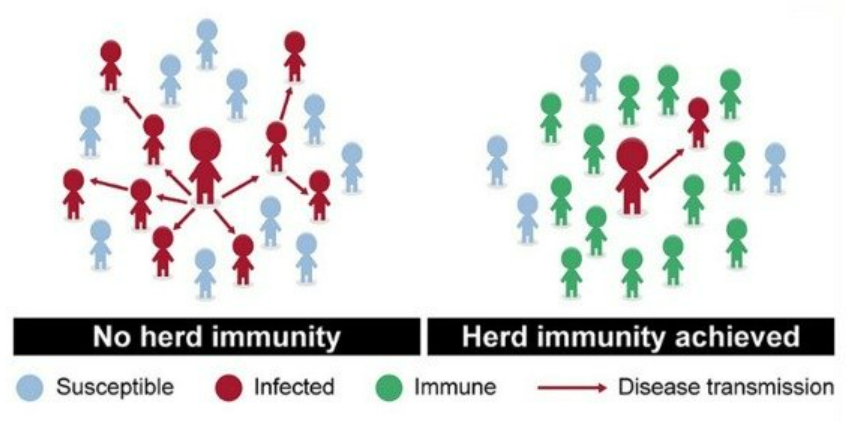
Herd Immunity:
- If a high % of the population is vaccinated, most people are immune.
- Pathogens cannot spread easily because there are fewer susceptible hosts.
- Protects even those who are not vaccinated (e.g., newborns, immunocompromised).
- Breaks Transmission Cycle: Fewer infected people → less chance of passing pathogen to others.
Rapid Immune Response: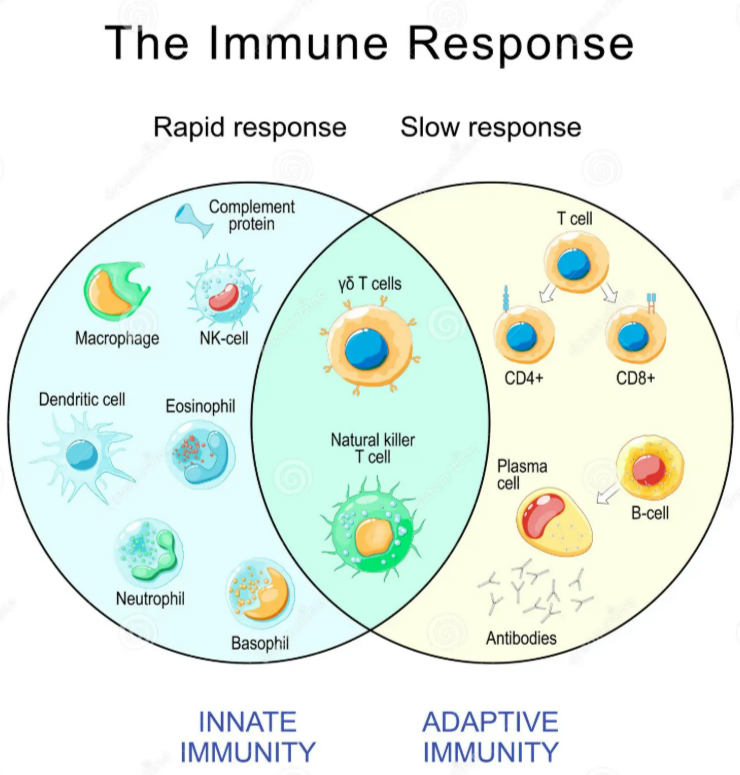
- Vaccinated individuals already have memory cells.
- If exposed, their immune system quickly eliminates the pathogen before symptoms develop.
- This reduces carriers in the population.
- Eradication Potential: With global vaccination, some diseases can be eliminated completely (e.g., smallpox eradicated in 1980).
🔬 Factors Affecting Success of Vaccination Programmes
- Pathogen mutation (e.g., influenza) may produce new antigens → vaccines become less effective.
- Logistics and cost of large-scale immunisation.
- Public acceptance: some people may refuse vaccines (due to fear, misinformation, or cultural reasons).
- Pathogen characteristics: vaccines work best against pathogens with a single stable antigen and no animal reservoirs (e.g., smallpox).
📌 Examples
- Smallpox: eradicated by worldwide vaccination.
- Polio: nearly eradicated due to mass vaccination programmes.
- Measles: controlled in many countries, but outbreaks still occur if vaccination rates drop.
🧠 Summary Box:
Vaccination programmes reduce disease incidence by:
– Creating herd immunity
– Interrupting transmission
– Protecting vulnerable groups
Success depends on: high coverage, stable pathogen, and public cooperation.