IB DP Biology Transport Study Notes - New Syllabus
IB DP Biology Transport Study Notes
IB DP Biology Transport Study Notes at IITian Academy focus on specific topic and type of questions asked in actual exam. Study Notes focus on IB Biology syllabus with guiding questions of
- What adaptations facilitate transport of fluids in animals and plants?
- What are the differences and similarities between transport in animals and plants?
Standard level and higher level: 3 hours
Additional higher level: 2 hours
B3.2.1 – Adaptations of Capillaries for Exchange of Materials
📌 Real-Life Examples
• Lungs: Oxygen enters blood, CO₂ exits
• Small intestine: Nutrients absorbed
• Kidneys: Blood is filtered → urine forms
Capillaries are the smallest blood vessels in the body. They connect arterioles (small arteries) to venules (small veins), and their key role is to exchange substances like oxygen, carbon dioxide, nutrients, and waste between blood and tissues (or alveoli in lungs).
✅ Key Adaptations of Capillaries for Efficient Exchange
1. Large Surface Area
- Dense capillary networks (beds) around tissues
- More area for diffusion → More exchange
2. Narrow Diameter (Lumen)
- Only one red blood cell passes at a time
- Slows flow → more time for exchange
- RBCs stay close to wall for faster diffusion
3. Thin Walls
- Made of a single layer of flattened endothelial cells
- Very short diffusion distance → fast exchange
4. Fenestrations (Pores)
- Found in kidneys, intestines, endocrine glands
- Allow rapid passage of fluid and large molecules
- Efficient in filtration and absorption
🧠 Summary Table
| Adaptation | How It Helps with Exchange |
|---|---|
| Large surface area | More room for substances to diffuse across |
| Narrow diameter | Slows blood flow and brings red blood cells close |
| Thin walls (one cell thick) | Short diffusion distance = faster exchange |
| Fenestrations (in some) | Quick movement of fluids and large molecules |
B3.2.2 – Structure of Arteries and Veins
• Artery: Thick wall, round shape, small lumen
• Vein: Thin wall, wide/irregular lumen, may have valves
• Capillary: Very small, one-cell-thick wall
Blood vessels have different structures based on their function. Arteries carry blood away from the heart, veins carry it toward the heart, and capillaries allow exchange of materials.
🩸 1. Function of Blood Vessels
| Vessel | Function |
|---|---|
| Arteries | Carry blood away from the heart |
| Veins | Carry blood into the heart |
| Capillaries | Exchange materials with tissues/lungs |

🛠️ 2. Structure and Function of Arteries
Main Role: Withstand and maintain high pressure from the heart
- Small lumen: Maintains high pressure
- Thick smooth muscle: Contracts to push blood
- Thick elastic tissue: Elastic recoil after each heartbeat
- Collagen: Prevents rupture
- No valves: Blood flows in one direction due to high pressure
🩹 3. Structure and Function of Veins
- Main Role: Return blood under low pressure to the heart

- Large lumen: Holds more blood and reduces resistance
- Thin smooth muscle: Less need to push blood
- Thin elastic tissue: Slight recoil
- Valves: Prevent backflow
- Flexible wall: Works with skeletal muscles to move blood
🔬 4. Comparing Arteries vs Veins
| Feature | Arteries | Veins |
|---|---|---|
| Direction of flow | Away from heart | Toward the heart |
| Wall thickness | Thick | Thin |
| Lumen size | Small | Large |
| Muscle layer | Thick | Thin |
| Elastic tissue | Thick | Thin |
| Valves | Absent | Present |
| Pressure | High | Low |
🔎 5. How to Identify Blood Vessels in Micrographs

Answer:

• Artery: Very thick wall, small round lumen
• Vein: Thin wall, large irregular lumen, may show valves
• Capillary: One cell thick, narrow lumen, hard to spot
🧠 Bonus Table – Slide Identification
| Feature | Artery | Vein | Capillary |
|---|---|---|---|
| Wall Thickness | Very thick | Thin | Very thin (1 cell) |
| Lumen Diameter | Narrow | Wide | Very narrow |
| Shape | Usually round | Irregular/flattened | Tiny, uniform |
| Valves visible? | No | Yes (sometimes) | No |
| Easy to identify? | Yes | Yes | Harder |
B3.2.3 – Adaptations of Arteries for Transporting Blood Away from the Heart
🧬 What are Arteries?
Arteries are blood vessels that carry blood away from the heart. They usually carry oxygenated blood, except for the pulmonary artery (which carries deoxygenated blood to the lungs).
Arteries must handle high pressure because the blood is pumped directly from the heart with great force.
🧪 Key Features of Arteries
| Feature | Structure | Function / Adaptation |
|---|---|---|
| Thick muscular walls | Smooth muscle layer | Helps control blood flow and maintain pressure by vasoconstriction (narrowing) and vasodilation (widening) |
| Elastic tissue | Elastic fibers in the middle layer (tunica media) | Allows the artery to stretch and recoil with each heartbeat-this helps to withstand and maintain high pressure |
| Narrow lumen | Small internal diameter | Increases resistance to help maintain high pressure |
| Smooth endothelium | Inner lining (tunica intima) | Reduces friction for smooth blood flow |
| No valves | Unlike veins | Arteries don’t need valves because high pressure prevents backflow |
🌿 Why Do Arteries Need to Withstand High Pressure?
Blood is pumped out of the left ventricle of the heart under very high pressure to ensure it reaches all parts of the body quickly.
If artery walls were weak or thin, they could burst or tear due to this pressure. Arteries must also maintain pressure between heartbeats (during diastole) to ensure continuous blood flow to tissues.
