CIE AS/A Level Biology -15.1 Control and coordination in mammals- Study Notes- New Syllabus
CIE AS/A Level Biology -15.1 Control and coordination in mammals- Study Notes- New Syllabus
Ace A level Biology Exam with CIE AS/A Level Biology -15.1 Control and coordination in mammals- Study Notes- New Syllabus
Key Concepts:
- describe the features of the endocrine system with reference to the hormones ADH, glucagon and insulin (see 14.1.8, 14.1.9 and 14.1.10)
- compare the features of the nervous system and the endocrine system
- describe the structure and function of a sensory neurone and a motor neurone and state that intermediate neurones connect sensory neurones and motor neurones
- outline the role of sensory receptor cells in detecting stimuli and stimulating the transmission of impulses in sensory neurones
- describe the sequence of events that results in an action potential in a sensory neurone, using a chemoreceptor cell in a human taste bud as an example
- describe and explain changes to the membrane potential of neurones, including:
• how the resting potential is maintained
• the events that occur during an action potential
• how the resting potential is restored during the refractory period - describe and explain the rapid transmission of an impulse in a myelinated neurone with reference to saltatory conduction
- explain the importance of the refractory period in determining the frequency of impulses
- describe the structure of a cholinergic synapse and explain how it functions, including the role of calcium ions
- describe the roles of neuromuscular junctions, the T-tubule system and sarcoplasmic reticulum in stimulating contraction in striated muscle
- describe the ultrastructure of striated muscle with reference to sarcomere structure using electron micrographs and diagrams
- explain the sliding filament model of muscular contraction including the roles of troponin, tropomyosin, calcium ions and ATP
Endocrine System & Hormone Examples
🌟 General Features of the Endocrine System
- The endocrine system is made up of glands and cells that secrete hormones directly into the bloodstream.
- Hormones are chemical messengers that travel in blood to target cells with specific receptors.
- Key features:
- Hormones act at low concentrations but produce large effects (signal amplification).
- They produce slower, longer-lasting responses compared to the nervous system.
- Hormone secretion is usually regulated by negative feedback to maintain homeostasis.
📌 Hormone Examples
1. Antidiuretic Hormone (ADH)
- Secreted by: Posterior pituitary gland (produced by hypothalamus).
- Target: Collecting ducts of kidneys.
- Action: Increases water reabsorption by inserting aquaporins into collecting duct membranes.
- Feature shown: Endocrine control of osmoregulation.
2. Insulin
- Secreted by: β-cells of the islets of Langerhans (pancreas).
- Target: Liver, muscle, fat cells.
- Action: Increases glucose uptake, stimulates glycogenesis (glucose → glycogen), lowers blood glucose.
- Feature shown: Negative feedback to control blood glucose homeostasis.
3. Glucagon
- Secreted by: α-cells of the islets of Langerhans (pancreas).
- Target: Liver cells.
- Action: Stimulates glycogenolysis and gluconeogenesis, raising blood glucose levels.
- Feature shown: Negative feedback during low blood glucose conditions.
📊 Summary Table
| Hormone | Source | Target | Effect | Role in Homeostasis |
|---|---|---|---|---|
| ADH | Posterior pituitary | Kidney collecting ducts | ↑ Water reabsorption | Maintains water balance (osmoregulation) |
| Insulin | Pancreatic β-cells | Liver, muscle, fat | ↓ Blood glucose (↑ uptake, ↑ glycogenesis) | Maintains glucose levels (high → normal) |
| Glucagon | Pancreatic α-cells | Liver | ↑ Blood glucose (↑ glycogenolysis, ↑ gluconeogenesis) | Maintains glucose levels (low → normal) |
✅ In short:
The endocrine system maintains homeostasis using hormones like:
• ADH → water balance
• Insulin → lowers blood glucose
• Glucagon → raises blood glucose
Each hormone acts on specific target cells via the bloodstream and is controlled by negative feedback.
Nervous System vs. Endocrine System
🌟 Similarities
- Both are involved in coordination and control of body functions.
- Both rely on communication between cells.
- Both help maintain homeostasis.
