Edexcel A Level (IAL) Biology -6.15 Current Usage of Antibiotics- Study Notes- New Syllabus
Edexcel A Level (IAL) Biology -6.15 Current Usage of Antibiotics- Study Notes- New syllabus
Edexcel A Level (IAL) Biology -6.15 Current Usage of Antibiotics- Study Notes -Edexcel A level Biology – per latest Syllabus.
Key Concepts:
- 6.15 know how an understanding of the contributory causes of hospital-acquired infections has led to codes of practice regarding antibiotic prescription and hospital practice that relate to infection prevention and control
Hospital-Acquired Infections (HAIs) and Codes of Practice
🌱 Introduction
Hospital-acquired infections (HAIs) are infections patients pick up inside hospitals or healthcare settings. Understanding why these infections occur has directly shaped the rules hospitals now follow for antibiotics and infection control.
🦠 Main Causes of Hospital-Acquired Infections
1. Overuse and Misuse of Antibiotics
- Hospitals use many antibiotics, creating strong selection pressure.
- Resistant strains like MRSA survive and spread.
- Broad-spectrum antibiotics kill normal flora, allowing pathogens like C. difficile to grow.
2. Vulnerable Patients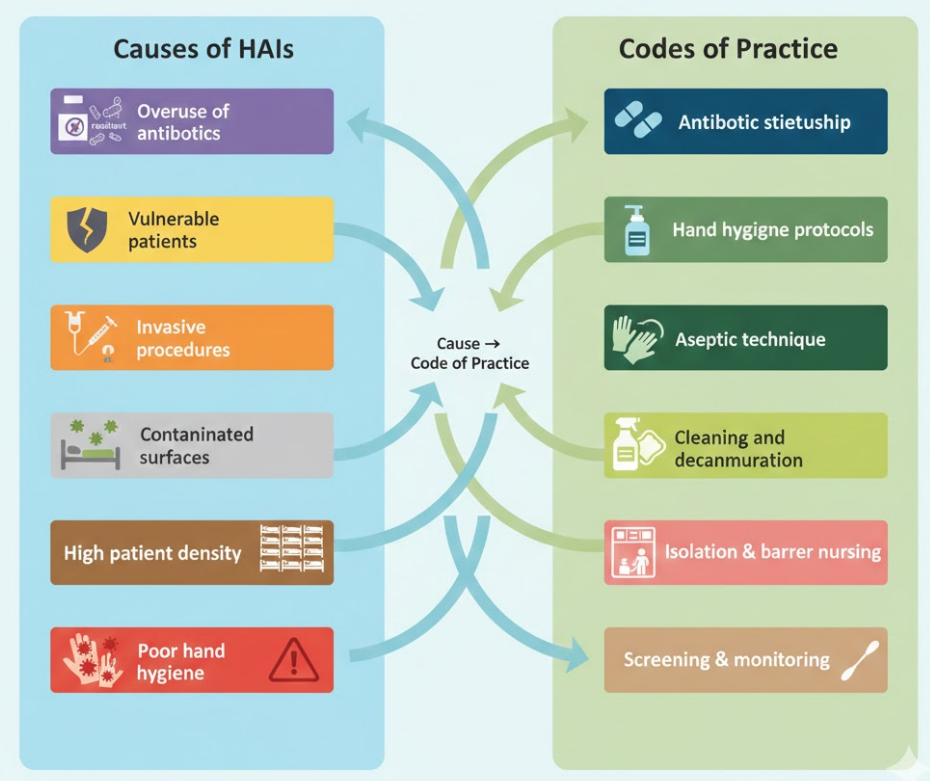
- Many patients have weak immune systems due to illness, surgery or treatments.
- They are more prone to infection and may not fight off even mild microbes.
3. Invasive Procedures
- Catheters, cannulas, ventilators and surgical wounds give microbes direct entry.
- Poor aseptic technique increases the risk.
4. Contaminated Surfaces and Equipment
- Bed rails, trolleys, stethoscopes and keyboards can hold microbes.
- Pathogens transfer between patients if cleaning is poor.
5. Poor Hand Hygiene
- The most common cause.
- Staff can move pathogens between patients if hands are not properly cleaned.
6. High Population Density
- Many patients in close proximity means rapid spread.
- Staff act as mobile carriers if precautions are not followed.
📘 How These Causes Led to Codes of Practice
A. Codes for Antibiotic Prescription (Antibiotic Stewardship)
- Prescribe antibiotics only when clearly needed.
- Use narrow-spectrum antibiotics when possible.
- Avoid unnecessary broad-spectrum drugs.
- Review prescriptions frequently and stop early if appropriate.
- Keep accurate records to track resistance patterns.
- Follow hospital stewardship teams and microbiology guidance.
Goal: Slow down resistance and reduce antibiotic-driven HAIs.
B. Codes for Infection Prevention and Control
1. Hand Hygiene
- Mandatory washing/sanitising before and after patient contact.
- Alcohol rubs placed at all ward entrances.
- WHO 7-step method used by all staff.
2. Aseptic Technique
- Use sterile gloves, sterile tools and proper skin cleaning before procedures.
- Apply aseptic non-touch technique (ANTT) for cannulas and dressings.
3. Cleaning and Decontamination
- Daily disinfection of high-contact surfaces.
- Deep cleaning of rooms after infectious patients.
- Regular sterilisation of reusable equipment.
4. Isolation and Barrier Nursing
- Separate rooms for patients with MRSA, C. difficile and resistant bacteria.
- Staff wear gowns, gloves and masks when entering isolation areas.
5. Screening and Monitoring
- Patients screened for MRSA on admission.
- Weekly infection reports to identify outbreaks early.
6. Safe Waste Disposal
- Sharps disposed in puncture-proof bins.
- Infectious waste handled separately.
📋 Summary Table
| Contributory Cause | Resulting Code of Practice |
|---|---|
| Antibiotic misuse | Antibiotic stewardship, restricted prescribing |
| Contaminated surfaces | Strict cleaning and sterilisation routines |
| Poor hand hygiene | Mandatory hand hygiene protocols |
| Invasive procedures | Aseptic technique and sterile equipment |
| Vulnerable patients | Isolation rooms, barrier nursing |
| High patient density | Screening, audit and monitoring |
HAIs spread due to resistance, poor hygiene, invasive procedures and contaminated surfaces.
These causes shaped strict rules: clean hands, clean surfaces, isolation, safe procedures and careful antibiotic use.
Aim: reduce infection rates and prevent resistant strains from spreading in hospitals.