📌 How Elastic & Muscle Layers Help Arteries Function
- Elastic Tissue
Stretches during systole (when heart pumps)
Recoils during diastole (heart relaxation)
Acts like a pressure reservoir, helping to even out blood flow - Smooth Muscle
Contracts to narrow the lumen (vasoconstriction)
Relaxes to widen the lumen (vasodilation)
Helps control blood distribution to organs depending on their needs (e.g. during exercise)
🔍 Real-Life Example: Aorta
The aorta is the largest artery and receives blood directly from the heart. It has an especially thick wall with lots of elastic fibers to handle the surge of pressure from the left ventricle.
📊 Summary Table: Arteries vs Veins
| Feature | Arteries | Veins |
|---|---|---|
| Direction of blood flow | Away from heart | Toward the heart |
| Oxygen level | Usually oxygenated | Usually deoxygenated |
| Pressure | High | Low |
| Wall thickness | Thick and muscular | Thin |
| Elasticity | High (elastic fibers) | Low |
| Valves | No | Yes (to prevent backflow) |
| Lumen size | Narrow | Wide |
Arteries are specialized to carry high-pressure blood away from the heart.
Thick muscular and elastic walls help them withstand the pressure and maintain smooth blood flow.
Elastic tissue enables stretch and recoil, while muscle allows control over diameter and blood flow.
These adaptations are vital for efficient circulation and organ perfusion.
B3.2.4 – Measurement of Pulse Rates
🧬 What is a Pulse?
A pulse is the rhythmic throbbing of arteries as blood is pushed through them by the heart.
It reflects the heart rate – i.e., how many times the heart beats in one minute (bpm). Each pulse you feel = one heartbeat.
📍 Where Can You Feel the Pulse?
| Pulse Point | Location | Use |
|---|---|---|
| Carotid artery | Side of the neck | Often used during emergencies |
| Radial artery | Inside of the wrist (thumb side) | Most common for everyday checks |
| Brachial artery | Inner elbow | Used in infants or blood pressure |
| Femoral artery | Groin area | Used in trauma cases |
| Dorsalis pedis | Top of foot | Used to check circulation in legs |
🧪 How to Measure Pulse Manually
This is a traditional method using your fingers – no tools needed.
- Use index and middle finger (never the thumb).
- Place gently over a pulse point (radial or carotid).
- Count the beats for:
- 15 seconds, then multiply by 4
- Or 30 seconds, then multiply by 2
- Or directly for 60 seconds for more accuracy
- Result = Heart rate in bpm (beats per minute)
📌 Normal resting pulse:
Adults: 60–100 bpm
Athletes: can be as low as 40–60 bpm
🔬 Digital Methods of Measuring Pulse
| Method | How it works | Pros | Cons |
|---|---|---|---|
| Heart rate monitors | Chest straps or wristbands detect electrical signals from heart | Very accurate | May be expensive |
| Smartwatches / Fitness bands | Use PPG (light sensors) to detect blood flow | Easy to use, gives continuous data | Less accurate if worn loosely or with movement |
| Pulse oximeters | Clips onto finger and uses light to detect pulse and oxygen levels | Simple, gives two values (pulse + oxygen) | Not reliable during motion or cold fingers |
| Smartphone apps | Uses camera + flash to detect tiny changes in color in fingertip | Convenient | Less reliable, affected by lighting/position |
🧪 Manual vs Digital: Quick Comparison
| Feature | Manual (Fingertips) | Digital Devices |
|---|---|---|
| Tools Needed | Just fingers + timer | Specific device/app |
| Accuracy | Good, but human error possible | Usually high, depends on device |
| Cost | Free | Can be costly |
| Real-time tracking | No | Yes |
| Continuous monitoring | No | Yes |
| User skill needed | Some practice | Minimal |
A pulse is the outward sign of a heartbeat—best felt at carotid or radial arteries.
Manual method: simple, low-cost, requires focus.
Digital methods: easy, often more precise, but depend on device quality.
Pulse rate gives insight into heart health, fitness, and circulation.
B3.2.5 – Adaptations of Veins for Returning Blood to the Heart
🧬 What Are Veins?
Veins are blood vessels that carry blood back to the heart. Most veins carry deoxygenated blood (except the pulmonary vein, which carries oxygenated blood from lungs to heart).
Blood in veins travels under low pressure, so veins need special features to assist return flow and prevent backflow.
🌿 Key Structural Adaptations of Veins
| Adaptation | Structure | Function / Benefit |
|---|---|---|
| Valves | One-way flap-like structures inside the vein | Prevent backflow of blood, especially in limbs where blood moves against gravity |
| Thin, flexible walls | Less muscle and elastic tissue than arteries | Allows veins to be easily compressed by surrounding skeletal muscles during movement |
| Wide lumen | Larger internal diameter than arteries | Reduces resistance, helps blood flow more easily under low pressure |
| Position near muscles | Often located between large muscles | Muscle contractions squeeze veins, pushing blood upward toward the heart (called muscle pump) |
| Low elasticity | Fewer elastic fibers | Not needed as veins don’t need to stretch and recoil like arteries |
🔬 How Blood Returns to the Heart Despite Low Pressure
- Muscle Pump Mechanism: When you walk or move, skeletal muscles contract, squeezing nearby veins. This pushes blood through the veins. Valves stop it from flowing backward.
- Breathing (Respiratory Pump): During inhalation, pressure in the chest drops, helping suck blood toward the heart from the veins.