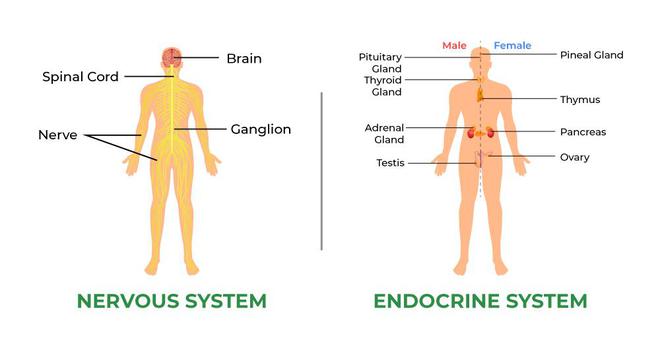
📊 Comparison Table
| Feature | Nervous System | Endocrine System |
|---|---|---|
| Mode of transmission | Electrical impulses (neurones) + neurotransmitters at synapses | Hormones transported in blood |
| Speed of response | Very fast (milliseconds) | Slower (seconds to hours, sometimes days) |
| Duration of effect | Short-lived | Long-lasting |
| Specificity | Impulses travel to specific target cells via neurones | Hormones reach all cells, but act only on target cells with receptors |
| Type of response | Immediate, rapid, short-term (e.g. reflexes, muscle contraction) | Gradual, long-term (e.g. growth, metabolism, osmoregulation) |
| Examples | Reflex arc, movement, pain response | Insulin regulating glucose, ADH regulating water balance |
| Energy use | High (neuronal firing requires ATP) | Relatively low (hormones secreted in small amounts) |
📌 Summary:
• Nervous system → fast, precise, short-term control.
• Endocrine system → slower, widespread, long-term regulation.
• Both systems work together to maintain homeostasis.
Structure & Function of Neurones
Sensory Neurone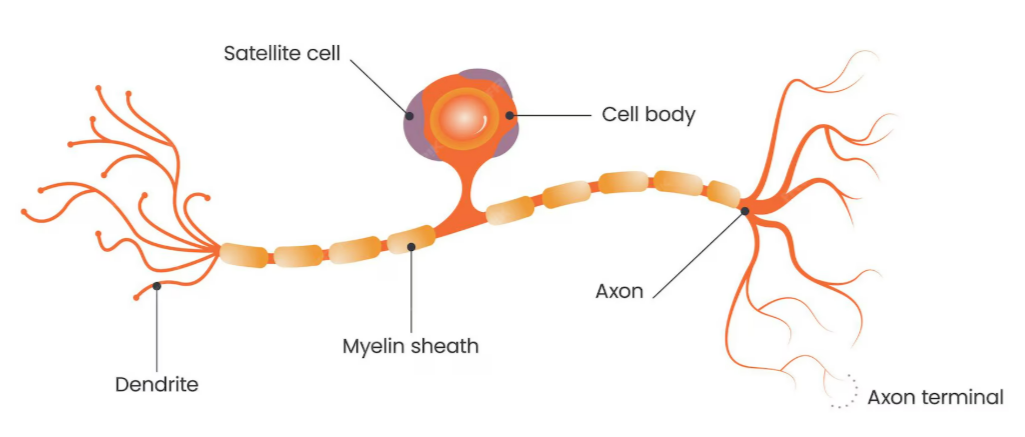
Structure
- Cell body: Located off to the side of the axon.
- Dendrites: Receive impulses from receptors (e.g. in skin, eyes, ears).
- Long dendron: Carries impulse towards cell body.
- Axon: Carries impulse away from cell body to the CNS.
- Myelin sheath: Insulates axon → speeds up transmission.
Function
- Transmits electrical impulses from sensory receptors to the CNS (spinal cord/brain).
Motor Neurone
Structure
- Cell body: Located at one end of the neurone, inside the CNS.
- Many dendrites: Receive impulses from other neurones.
- Long axon: Extends out of CNS to effectors.
- Myelin sheath: Insulates axon → faster conduction.
- Axon terminals: Synapse with muscles or glands (effectors).
Function
- Transmits impulses from CNS to effectors (muscles → contraction, glands → secretion).
Intermediate / Relay Neurone
- Found within CNS.
- Connects sensory neurones to motor neurones.
- Usually short, unmyelinated axons.
- Allows integration & coordination of responses.
📊 Comparison Table
| Feature | Sensory Neurone | Motor Neurone |
| Direction of impulse | Receptor → CNS | CNS → Effector |
| Cell body position | Side branch of axon (outside CNS, in dorsal root ganglion) | Inside CNS, at one end |
| Function | Detects and transmits sensory info | Sends commands to muscles/glands |
| Connection | Connects with relay neurones | Connects with effectors |
✅ Key Point:
Sensory neurones bring information into the CNS.
Motor neurones carry commands out of the CNS.
Relay neurones link them inside the CNS.
Role of Sensory Receptor Cells
👁️ What are Sensory Receptors?
- Specialised cells or nerve endings that detect changes in the environment (stimuli).
