CIE AS/A Level Biology -14.1 Homeostasis in mammals- Study Notes- New Syllabus
CIE AS/A Level Biology -14.1 Homeostasis in mammals- Study Notes- New Syllabus
Ace A level Biology Exam with CIE AS/A Level Biology -14.1 Homeostasis in mammals- Study Notes- New Syllabus
Key Concepts:
- explain what is meant by homeostasis and the importance of homeostasis in mammals
- explain the principles of homeostasis in terms of internal and external stimuli, receptors, coordination systems (nervous system and endocrine system), effectors (muscles and glands) and negative feedback
- state that urea is produced in the liver from the deamination of excess amino acids
- describe the structure of the human kidney, limited to: fibrous capsule, cortex, medulla, renal pelvis, ureter, branches of the renal artery and renal vein
- Identify, in diagrams, photomicrographs and electron micrographs, the parts of a nephron and its associated blood vessels and structures, limited to: glomerulus, Bowman’s capsule, proximal convoluted tubule, loop of Henle, distal convoluted tubule, collecting duct
- describe and explain the formation of urine in the nephron, limited to:
• the formation of glomerular filtrate by ultrafiltration in the Bowman’s capsule
• selective reabsorption in the proximal convoluted tubule - relate the detailed structure of the Bowman’s capsule and proximal convoluted tubule to their functions in the formation of urine
- describe the roles of the hypothalamus, posterior pituitary gland, antidiuretic hormone (ADH), aquaporins and collecting ducts in osmoregulation
- describe the principles of cell signalling using the example of the control of blood glucose concentration by glucagon, limited to:
• binding of hormone to cell surface receptor causing conformational change
• activation of G-protein leading to stimulation of adenylyl cyclase
• formation of the second messenger, cyclic AMP (cAMP)
• activation of protein kinase A by cAMP leading to initiation of an enzyme cascade
• amplification of the signal through the enzyme cascade as a result of activation of more and more enzymes by phosphorylation
• cellular response in which the final enzyme in the pathway is activated, catalysing the breakdown of glycogen - explain how negative feedback control mechanisms regulate blood glucose concentration, with reference to the effects of insulin on muscle cells and liver cells and the effect of glucagon on liver cells
- explain the principles of operation of test strips and biosensors for measuring the concentration of glucose in blood and urine, with reference to glucose oxidase and peroxidase enzymes
Homeostasis in Mammals
📌 Definition
- Homeostasis is the process by which an organism maintains a stable internal environment, despite changes in the external environment.
🌱 Importance in Mammals
- Maintains enzyme efficiency: Most enzymes work optimally at specific temperatures and pH. Homeostasis keeps these conditions stable for efficient metabolic reactions.
- Regulates water and ion balance: Prevents dehydration or excessive water uptake. Maintains osmotic balance, essential for cell function.
- Maintains blood glucose levels: Ensures steady energy supply for cells, especially brain and muscles.
- Controls body temperature: Prevents hyperthermia or hypothermia, protecting vital organs.
- Removes waste products efficiently: Maintains healthy internal environment by excreting urea, CO₂, and other wastes.
🧠 Key Points
- Homeostasis is vital for survival, growth, and normal functioning of mammals.
- Achieved through feedback mechanisms (negative and positive feedback).
- Examples include thermoregulation, osmoregulation, and blood glucose regulation.
Principles of Homeostasis
📌 Overview
- Homeostasis involves detecting changes, coordinating a response, and restoring stable internal conditions.
- Achieved through negative feedback mechanisms using receptors, coordination systems, and effectors.
🌱 Steps in Homeostasis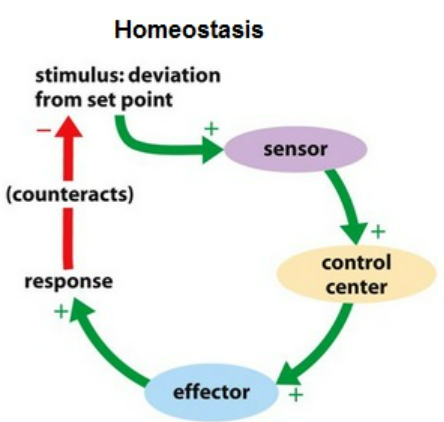
- Stimuli:
- Internal stimuli: Changes inside the body (e.g., blood glucose, body temperature).