- Suction Effect of the Heart: As the heart relaxes during diastole, it creates a suction force, helping to pull blood in.
🔍 Real-World Example: Varicose Veins
Varicose veins happen when valves in leg veins fail, causing blood to pool. Veins swell and twist, often seen in people who stand for long hours. This shows the importance of valves and muscle movement in keeping venous blood flowing properly.
📊 Arteries vs Veins – Quick Comparison
| Feature | Arteries | Veins |
|---|---|---|
| Direction of flow | Away from heart | Toward heart |
| Pressure | High | Low |
| Walls | Thick, muscular | Thin, flexible |
| Valves | Absent (except pulmonary artery) | Present |
| Lumen | Narrow | Wide |
| Role of muscle | Muscle in wall | External skeletal muscles help flow |
Veins return blood to the heart under low pressure.
They have valves to prevent backflow, especially in limbs.
Thin walls and wide lumens allow blood to flow smoothly.
Surrounding muscle contractions help push blood through veins (muscle pump).
These adaptations ensure efficient venous return despite gravity and low pressure.
B3.2.6 – Causes & Consequences of Coronary Artery Occlusion
Coronary arteries are the blood vessels that supply the heart muscle (myocardium) with oxygen and nutrients. If these arteries get blocked or narrowed, the heart gets less oxygen, which can lead to serious conditions like coronary heart disease (CHD) or heart attacks.
🌿 What Is Occlusion?
Occlusion means a blockage or closing of a blood vessel. In coronary arteries, this is usually caused by a build-up of fatty deposits (atheroma) in the artery walls.
📌 Causes of Coronary Artery Occlusion
| Cause | Explanation |
|---|---|
| Atherosclerosis | Build-up of fatty plaques (mainly cholesterol) in artery walls |
| High LDL (bad) cholesterol | Leads to plaque formation |
| High blood pressure (hypertension) | Damages artery walls, increasing plaque risk |
| Smoking | Damages endothelium and promotes atheroma |
| Diabetes | High blood sugar damages vessels |
| Lack of exercise | Contributes to obesity and poor circulation |
| Diet high in saturated fats | Linked to higher LDL cholesterol |
| Genetics | Family history of heart disease increases risk |
| Age & gender | Older age and being male = higher risk |
🧪 Consequences of Coronary Artery Occlusion
| Condition | What Happens | Effect on the Body |
|---|---|---|
| Angina | Temporary narrowing of coronary artery | Chest pain during exertion |
| Myocardial Infarction (Heart Attack) | Complete blockage of a coronary artery | Heart muscle cells die from lack of oxygen |
| Heart Failure | Weakened heart can’t pump properly | Breathlessness, fatigue, fluid build-up |
| Arrhythmias | Irregular heartbeat | Can be life-threatening |
| Sudden cardiac death | Complete failure of the heart | Immediate emergency situation |
📊 Understanding & Evaluating Epidemiological Data
What Is Epidemiology?
The scientific study of patterns and causes of disease in populations. Helps identify risk factors and public health strategies.
🧠 Key Terms:
| Term | Definition |
|---|---|
| Correlation | A statistical relationship between two variables (e.g. fat intake & CHD) |
| Correlation coefficient (r) | Value between -1 and +1 that shows strength and direction of correlation |
| Causation | One factor directly causes another |
❗ Important Note: Correlation ≠ Causation. A high correlation (e.g. between saturated fat intake and CHD) doesn’t prove that one causes the other—other confounding factors (like activity level or genetics) may be involved.
📈 Example: Evaluating Data
| Study Finding | How to Think About It |
|---|---|
| High intake of saturated fat is correlated with higher CHD rates | Suggests a possible link, but doesn’t prove cause |
| A country with low CHD also has low smoking rates | Possible protective effect—worth further study |
| Correlation coefficient r = 0.2 | Weak correlation – likely not significant |
| Correlation coefficient r = 0.85 | Strong positive correlation – but still not proof of cause |
Coronary artery occlusion is mainly caused by atherosclerosis and leads to serious heart conditions like angina, heart attacks, or heart failure.
Risk factors include diet, smoking, lack of exercise, and genetics.
Epidemiological data helps identify correlations, but:
– High correlation doesn’t prove causation
– Low or no correlation may refute a hypothesis
– Understanding correlation coefficients helps evaluate the strength of relationships in medical data.