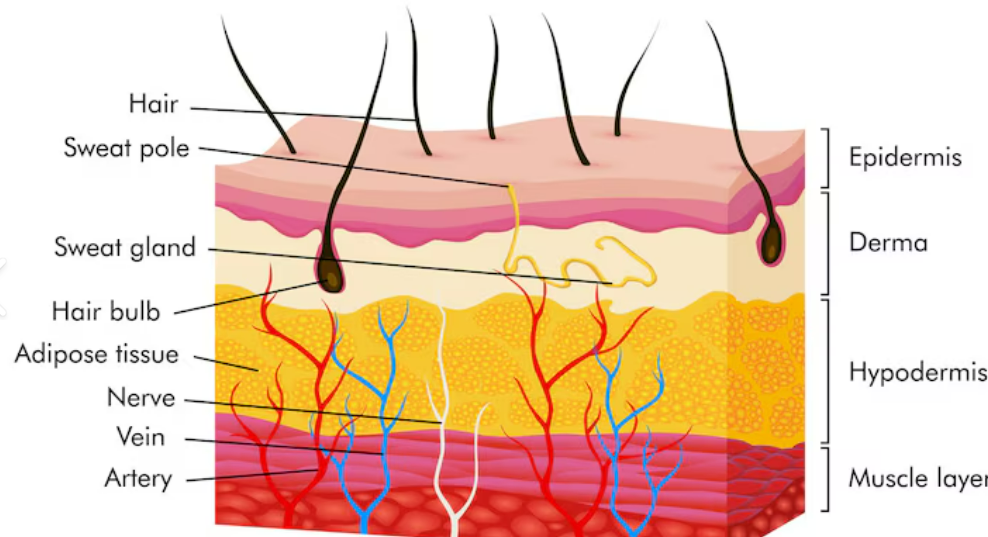
- Located in sense organs (eyes, ears, skin, nose, tongue).
- Each receptor is specific to one type of stimulus (e.g., light, pressure, chemicals, temperature).
⚡ How They Work
Detection of Stimulus
- Receptor proteins detect a specific form of energy (e.g., light, vibration, pressure).
Transduction
- Stimulus energy is converted into an electrical signal (generator potential / receptor potential).
Threshold & Action Potential
- If generator potential reaches threshold, an action potential is triggered in the sensory neurone.
- This is an all-or-nothing response → stronger stimuli = higher frequency of impulses, not larger ones.
Transmission
- Action potential is carried along the sensory neurone to the CNS for processing.
🔬 Examples of Receptors
| Receptor Type | Stimulus Detected | Location | Example |
| Photoreceptors | Light | Retina (eye) | Rods & cones |
| Mechanoreceptors | Pressure, vibration, sound | Skin, inner ear | Pacinian corpuscle |
| Chemoreceptors | Chemicals (taste, smell) | Nose, tongue | Olfactory cells, taste buds |
| Thermoreceptors | Temperature | Skin, hypothalamus | Hot & cold receptors |
📌 Summary
Sensory receptors detect stimuli.
Convert energy into electrical signals.
Generate action potentials in sensory neurones.
Send signals to CNS for interpretation → leading to a response.
Sequence of Events Leading to an Action Potential (Chemoreceptor in Taste Buds)
1. Stimulus Detection
- A chemical stimulus (e.g., sugar or salt molecules) dissolves in saliva.
- These chemicals bind to chemoreceptor proteins in the taste bud receptor cell membrane.