- External stimuli: Changes in the environment (e.g., ambient temperature, light, oxygen levels).
- Receptors: Detect changes in the internal or external environment. Examples: thermoreceptors in skin, chemoreceptors in blood vessels.
- Coordination Systems:
- Nervous system: Fast, short-term responses using nerve impulses.
- Endocrine system: Slower, long-term responses using hormones.
- Effectors:
- Muscles: Contract or relax to produce a response (e.g., shivering, sweating).
- Glands: Secrete hormones or enzymes (e.g., insulin release).
- Negative Feedback: Response opposes the initial change, restoring conditions to the set point. Example: Blood glucose rises → insulin released → glucose taken up by cells → blood glucose falls → insulin secretion decreases.
🧠 Key Points:
- Homeostasis maintains stable internal conditions despite external or internal changes.
- Negative feedback is the main principle: the system counters deviations from the set point.
- Effective homeostasis requires receptors, coordination systems, and effectors working together.
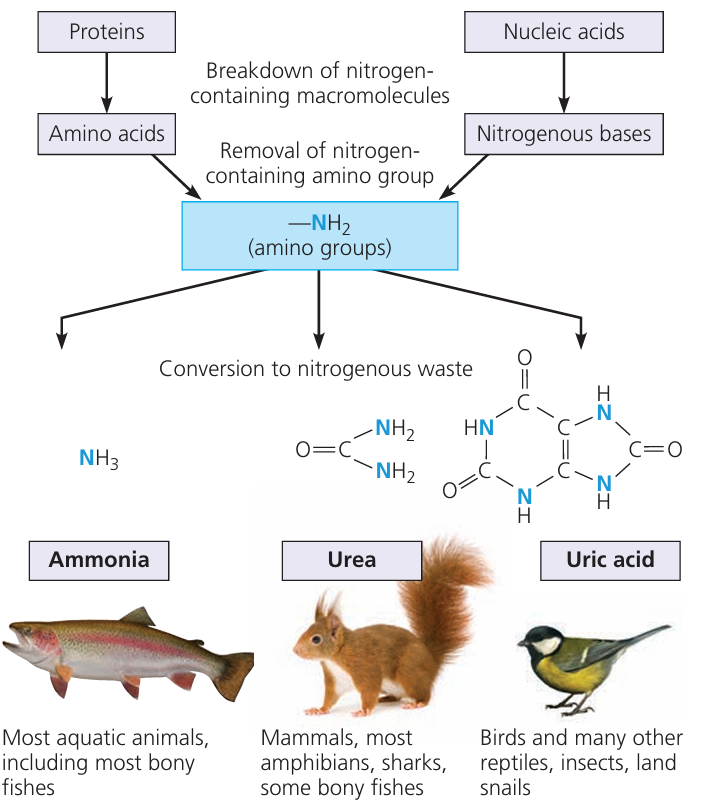
Urea Production in Mammals
📌 Overview
- Urea is a nitrogenous waste produced in the liver.
- Formed from the deamination of excess amino acids when protein intake exceeds the body’s needs.
🌱 Process of Urea Formation
- Deamination of amino acids: The amino group (-NH₂) is removed from amino acids, producing ammonia (NH₃), which is highly toxic.
- Conversion to urea: Ammonia reacts with carbon dioxide in the liver to form urea, which is less toxic than ammonia.
- Transport and Excretion: Urea is transported via the blood to the kidneys and excreted in urine, maintaining nitrogen balance in the body.
🧠 Key Points:
- Function: Detoxifies ammonia from excess amino acids.
- Importance: Prevents toxic accumulation of nitrogenous waste in the body.
Structure of the Human Kidney
📌 Overview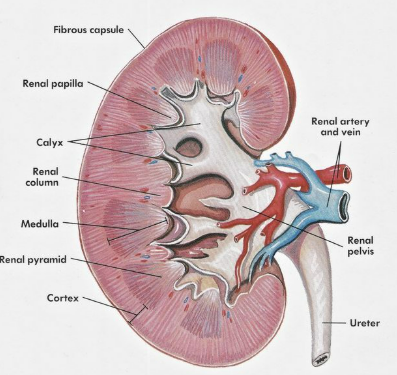
- The kidney is a bean-shaped organ responsible for filtering blood, removing waste, and maintaining water and ion balance.