B3.2.7 – Transport of Water from Roots to Leaves During Transpiration
🧪 What is Transpiration?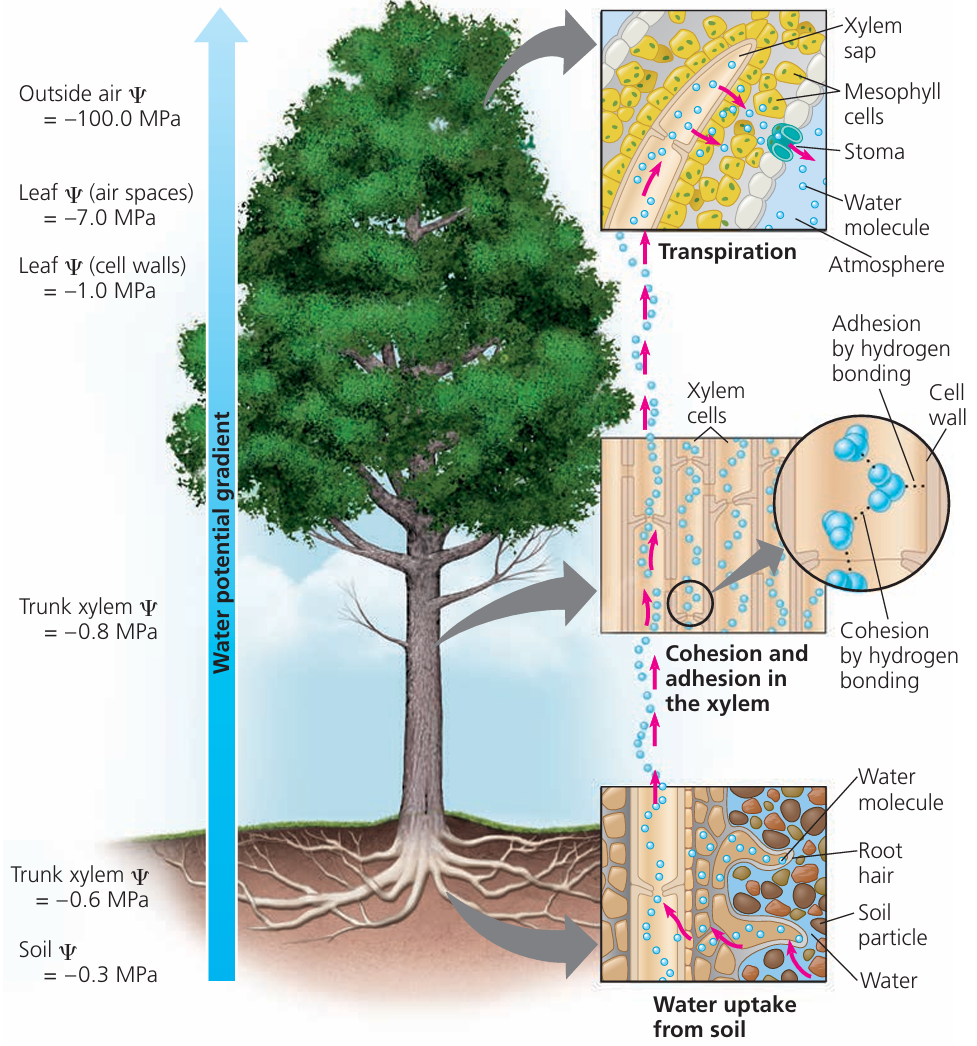
Transpiration is the loss of water vapour from the aerial parts of a plant, mainly through stomata in the leaves. This process helps to pull water upward from the roots to the leaves via xylem vessels.
🔬 How Water Moves Through the Plant (Transpiration Stream)
Water movement is a result of several forces working together:
- Water evaporates from moist cell walls of mesophyll cells into air spaces in the leaf.
- It then diffuses out through the stomata.
- This causes a drop in water potential inside the leaf cells.
- Water is drawn out of xylem vessels in the leaf to replace the lost water.
- This creates tension (a kind of suction or negative pressure) in the xylem.
- The tension pulls water upward from the roots through the stem.
- Due to cohesion, water molecules stick together and form an unbroken column from roots to leaves.
🌱 Key Forces Involved
| Force | What It Does | Why It Matters |
|---|---|---|
| Transpiration pull (tension) | Negative pressure created by water loss in leaves | Pulls water upward through xylem |
| Cohesion | Water molecules stick to each other via hydrogen bonds | Ensures a continuous column of water |
| Adhesion | Water molecules stick to walls of xylem vessels | Helps resist gravity and supports capillary action |
| Capillary action | Combined effect of adhesion + cohesion | Helps draw water through tiny spaces in cell walls |
🌿 Xylem Structure & Function in Water Transport
| Feature | Adaptation | Function |
|---|---|---|
| Hollow, dead cells | No organelles or cytoplasm | Allows free flow of water |
| Lignified walls | Strong and rigid | Prevents collapse under tension |
| Pits | Thin areas without lignin | Allow sideways movement of water between xylem vessels |
| Narrow tubes | Small diameter | Supports capillary action and smooth water flow |
🔍 Why Is Transpiration Important?
- Delivers water to cells for photosynthesis
- Cools the plant through evaporation
- Helps in mineral transport
- Maintains turgor pressure in cells
Water moves from roots to leaves through the xylem by the transpiration stream.
Evaporation from leaves creates tension that pulls water upward.
Cohesion between water molecules keeps the column continuous.
Adhesion and capillary action assist water movement through narrow tubes and cell walls.
Xylem vessels are adapted for this transport: strong, hollow, and narrow.
B3.2.8 – Adaptations of Xylem Vessels for Water Transport
🧬 What Is Xylem?
- Xylem is a type of vascular tissue in plants.
- Its main role is the transport of water and mineral ions from the roots to the leaves.
- Water moves through the xylem as part of the transpiration stream.
🌱 Structural Adaptations of Xylem Vessels
| Adaptation | Feature | Function / Benefit |
|---|---|---|
| No cell contents | Xylem cells are dead at maturity | Provides a clear, open tube for water flow |
| Absent or incomplete end walls | End walls break down to form continuous tubes | Allows uninterrupted vertical flow of water |
| Lignified walls | Thick walls strengthened with lignin | Prevents collapse under tension during transpiration |
| Narrow diameter | Xylem vessels are thin | Helps with capillary action and water cohesion |
| Pits (bordered pits) | Thin areas in walls without lignin | Allow sideways movement of water between vessels or into surrounding cells |
| Tubes arranged vertically | Long vertical columns of connected cells | Supports efficient upward flow of water |
📌 More on Lignin in Xylem Walls
Lignin gives mechanical strength to the vessel walls.
It can form spiral, ring, or reticulate (net-like) patterns, which provide flexibility and strength.
Lignified walls resist the inward pull created by transpiration tension.