2. Generator Potential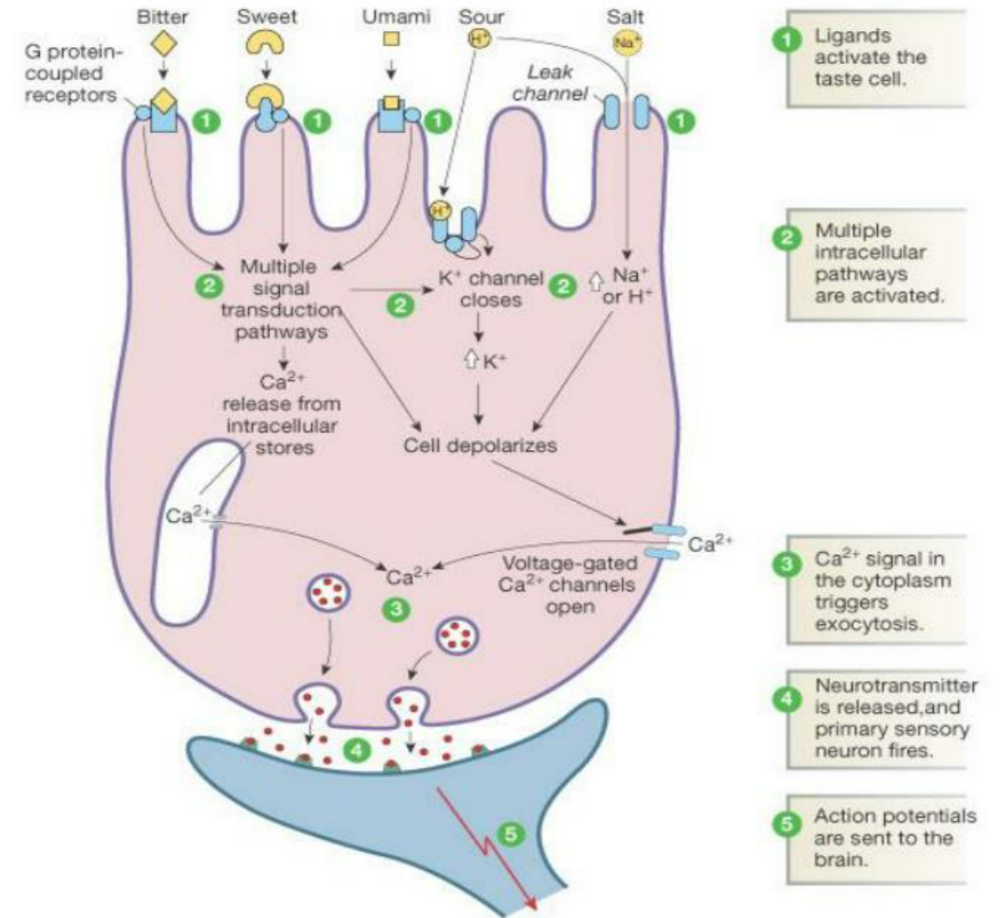
- Binding of the chemical opens ion channels in the receptor cell membrane.
- Sodium (Na⁺) or hydrogen ions (H⁺) enter the receptor cell.
- This causes depolarisation (inside becomes less negative).
- If depolarisation is large enough → a generator potential is produced.
3. Threshold Reached
- If the generator potential reaches the threshold value:
- Voltage-gated sodium channels in the sensory neurone open.
- A full action potential is triggered.
4. Action Potential Propagation
- Sodium ions flood into the neurone → rapid depolarisation.
- The action potential is conducted along the sensory neurone axon towards the CNS.
- The strength of the stimulus is coded by the frequency of action potentials, not their size.
📌 Summary
Chemical stimulus binds → ion channels open.
Ion influx depolarises receptor → generator potential.
Threshold reached → action potential triggered.
Action potential travels to CNS → interpreted as taste.
Changes in Membrane Potential of Neurones
1. Resting Potential (–70 mV)
- The neurone membrane is polarised.
- Maintained by the sodium–potassium pump and membrane permeability:
- Pumps 3 Na⁺ ions out and 2 K⁺ ions in (active transport using ATP).
- Membrane is more permeable to K⁺ than Na⁺ → more positive ions leave than enter.
- Inside of the axon becomes negatively charged relative to outside (–70 mV).
- This creates the resting potential, ready for excitation.
2. Events of an Action Potential
- a) Depolarisation (Stimulus):
- Stimulus causes Na⁺ channels to open.
- Na⁺ rushes into axon (down electrochemical gradient).
- Membrane potential becomes less negative.
- If threshold (≈ –55 mV) is reached → full action potential triggered.
- b) Rising Phase:
- More Na⁺ channels open (positive feedback).
- Rapid Na⁺ influx makes inside of axon positive (+30 mV).
- c) Repolarisation:
- At +30 mV, Na⁺ channels close.
- K⁺ channels open, K⁺ diffuses out of axon.
- This restores negative charge inside.
- d) Hyperpolarisation:
- Too many K⁺ ions leave → membrane becomes more negative than resting (below –70 mV).
3. Refractory Period (Restoration of Resting Potential)
- Na⁺ channels cannot open immediately → ensures one-way transmission of impulses.
- Sodium–potassium pump restores original ion balance:
- Pumps Na⁺ back out and K⁺ back in.
- Membrane potential returns to resting –70 mV.
- Resting potential: maintained by Na⁺/K⁺ pump.
- Depolarisation: Na⁺ influx.
- Repolarisation: K⁺ efflux.
- Hyperpolarisation: overshoot.
- Refractory period: restores resting potential.