- Key structures include the fibrous capsule, cortex, medulla, renal pelvis, ureter, and blood vessels.
🌱 Key Structures
| Structure | Description & Function |
|---|---|
| Fibrous capsule | Tough outer layer that protects the kidney from damage and infection. |
| Cortex | Outer region beneath the capsule; contains glomeruli and convoluted tubules where filtration and selective reabsorption occur. |
| Medulla | Inner region; contains renal pyramids and loops of Henle for concentration of urine. |
| Renal pelvis | Funnel-shaped cavity that collects urine from medulla and directs it into the ureter. |
| Ureter | Tube that transports urine from the kidney to the bladder. |
| Renal artery | Branches into smaller arterioles, supplying oxygenated blood to nephrons. |
| Renal vein | Carries deoxygenated, filtered blood away from the kidney. |
- Blood enters via the renal artery, is filtered in the cortex and medulla, and leaves via the renal vein.
- The ureter transports urine to the bladder for storage.
- The fibrous capsule provides protection, while the cortex and medulla carry out most of the filtering and concentrating functions.
Structure of a Nephron
📌 Overview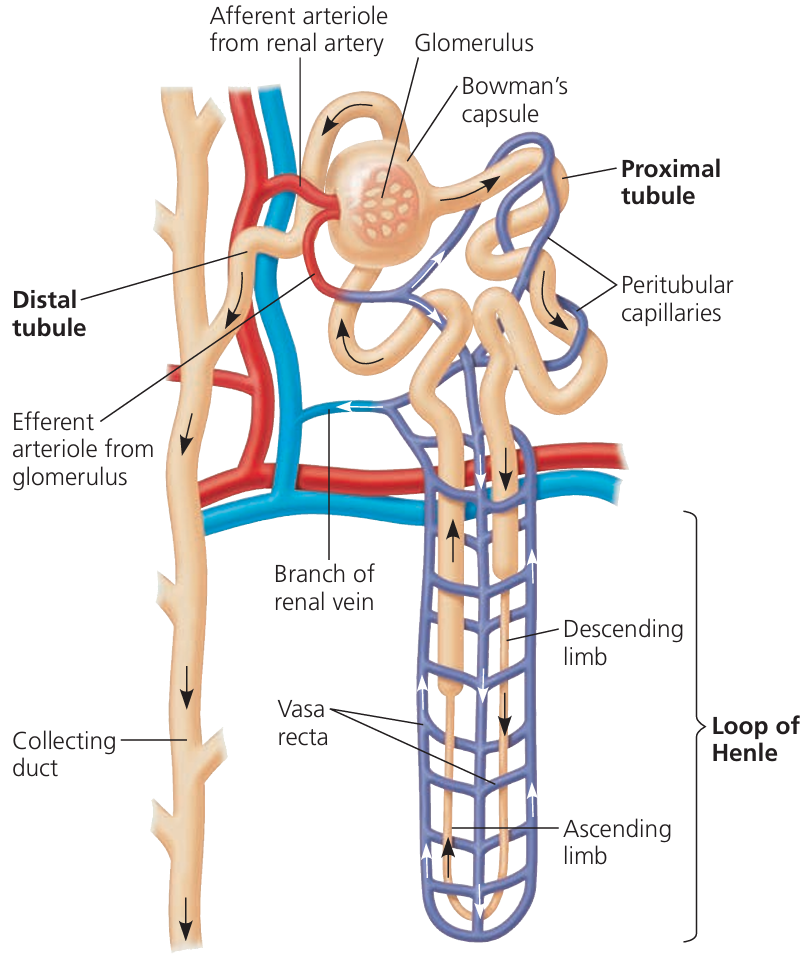
- The nephron is the functional unit of the kidney, responsible for filtration, reabsorption, and urine formation.
- Each nephron is associated with blood vessels that supply and drain blood.