🔬 Why Are Xylem Vessels So Effective?
- There’s no obstruction – no cytoplasm, no nuclei – so water moves freely.
- The continuous, hollow structure works like a pipeline.
- The cohesive property of water + transpiration pull = efficient movement.
- Pits are essential when some vessels are blocked or damaged they provide alternative pathways.
📊 Overview Table: Xylem Adaptations
| Structure | Adaptation | How It Helps |
|---|---|---|
| No cytoplasm or organelles | Cells die at maturity | Maximises space for water |
| Lignified thick walls | Strong and waterproof | Prevent collapse & leakage |
| Perforated or missing end walls | Forms continuous tube | Unimpeded water flow |
| Narrow lumen | Small diameter | Enhances capillary action |
| Pits in side walls | Thin non-lignified areas | Lateral water movement |
Xylem vessels are highly specialised tubes designed for efficient water transport.
No internal contents and open structure ensure a smooth, one-way flow.
Lignin makes walls strong and resistant to the tension from transpiration.
Pits allow flexibility in water movement, especially if some paths are blocked.
These features make xylem perfect for moving water up tall plants without energy input.
B3.2.9 – Tissue Distribution in a Dicot Stem (Transverse Section)
🧬 What is a Transverse Section (T.S.)?
A transverse section is a horizontal cross-section of a plant organ (like the stem), cut perpendicular to its length.
Helps us study the arrangement of tissues like xylem, phloem, cortex, and epidermis.
🌱 Key Tissues in a Dicotyledonous Stem
| Tissue | Location | Function |
|---|---|---|
| Epidermis | Outermost layer | Protects stem from physical damage and pathogens; may have a waxy cuticle |
| Cortex | Just inside epidermis | Made of parenchyma cells; stores food and allows diffusion of gases |
| Vascular bundles | Arranged in a circle near edge | Contain xylem and phloem for transport |
| Phloem | Outer part of each vascular bundle | Transports sugars (from leaves to rest of plant) |
| Xylem | Inner part of each vascular bundle | Transports water and minerals (from roots to leaves) |
| Cambium | Between xylem and phloem | Responsible for secondary growth (produces new xylem/phloem) |
| Pith (medulla) | Central region | Stores nutrients and provides structural support |
📌 Arrangement in a Dicot Stem (Top View = Cross Section)
- Vascular bundles are arranged in a ring near the outer edge.
- Each bundle has:
- Xylem on the inner side
- Phloem on the outer side
- Cambium in between (in growing stems)
- The cortex surrounds the ring.
- The epidermis is the outermost layer.
- The pith is in the center.
✍️ Example Annotations for Diagram
| Label | Annotation (Function) |
|---|---|
| Epidermis | Protection; may secrete cuticle |
| Cortex | Storage; gas exchange |
| Phloem | Transports sugars (translocation) |
| Xylem | Transports water and minerals |
| Cambium | Produces new vascular tissue |
| Pith | Stores nutrients; supports stem |
In dicot stems, vascular bundles are arranged in a ring.
Xylem is on the inside, phloem on the outside, and cambium in between.
Cortex and pith provide support and storage.
B3.2.10 – Tissue Distribution in a Dicot Root (Transverse Section)
🧬 What is a Transverse Section of a Root?
A transverse section (T.S.) is a cross-sectional cut made perpendicular to the root’s length.
It shows the internal arrangement of tissues like xylem, phloem, cortex, and epidermis in a dicotyledonous plant root.
🌿 Key Tissues in a Dicot Root
| Tissue | Location | Function |
|---|---|---|
| Epidermis | Outermost layer (often with root hairs) | Absorbs water and minerals from soil |
| Cortex | Inside epidermis, large region | Stores food, aids in water movement |
| Endodermis | Thin single layer around vascular bundle | Regulates entry of water and minerals into xylem |
| Pericycle | Just inside endodermis | Can form lateral roots and vascular tissues |
| Xylem | Centrally located, star-shaped | Transports water and minerals upwards |
| Phloem | Between arms of xylem star | Transports sugars and organic substances |
📌 Typical Arrangement in a Dicot Root (T.S. View)
- Xylem forms a central “X” or star shape.
- Phloem is found between the arms of the xylem.
- The vascular bundle is compact and centrally located.
- Cortex is thick and surrounds the vascular tissue.
- Epidermis is the outermost layer.
📊 Table of Root Tissue Functions
| Tissue | Function |
|---|---|
| Epidermis | Absorbs water and minerals from soil |
| Cortex | Stores starch, helps in water movement |
| Endodermis | Regulates selective absorption into xylem |
| Pericycle | Origin of lateral roots and new vascular tissue |
| Xylem | Conducts water and minerals upward |
| Phloem | Transports food from leaves to roots |
In dicot roots, xylem is central and star-shaped, surrounded by phloem.
The vascular bundle is compact and located centrally, unlike in stems.
Cortex and epidermis assist in absorption and storage.
Additional Higher Level
B3.2.11 – Release and Reuptake of Tissue Fluid in Capillaries
🧬 What is Tissue Fluid?
- Tissue fluid is the watery fluid that surrounds body cells.
- It delivers oxygen and nutrients to cells and removes waste products.
- It is formed from blood plasma (without large proteins or blood cells) and acts as the link between blood and cells.