Rapid Transmission of an Impulse in a Myelinated Neurone (Saltatory Conduction)
Structure of a Myelinated Neurone
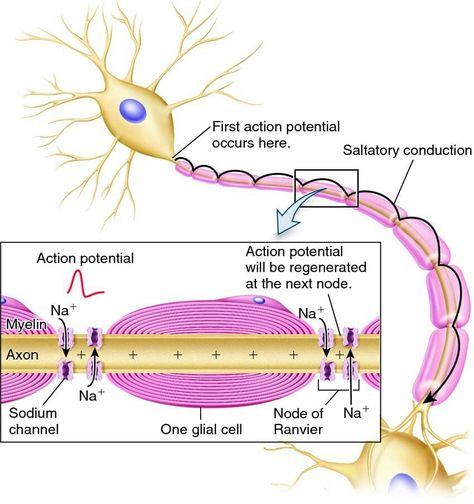
- Myelin sheath: layers of lipid membrane formed by Schwann cells.
- Nodes of Ranvier: small gaps (2–3 µm) between adjacent Schwann cells where the axon membrane is exposed.
- Ion channels concentrated only at the nodes, not along myelinated sections.
Saltatory Conduction (Jumping Conduction)
- In myelinated neurones, depolarisation occurs only at the nodes of Ranvier.
- Action potential jumps from node to node rather than moving continuously along the axon.
- Between nodes, the myelin prevents ion movement → speeding transmission.
🔍 Why It Is Faster
- Fewer depolarisation events → less time required.
- Local currents travel further under myelin before needing to regenerate an action potential.
- Uses less ATP as fewer Na⁺/K⁺ pump operations are needed.
📊 Comparison: Myelinated vs. Non-myelinated Neurone
| Feature | Myelinated Neurone | Non-myelinated Neurone |
|---|---|---|
| Speed of transmission | Fast (up to 120 m/s) due to saltatory conduction | Slow (≈ 2 m/s), impulse moves continuously |
| Energy use | Lower (fewer ion pumps active) | Higher (more continuous pumping) |
| Impulse conduction | Jumps node to node | Continuous along entire axon |
| Found in | Vertebrates, longer axons | Many invertebrates, short axons |
Importance of the Refractory Period in Determining the Frequency of Impulses
🧩 What is the Refractory Period?
- The short time (≈ 2–10 ms) after an action potential when a neurone cannot immediately fire another action potential.
- Two phases:
- Absolute refractory period: no new impulse can be generated (Na⁺ channels inactivated).
- Relative refractory period: a stronger-than-normal stimulus is required (K⁺ channels still open, membrane hyperpolarised).
⚡ Importance in Controlling Impulse Frequency
- Limits maximum frequency: ensures impulses cannot follow each other too closely → sets an upper limit to how fast neurones can fire.
- Prevents overlap of action potentials: each impulse remains a separate, discrete event.
- Prevents bidirectional impulses: ensures impulses travel in one direction only along the axon.
- Stimulus strength coding:
- Stronger stimuli = more frequent impulses (up to maximum, limited by refractory period).
- Weaker stimuli = lower frequency of impulses.
📊 Summary Table
| Function of Refractory Period | Explanation |
|---|---|
| Impulse separation | Ensures each action potential is distinct. |
| One-way transmission | Stops impulses from travelling backwards. |
| Frequency coding | Limits max impulse frequency → stimulus strength encoded by frequency, not size, of impulses. |
| Restoration | Allows ion gradients (Na⁺/K⁺) to reset before next action potential. |
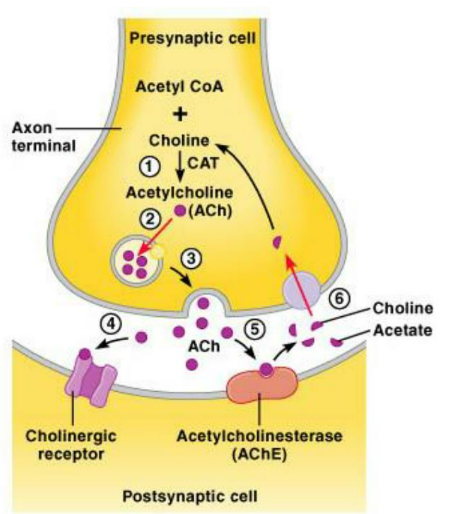
Cholinergic Synapse – Structure and Function
🧩 Structure of a Cholinergic Synapse
- A cholinergic synapse transmits impulses between neurones using the neurotransmitter acetylcholine (ACh).
- Presynaptic neurone
- Synaptic knob: swollen end of axon containing many mitochondria (ATP for neurotransmitter synthesis).
- Vesicles: contain acetylcholine.
- Voltage-gated Ca²⁺ channels: open in response to depolarisation.
 Synaptic cleft
Synaptic cleft- Tiny gap (~20–40 nm) between presynaptic and postsynaptic membranes.
- Postsynaptic neurone
- Receptors: protein receptors specific to acetylcholine, located on sodium ion channels.