🌱 Key Structures of a Nephron
| Structure | Description & Function |
|---|---|
| Glomerulus | A tuft of capillaries where blood filtration begins. |
| Bowman’s capsule | Cup-shaped structure surrounding the glomerulus; collects filtrate (water, ions, small molecules). |
| Proximal convoluted tubule (PCT) | Twisted tubule where most selective reabsorption occurs (glucose, amino acids, ions, water). |
| Loop of Henle | Hairpin-shaped loop that concentrates urine by reabsorbing water and salts; has descending and ascending limbs. |
| Distal convoluted tubule (DCT) | Twisted tubule involved in selective reabsorption of ions and pH balance. |
| Collecting duct | Collects urine from multiple nephrons; final site for water reabsorption; directs urine to the renal pelvis. |
🌱 Associated Blood Vessels
| Blood Vessel | Description & Function |
|---|---|
| Afferent arteriole | Brings blood into the glomerulus for filtration. |
| Efferent arteriole | Carries blood away from glomerulus; forms peritubular capillaries. |
| Peritubular capillaries / vasa recta | Surround nephron tubules; site of reabsorption and secretion between blood and nephron. |
🧠 Key Points:
- Each nephron is closely associated with blood vessels, ensuring efficient exchange of substances.
- Filtration occurs in the glomerulus/Bowman’s capsule, while tubules and collecting duct modify filtrate into urine.
- Electron micrographs and photomicrographs help identify fine structures such as podocytes in Bowman’s capsule or microvilli in the PCT.
Urine Formation in the Nephron
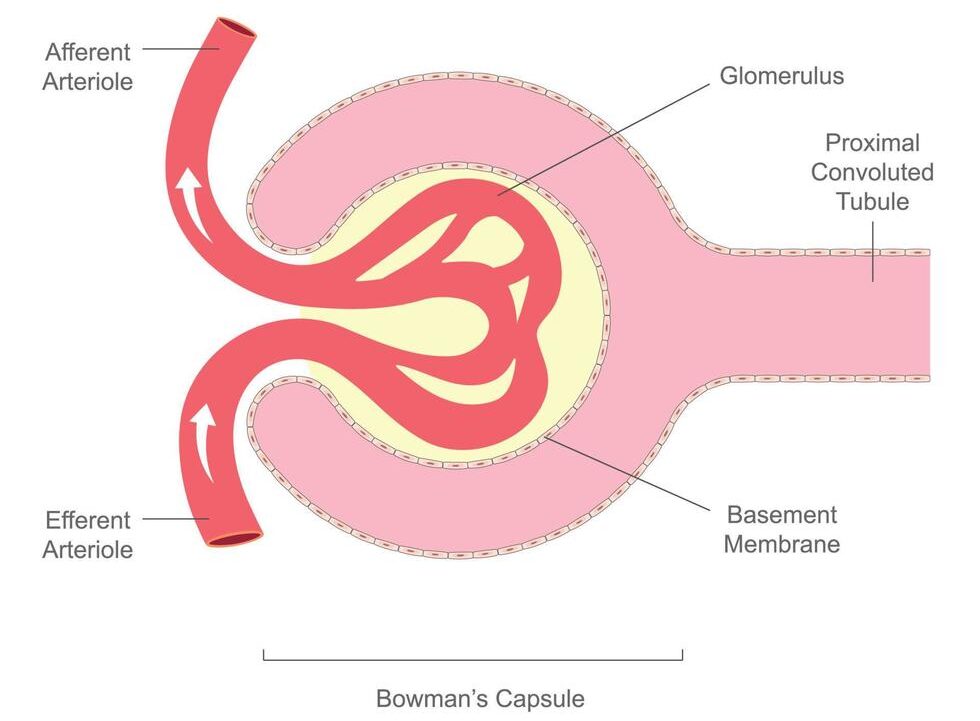
1️⃣ Formation of Glomerular Filtrate (Ultrafiltration in Bowman’s Capsule)
- Process: Blood enters the glomerulus (capillary knot) under high pressure due to the afferent arteriole being wider than the efferent arteriole.
- This high hydrostatic pressure forces small molecules out of blood into the Bowman’s capsule.
- Ultrafiltration occurs through:
- Fenestrations in capillary walls (tiny pores).

- Basement membrane (acts as a selective filter, preventing large molecules like proteins and blood cells).
- Podocytes (specialized cells with filtration slits that prevent large molecules from passing).
- Fenestrations in capillary walls (tiny pores).
- Substances filtered (filtrate contains): Water, Glucose, Amino acids, Urea, Salts (Na⁺, Cl⁻, etc.)