🌱 How Is Tissue Fluid Formed? (Pressure Filtration)
Process at the Arterial End of Capillaries:
| Step | What Happens | Why It Happens |
|---|---|---|
| 1 | Blood enters capillaries from arterioles under high hydrostatic pressure | Due to strong pumping action of the heart |
| 2 | This pressure forces plasma out of the capillaries through gaps in the wall | Called pressure filtration |
| 3 | Large proteins and blood cells stay in the blood | They’re too big to pass through |
| 4 | The filtered fluid is now called tissue fluid | It bathes the cells, allowing exchange of substances |
🔁 How Is Tissue Fluid Reabsorbed?
Process at the Venous End of Capillaries:
| Force | Effect |
|---|---|
| Hydrostatic pressure drops | Blood pressure decreases due to fluid loss |
| Oncotic pressure remains | Plasma proteins (mainly albumin) create a pulling force that draws water back in |
| Net inward flow | Tissue fluid returns to capillaries by osmosis |
Not all fluid is reabsorbed – some enters lymph vessels and eventually returns to the blood.
📊 Overview Table: Pressure Changes in Capillaries
| Capillary End | Hydrostatic Pressure | Oncotic Pressure | Net Movement |
|---|---|---|---|
| Arterial end | High | Low | Fluid pushed out (filtration) |
| Venous end | Low | High | Fluid drawn in (reabsorption) |
🩸 Summary of Forces Involved
| Force | Direction | Explanation |
|---|---|---|
| Hydrostatic pressure | Outward | Pushes plasma out of capillaries |
| Oncotic (osmotic) pressure | Inward | Pulls water back due to plasma proteins |
🔍 Why Is Tissue Fluid Important?
- Allows diffusion of oxygen, glucose, amino acids into cells.
- Collects waste products like CO₂ and urea.
- Maintains a moist environment for cell functioning.
- Assists in temperature regulation and immune cell movement.
Tissue fluid is formed at the arterial end of capillaries by pressure filtration of blood plasma.
High hydrostatic pressure pushes fluid out; large proteins stay behind.
At the venous end, lower pressure + oncotic pull causes most of the fluid to return to the blood.
Excess fluid is collected by the lymphatic system.
Tissue fluid is vital for cellular exchange and maintaining homeostasis.
B3.2.12 – Exchange Between Tissue Fluid and Cells
🧬 What Is Tissue Fluid?
Tissue fluid is the watery fluid surrounding cells in tissues. It is formed by pressure filtration of blood plasma from capillaries and acts as a medium for exchange of substances between blood and cells.
🌱 Exchange Between Tissue Fluid and Cells
| Substance | Direction | Why It Happens |
|---|---|---|
| Oxygen (O₂) | From tissue fluid → into cells | For cellular respiration |
| Glucose, amino acids, fatty acids | From tissue fluid → into cells | Used for energy and growth |
| Carbon dioxide (CO₂) | From cells → into tissue fluid | Waste from respiration |
| Urea and other wastes | From cells → into tissue fluid | To be excreted by kidneys |
| Hormones | From tissue fluid → into cells | To trigger specific cell responses |
This exchange happens mostly by diffusion, depending on concentration gradients.
🔬 Plasma vs Tissue Fluid – Composition Comparison
| Component | Plasma | Tissue Fluid |
|---|---|---|
| Water | ✅ | ✅ |
| Oxygen (O₂) | ✅ | ✅ |
| Glucose | ✅ | ✅ |
| Amino acids / fatty acids | ✅ | ✅ |
| Ions (Na⁺, K⁺, Cl⁻, etc.) | ✅ | ✅ |
| Hormones | ✅ | ✅ |
| Plasma proteins (e.g. albumin) | ✅ | ❌ |
| Red blood cells | ✅ | ❌ |
| White blood cells | ✅ | Some may enter during infection |
| Platelets | ✅ | ❌ |
📌 Key Differences Between Plasma & Tissue Fluid
| Plasma | Tissue Fluid |
|---|---|
| Found inside blood vessels | Found outside blood vessels, around cells |
| Contains plasma proteins | Lacks large proteins |
| Carries blood cells | Normally no blood cells, except WBCs |
| Slightly higher pressure | Lower pressure |
| Part of circulatory system | Part of interstitial fluid in tissues |
Tissue fluid allows two-way exchange between cells and capillaries.
Cells receive oxygen, glucose, amino acids, and hormones.
Cells release CO₂ and waste into tissue fluid.
Plasma and tissue fluid have similar compositions, but:
– Tissue fluid lacks large proteins and cells
– Plasma is confined to vessels, tissue fluid surrounds cells
This system keeps cells nourished and in balance with their environment.
B3.2.13 – Drainage of Excess Tissue Fluid into Lymph Ducts
🌿 What Happens to Extra Tissue Fluid?
Not all tissue fluid returns to capillaries at the venous end.
Excess tissue fluid is collected by a separate system: the lymphatic system.
🧬 What Is the Lymphatic System?
A network of vessels, ducts, and nodes that helps:
- Drain excess tissue fluid
- Transport white blood cells
- Support the immune system
🔄 How Excess Fluid Drains into Lymph Ducts
✅ Step-by-Step Flow:
- Tissue fluid builds up in spaces between cells.
- It enters lymph capillaries via tiny gaps in their thin walls.
- Fluid inside is now called lymph.
- Lymph travels through lymph vessels, which:
- Have thin walls with gaps (allowing fluid entry).
- Contain valves to prevent backflow.
- Lymph is eventually returned to the bloodstream, usually at:
- The subclavian vein (near the neck/shoulders).