- Enzyme acetylcholinesterase (AChE): located in cleft, breaks down acetylcholine.
🔄 Function of a Cholinergic Synapse
- Arrival of Impulse: Action potential reaches presynaptic knob → membrane depolarises.
- Role of Calcium Ions (Ca²⁺): Depolarisation opens voltage-gated Ca²⁺ channels → Ca²⁺ diffuses in → vesicles fuse with presynaptic membrane.
- Release of Neurotransmitter: Vesicles release acetylcholine (ACh) into synaptic cleft by exocytosis.
- Binding to Receptors: ACh diffuses across cleft → binds to receptors on postsynaptic membrane → Na⁺ channels open → depolarisation (EPSP). If threshold reached → new action potential.
- Termination of Signal: AChE breaks down ACh into choline + acetate → reabsorbed and recycled into new ACh using ATP → synapse reset, signal short-lived.
📊 Summary Table
| Step | Role of Ca²⁺ | Outcome |
|---|---|---|
| Impulse arrives | Depolarisation opens Ca²⁺ channels | Ca²⁺ enters presynaptic knob |
| Vesicle fusion | Ca²⁺ binds to proteins in vesicle membrane | Vesicles fuse with presynaptic membrane |
| Neurotransmitter release | Triggered by Ca²⁺ influx | ACh released by exocytosis |
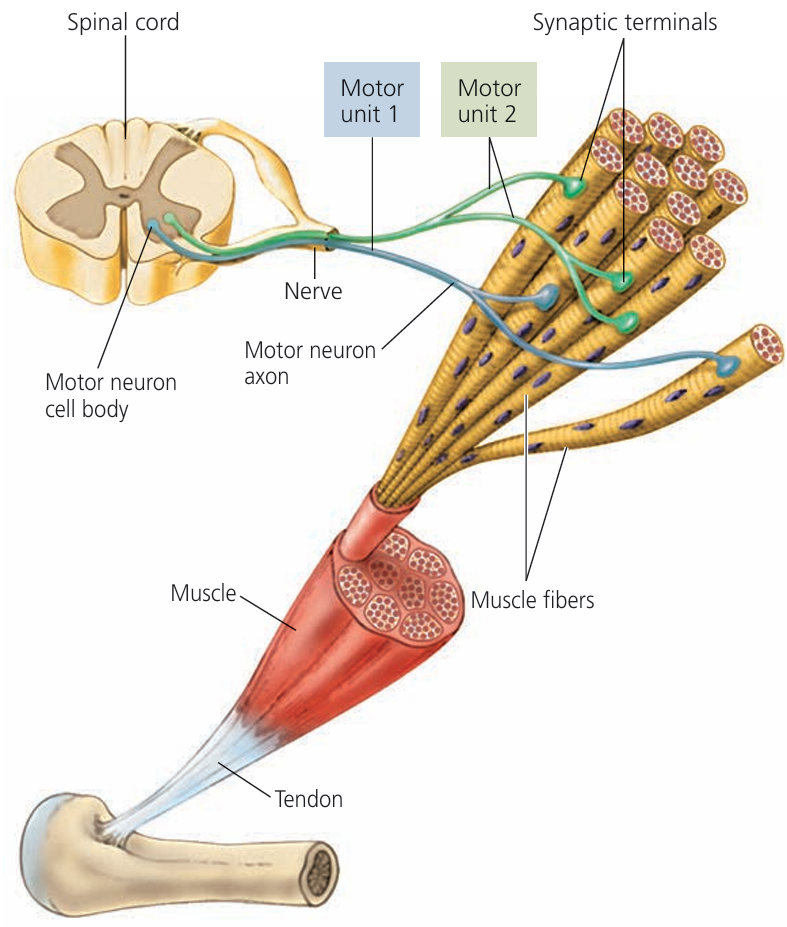
Neuromuscular Junctions, T-tubules & Sarcoplasmic Reticulum in Muscle Contraction
⚡ Neuromuscular Junction (NMJ)
- Specialised synapse between a motor neurone and a muscle fibre.
- Uses acetylcholine (ACh) as neurotransmitter.
Steps:
- Action potential arrives at motor neurone terminal → Ca²⁺ enters.
- Vesicles release ACh into synaptic cleft.
- ACh binds to receptors on sarcolemma (muscle cell membrane).
- Opens Na⁺ channels → depolarisation of sarcolemma.
- If threshold reached → action potential generated in muscle fibre.
Role: Converts nerve impulse into muscle fibre action potential.