- Not filtered (remain in blood): Proteins (too large), Blood cells
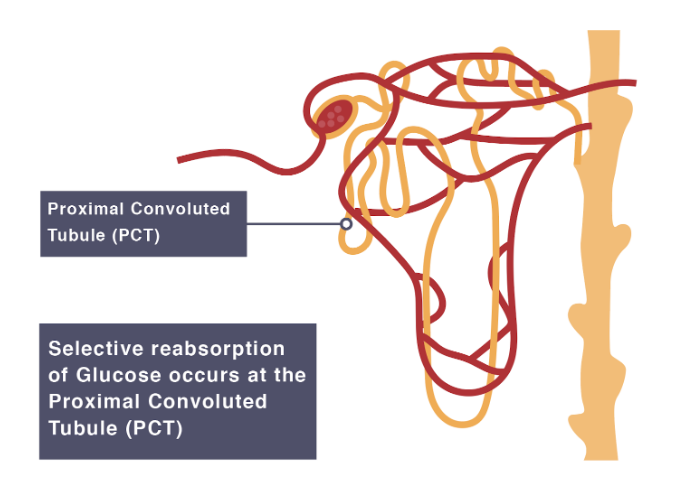
2️⃣ Selective Reabsorption in the Proximal Convoluted Tubule (PCT)
- Around 80% of the filtrate is reabsorbed here.
- Epithelial cell adaptations:
- Microvilli → large surface area for absorption.
- Mitochondria → provide ATP for active transport.
- Carrier proteins & co-transporters → allow selective uptake.
- Mechanism of Reabsorption:
- Glucose & amino acids: Active transport & co-transport with Na⁺ ions.
- Water: Osmosis (follows solute reabsorption).
- Ions (Na⁺, Cl⁻, K⁺, HCO₃⁻): Active transport & facilitated diffusion.
- Urea: Some passively reabsorbed (due to water movement).
- Filtrate leaving PCT: mainly water, urea, and some ions.
🌟 Summary Table
| Stage | Location | Process | Substances Reabsorbed/Filtered |
|---|---|---|---|
| Ultrafiltration | Glomerulus → Bowman’s capsule | High pressure filtration | Small molecules (water, glucose, amino acids, salts, urea) |
| Selective Reabsorption | Proximal Convoluted Tubule | Active transport, diffusion, osmosis | Glucose, amino acids, most water, most ions |
📌 Key Idea:
- Ultrafiltration: Non-selective filtration of small molecules.
- Selective Reabsorption: Ensures useful substances (glucose, amino acids, most water, ions) return to blood, while waste (urea) stays in filtrate.
Structure and Function of Bowman’s Capsule & PCT in Urine Formation
1. Bowman’s Capsule (Ultrafiltration)
Structure
- Cup-shaped structure surrounding the glomerulus.
 Inner layer of podocytes: specialized epithelial cells with foot-like projections (pedicels) that leave filtration slits.
Inner layer of podocytes: specialized epithelial cells with foot-like projections (pedicels) that leave filtration slits.- Basement membrane between capillaries and capsule wall acts as a selective barrier.
- Glomerulus capillaries: fenestrated (tiny pores).
- Afferent arteriole wider than efferent arteriole → creates high hydrostatic pressure.
Function
- Ultrafiltration:
- High pressure forces small molecules out of blood into the capsule.
- Fenestrations allow plasma components (water, glucose, amino acids, salts, urea) through but block large proteins and cells.
- Basement membrane ensures only molecules below a certain size pass.
- Podocyte slits prevent large proteins escaping, while maintaining permeability to small solutes.
- Result: Formation of glomerular filtrate (like plasma but without proteins).
2. Proximal Convoluted Tubule (PCT) (Selective Reabsorption)
Structure
- Highly coiled tubule → increases surface area.

- Epithelium made of cuboidal cells with:
- Microvilli (brush border) → massive surface area for absorption.
- Numerous mitochondria → provide ATP for active transport.
- Tight junctions between cells → prevent leakage of reabsorbed materials back into filtrate.
- Carrier proteins & co-transporters in membranes → allow selective reabsorption.
Function
- Selective reabsorption of useful substances:
- Glucose & amino acids → actively transported (co-transport with Na⁺).
- Na⁺ & Cl⁻ ions → reabsorbed by active transport & facilitated diffusion.
- Water → follows solute reabsorption by osmosis.
- HCO₃⁻ ions → reabsorbed for pH regulation.
- Some urea also reabsorbed passively (follows water).
- Result: ~80% of filtrate (water, glucose, amino acids, ions) is reabsorbed into blood, leaving filtrate with mainly urea, excess salts & water.