📌 Key Features of Lymphatic Vessels
| Feature | Function |
|---|---|
| Thin walls | Allow easy entry of tissue fluid |
| Gaps in wall | Permit movement of fluid, proteins, and WBCs |
| Valves | Ensure one-way flow towards the heart |
| No pump | Movement depends on skeletal muscle contractions |
📊 Table: Blood Capillaries vs Lymph Vessels
| Feature | Blood Capillaries | Lymphatic Vessels |
|---|---|---|
| Wall structure | One cell thick | Thin with larger gaps |
| Pressure | High → low | Low |
| Contains | Blood plasma (or cells) | Lymph (filtered tissue fluid) |
| Direction of flow | Two-way exchange | One-way (towards heart) |
| Valves | Absent | Present |
🔬 What’s in Lymph?
- Water
- Ions
- Small proteins
- Fats (from intestine)
- White blood cells (mainly lymphocytes)
- Waste products
Excess tissue fluid is drained by the lymphatic system.
Lymph vessels have thin walls, valves, and gaps to collect and direct fluid.
Lymph is eventually returned to the blood, maintaining fluid balance.
This process supports circulation and immunity.
B3.2.14 – Single vs Double Circulation
🧬 What Is Circulation?
Circulation refers to the path blood takes through the heart and around the body.
Animals may have either:
- Single circulation (e.g. bony fish)
- Double circulation (e.g. mammals)
Single Circulation in Bony Fish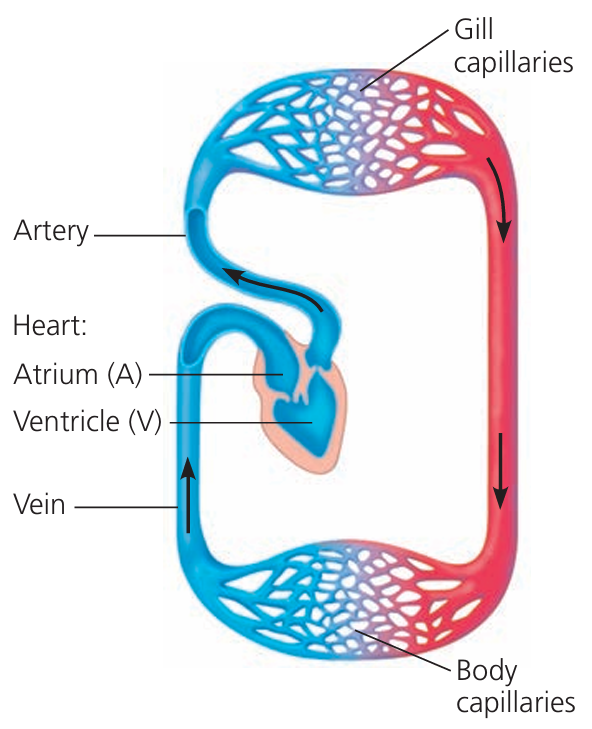
Blood flows through the heart once per complete body circuit.
Simple Flow:
Heart → Gills → Body → Heart
💡 Key Points:
- 2-chambered heart (1 atrium, 1 ventricle)
- Blood is oxygenated at the gills.
- After the gills, blood goes to the rest of the body.
- Slower flow due to drop in pressure after gills.
Double Circulation in Mammals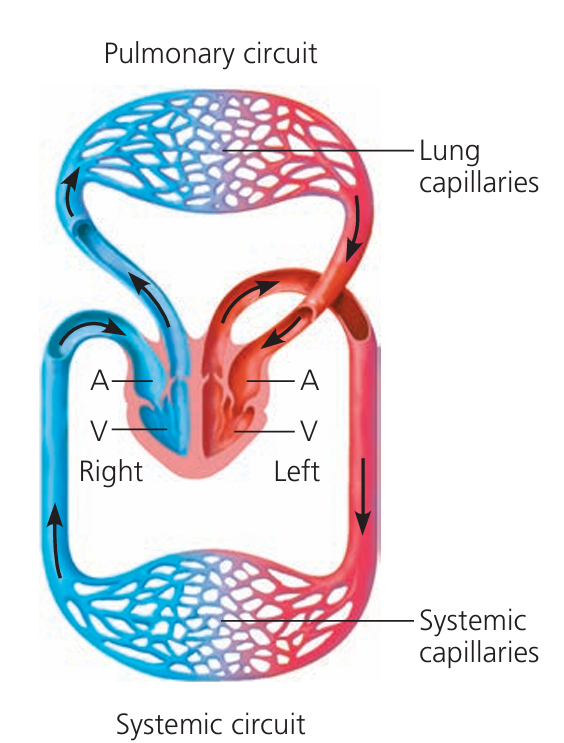
Blood flows through the heart twice per complete circuit.
Two Circuits:
- Pulmonary circulation: Heart → Lungs → Heart (for oxygenation)
- Systemic circulation: Heart → Body → Heart (to deliver oxygen to tissues)
💡 Key Points:
- 4-chambered heart (2 atria, 2 ventricles)
- Maintains high pressure in systemic circuit.
- Faster and more efficient oxygen delivery.
📊 Comparison Table: Single vs Double Circulation
| Feature | Single Circulation (Fish) | Double Circulation (Mammals) |
|---|---|---|
| Heart chambers | 2 (1 atrium, 1 ventricle) | 4 (2 atria, 2 ventricles) |
| Blood passes through heart | Once per circuit | Twice per circuit |
| Oxygenation site | Gills | Lungs |
| Efficiency | Lower | Higher |
| Blood pressure to body | Drops after gills | Maintained high from left ventricle |
| Adaptation for | Aquatic life | High-energy demands of warm-blooded life |
Fish have single circulation: Heart → Gills → Body → Heart.