📡 T-tubule (Transverse Tubule) System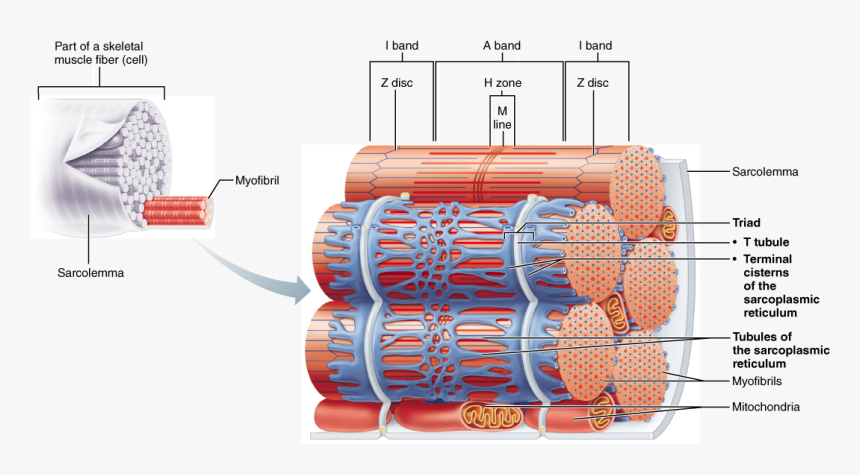
- Invaginations of sarcolemma that penetrate deep into muscle fibre.
- Carry the action potential from sarcolemma into the interior of muscle fibre.
Role: Ensures depolarisation spreads rapidly & simultaneously to all myofibrils for coordinated contraction.
🧪 Sarcoplasmic Reticulum (SR)
- Specialised smooth endoplasmic reticulum in muscle fibres.
- Stores calcium ions (Ca²⁺).
Steps:
- Action potential from T-tubules stimulates SR to open Ca²⁺ channels.
- Ca²⁺ released into sarcoplasm (cytoplasm of muscle cell).
- Ca²⁺ binds to troponin on actin filaments.
- This moves tropomyosin, exposing binding sites for myosin heads.
- Cross-bridge formation → muscle contraction.
Role: Provides the Ca²⁺ required to initiate actin–myosin interaction.
📊 Summary Table
| Structure | Function in Contraction |
|---|---|
| Neuromuscular junction | Transmits nerve impulse to muscle fibre via acetylcholine, initiating depolarisation |
| T-tubule system | Rapidly conducts action potential deep into muscle fibre for synchronous activation |
| Sarcoplasmic reticulum | Releases Ca²⁺ into sarcoplasm, triggering actin–myosin cross-bridge formation |
Ultrastructure of Striated Muscle & Sarcomere
🔬 Overview of Striated (Skeletal) Muscle
- Made up of long, multinucleate fibres containing myofibrils.
- Myofibrils are repeating units of sarcomeres (the contractile units).
- Striated appearance due to alternating light and dark bands.
📏 Sarcomere Structure (from Z-line to Z-line)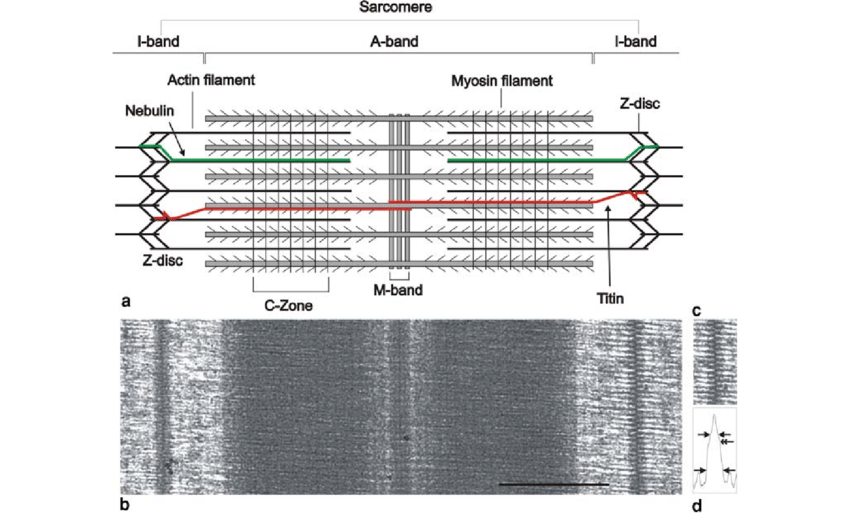
- A sarcomere = functional unit of contraction.
- Z-line (Z-disc): boundary of a sarcomere; anchors actin (thin filaments).
- M-line: centre of sarcomere; anchors myosin (thick filaments).
- A-band (dark band): entire length of thick (myosin) filaments; includes overlap with actin.
- I-band (light band): only thin (actin) filaments; spans between thick filaments.