🌟 Summary Table
| Structure | Special Adaptations | Function in Urine Formation |
|---|---|---|
| Bowman’s Capsule | Podocytes with filtration slits; basement membrane; fenestrated capillaries; high pressure from arteriole size difference | Ultrafiltration – filters blood to form glomerular filtrate (excludes proteins & cells) |
| PCT | Microvilli (large SA); many mitochondria (ATP supply); tight junctions; carrier proteins & co-transporters | Selective reabsorption of glucose, amino acids, ions, water into blood |
📌 Key Idea:
Bowman’s capsule → designed for high-pressure filtration.
PCT → designed for efficient reabsorption of useful solutes and water.
Osmoregulation in Humans
🧠 Hypothalamus
- Contains osmoreceptors that monitor the water potential of blood plasma.
- If water potential falls (blood too concentrated): osmoreceptors shrink → stimulate nerve cells.
- If water potential rises (blood too dilute): osmoreceptors swell → reduce stimulation.
- Acts as the control centre for osmoregulation.
Posterior Pituitary Gland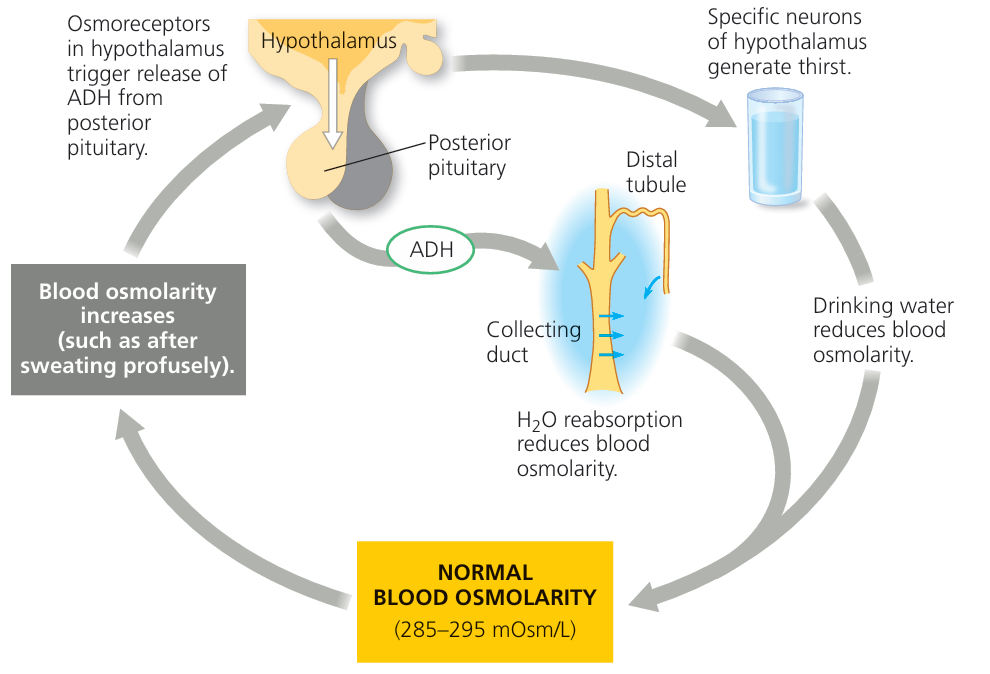
- Connected to hypothalamus by neurosecretory cells.
- When stimulated by hypothalamus → secretes antidiuretic hormone (ADH) into bloodstream.
Antidiuretic Hormone (ADH)
- A peptide hormone.
- Targets cells of the collecting ducts (and distal convoluted tubule).
- Binds to receptors on cell membranes → activates cAMP (second messenger).
- Stimulates insertion of aquaporins into membranes.
Aquaporins
- Protein channels allowing facilitated diffusion of water.
- Inserted into collecting duct cell membranes in response to ADH.
- More aquaporins = more water reabsorbed into blood.
🧪 Collecting Ducts
- With ADH: highly permeable → water reabsorbed → small volume, concentrated urine.
- Without ADH: impermeable → little reabsorption → large volume, dilute urine.
🌟 Overall Process
| Condition | ADH secretion | Aquaporins in collecting duct | Urine produced |
|---|---|---|---|
| Low water potential (dehydration) | High | Many | Small volume, concentrated |
| High water potential (excess water) | Low | Few/none | Large volume, dilute |
📌 Key Idea:
Osmoregulation is a negative feedback system:
• Hypothalamus detects water potential of blood.