- H-zone: central part of A-band where only myosin is present (no overlap with actin).
⚙️ Filament Arrangement
- Thin filaments (actin): Composed of actin, tropomyosin, and troponin; anchored at the Z-line.
- Thick filaments (myosin): Made of myosin molecules with projecting myosin heads; anchored at the M-line.
- Overlap of actin & myosin → cross-bridge formation during contraction.
📊 Summary Table
| Band/Line | Description | Visible in EM |
|---|---|---|
| Z-line | Boundary of sarcomere, actin anchored | Dark thin line |
| M-line | Centre of sarcomere, myosin anchored | Thin line in H-zone |
| A-band | Myosin length (with overlap of actin) | Dark band |
| I-band | Actin only | Light band |
| H-zone | Myosin only (no overlap) | Lighter region in middle of A-band |
Sliding Filament Model of Muscle Contraction
🔬 Overview
- Explains how sarcomeres shorten → muscle contraction.
- Relies on interaction between actin (thin filaments) and myosin (thick filaments).
- Controlled by calcium ions (Ca²⁺), troponin, tropomyosin, and ATP.
⚙️ Steps in the Sliding Filament Model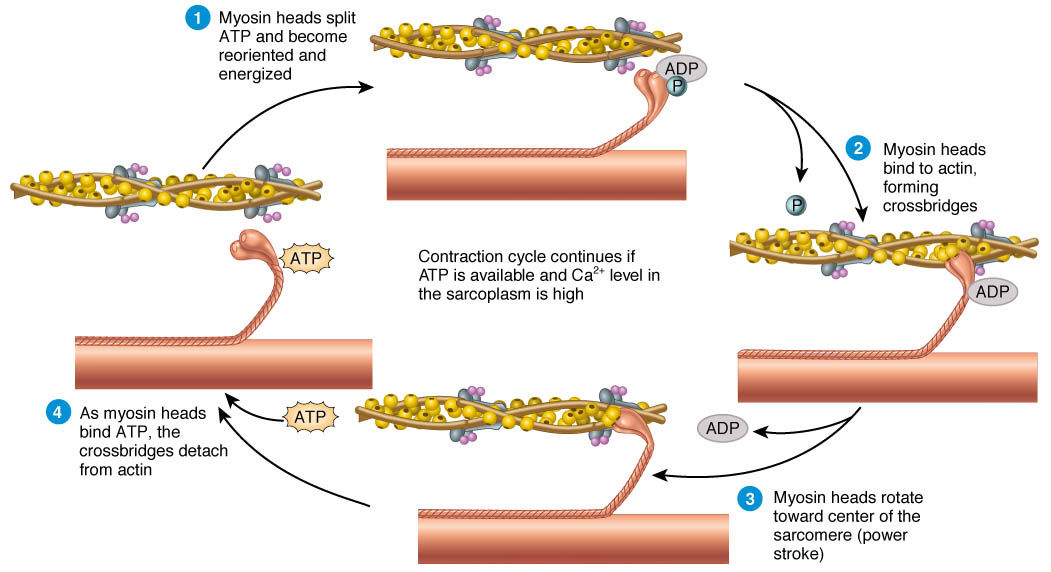
- At Rest: Tropomyosin covers actin’s binding sites → prevents cross-bridge formation. Troponin attached to tropomyosin. Myosin heads cocked (primed by ATP hydrolysis).
- Calcium Ion Release: Action potential → T-tubules → SR releases Ca²⁺. Ca²⁺ binds troponin → tropomyosin moves → actin binding sites exposed.
- Cross-Bridge Formation: Myosin head (ADP + Pi) binds to actin → cross-bridge forms.
- Power Stroke: Myosin head tilts, pulling actin towards M-line. ADP + Pi released → energy from ATP hydrolysis moves actin. Sarcomere shortens.
- Cross-Bridge Detachment: New ATP binds myosin head → detaches from actin.
- Re-cocking of Myosin Head: ATP hydrolysed → ADP + Pi. Myosin head resets, ready for next cycle.
🔁 Cycle Repeats: As long as Ca²⁺ is present and ATP available, cross-bridge cycling continues. I-band and H-zone shorten; A-band constant.
📊 Key Roles of Molecules
| Molecule | Role |
|---|---|
| Calcium ions (Ca²⁺) | Released from SR; bind troponin → expose actin binding sites |
| Troponin | Ca²⁺ binding causes shift → moves tropomyosin |
| Tropomyosin | Blocks actin’s myosin-binding sites at rest; moves when troponin changes shape |
| ATP | Energy for detachment & resetting of myosin heads; hydrolysis primes power stroke |