• Posterior pituitary adjusts ADH secretion.
• ADH regulates aquaporins in collecting duct.
• Water reabsorption adjusts to restore balance.
Principles of Cell Signalling: Glucagon Example
1. Binding of Hormone to Receptor
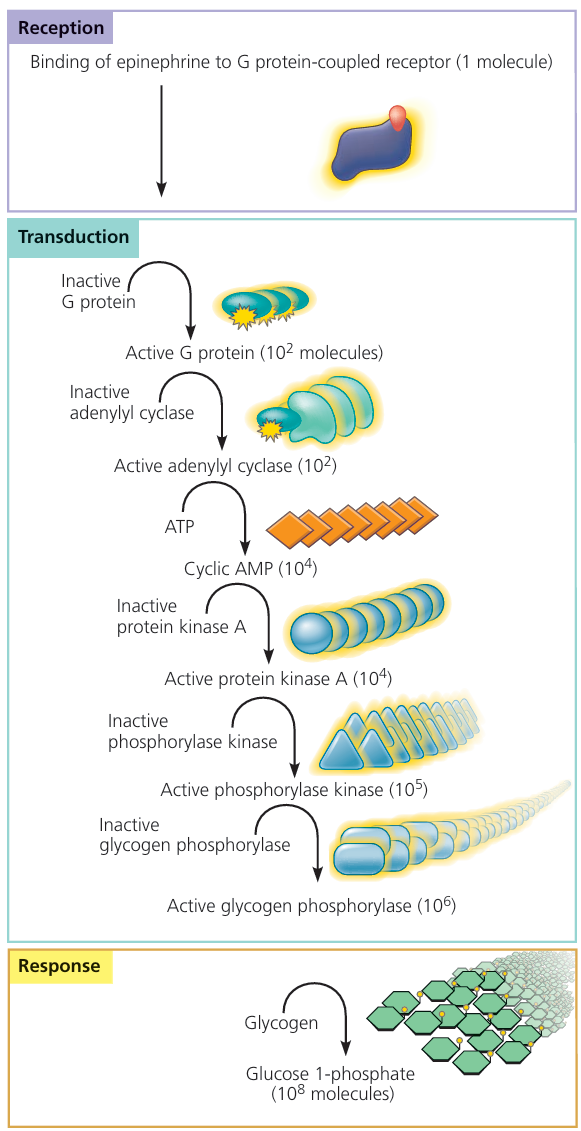
- Glucagon is a peptide hormone released from pancreatic α-cells when blood glucose is low.
- Binds to a specific receptor on the liver cell (hepatocyte) surface membrane.
- Binding causes a conformational change in the receptor protein.
2. Activation of G-Protein
- The receptor is coupled with a G-protein on the inner plasma membrane.
- Receptor change activates the G-protein.
- Active G-protein stimulates adenylyl cyclase.
3. Formation of Second Messenger (cAMP)
- Adenylyl cyclase converts ATP → cyclic AMP (cAMP).
- cAMP acts as a second messenger, transmitting the signal into the cytoplasm.
4. Activation of Protein Kinase A (PKA)
- cAMP activates protein kinase A (PKA).
- PKA phosphorylates target proteins inside the cell.
5. Enzyme Cascade (Signal Amplification)
- PKA phosphorylates and activates enzymes in a cascade.
- Each enzyme activates many molecules of the next one.
- This results in signal amplification – a small glucagon signal produces a large effect.
6. Cellular Response: Glycogen Breakdown
- The final enzyme, glycogen phosphorylase, is activated.
- It catalyses:
Glycogen → Glucose-1-phosphate → Glucose (released into blood). - Result: Increased blood glucose concentration.
🔑 Summary Flow
Glucagon → Receptor → G-Protein → Adenylyl cyclase → cAMP → Protein Kinase A → Enzyme cascade → Glycogen phosphorylase → Glucose release
✅ Key Principles of Cell Signalling:
• Specificity: Only hepatocytes with glucagon receptors respond.
• Amplification: One glucagon molecule → many glucose molecules released.
• Second messenger system: cAMP spreads the signal within the cell.
Negative Feedback Control of Blood Glucose
📌 Principle of Negative Feedback
- Definition: A control mechanism where a change in a factor (e.g., blood glucose) triggers a response to bring it back to normal.
- Normal blood glucose: ~90 mg/100 ml (5 mmol/L).
- Controlled by hormones insulin and glucagon, secreted by the islets of Langerhans in the pancreas.
1. When Blood Glucose is Too High (Hyperglycaemia)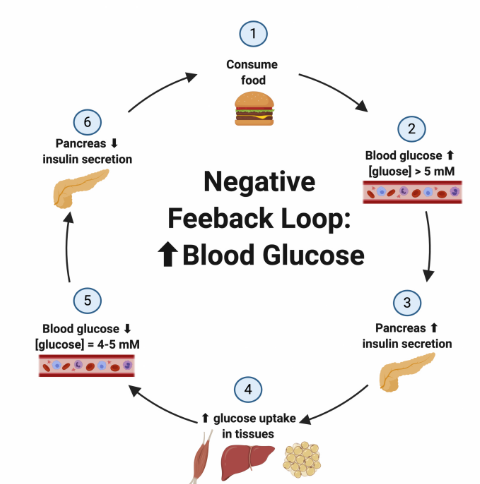
- Detected by: β-cells (beta cells) in the pancreas.
- Response: Secretion of insulin.
Effect of Insulin
- Muscle cells:
- Increases glucose uptake via transporters.
- Stimulates glycogenesis (glucose → glycogen).
- Increases glucose respiration.
- Liver cells (hepatocytes):
- Stimulates glycogenesis (storage of glucose).
- Inhibits glycogenolysis and gluconeogenesis.
👉 Result: Blood glucose falls back to normal.
2. When Blood Glucose is Too Low (Hypoglycaemia)
- Detected by: α-cells (alpha cells) in the pancreas.
- Response: Secretion of glucagon.
Effect of Glucagon (on liver cells only)
- Stimulates glycogenolysis (glycogen → glucose).
- Stimulates gluconeogenesis (from amino acids/fats).
- Inhibits glycogenesis (stopping further storage).
👉 Result: Blood glucose rises back to normal.
🔁 Negative Feedback Summary
| Condition | Hormone | Target Cells | Effect | Outcome |
|---|---|---|---|---|
| High blood glucose | Insulin (β-cells) | Muscle + Liver | ↑ Glucose uptake, ↑ Glycogenesis, ↓ Gluconeogenesis | Glucose ↓ to normal |
| Low blood glucose | Glucagon (α-cells) | Liver only | ↑ Glycogenolysis, ↑ Gluconeogenesis, ↓ Glycogenesis | Glucose ↑ to normal |
📊 Key Idea:
• Insulin and glucagon work antagonistically (opposite effects).
• Negative feedback ensures blood glucose remains stable despite diet or activity changes.
Principles of Operation of Test Strips & Biosensors for Glucose
📌 Test Strips for Glucose (Urine/Blood)
- Enzyme used: Glucose oxidase (GOx).
- How it works:
- GOx catalyses oxidation of glucose → gluconolactone, producing hydrogen peroxide (H₂O₂).
- Peroxidase enzyme uses H₂O₂ to oxidise a colourless dye → coloured compound.
- Colour intensity ∝ glucose concentration.
- User compares strip colour with a standard chart.
Limitation: Provides only an approximate, semi-quantitative result (not precise).
📌 Biosensors for Blood Glucose
Used in clinical devices (e.g., glucose meters for diabetics). Work in three stages:
1. Recognition: GOx enzyme binds specifically to glucose in the blood sample, producing H₂O₂ and/or electrons.
2. Transduction: A transducer (usually an electrode) detects the electrons or chemical change and converts it into an electrical signal.
3. Processing: The signal is amplified and processed by a microprocessor → digital display shows exact glucose concentration.
🔎 Key Differences
| Feature | Test Strips | Biosensors |
|---|---|---|
| Enzymes used | Glucose oxidase + Peroxidase | Glucose oxidase |
| Output | Colour change (compared to chart) | Digital readout |
| Accuracy | Semi-quantitative (approximate) | Quantitative (precise) |
| Use | Quick home test, urine samples | Blood glucose monitoring for diabetics |
✅ Summary:
• Both methods rely on glucose oxidase enzyme.
• Test strips → colour change (approximate).
• Biosensors → electrochemical detection (accurate, quantitative).