Mammals have double circulation:
Pulmonary (Heart → Lungs → Heart) + Systemic (Heart → Body → Heart)
Double circulation provides higher pressure and speed, ideal for active, warm-blooded organisms.
B3.2.15 – Adaptations of the Mammalian Heart for Pressurized Blood Flow
🧬 Main Function of the Heart
Acts as a muscular pump to keep blood flowing under pressure through arteries to organs.
Must generate high pressure to ensure efficient oxygen and nutrient delivery.
🔍 Structural Adaptations & Their Functions
| Structure | Form–Function Adaptation |
|---|---|
| Cardiac Muscle | Specialized myogenic (self-contracting) muscle; strong, thick walls in ventricles (esp. left) allow forceful contraction to pump blood under high pressure. Doesn’t fatigue easily. |
| Pacemaker (Sinoatrial Node – SA Node) | Located in the right atrium wall. Initiates electrical impulses that cause rhythmic contractions—controls heartbeat rate and ensures coordinated pumping. |
| Atria | Thin-walled upper chambers that receive blood from veins. Push blood into ventricles at low pressure. |
| Ventricles | Thicker muscular walls than atria. Especially left ventricle—its thick wall pumps blood into the aorta under high pressure for systemic circulation. |
| Atrioventricular (AV) Valves | Between atria and ventricles (tricuspid & bicuspid). Prevent backflow into atria when ventricles contract. |
| Semilunar Valves | At exits of ventricles (aortic and pulmonary valves). Prevent backflow from arteries into ventricles. |
| Septum | Muscular wall that separates left and right sides of the heart. Prevents mixing of oxygenated and deoxygenated blood. |
| Coronary Vessels | Supply oxygen and glucose to the heart muscle itself. Essential for maintaining continuous contraction. Blockage here → heart attack. |
🔁 Unidirectional Flow of Blood Through the Heart
🩸 Path of Blood (Frontal Plane View):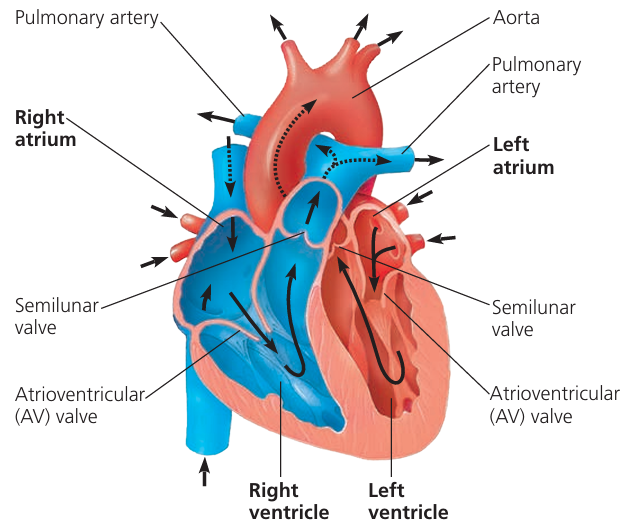
Vena cava (deoxygenated blood from body) →
Right atrium →
Tricuspid valve →
Right ventricle →
Pulmonary valve →
Pulmonary artery → lungs (oxygenation) →
Pulmonary vein (oxygenated blood) →
Left atrium →
Bicuspid valve →
Left ventricle →
Aortic valve →
Aorta → rest of the body
👉 Valves ensure one-way flow and prevent backflow at each stage.
The mammalian heart is highly specialized to maintain high-pressure, unidirectional flow.
Thick ventricles, especially on the left side, help push blood over long distances.
Valves, pacemaker cells, and coronary circulation all work together to keep blood moving efficiently and reliably.
B3.2.16 – Stages in the Cardiac Cycle
🧬 What Is the Cardiac Cycle?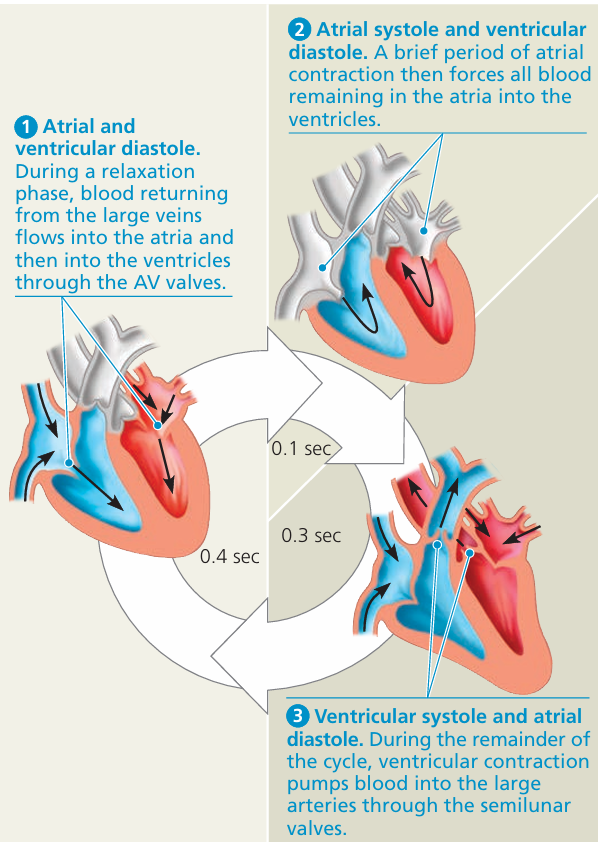
- The cardiac cycle refers to the sequence of events during one complete heartbeat (usually ~0.8 sec).
- It includes contraction (systole) and relaxation (diastole) of atria and ventricles.
- Controlled by the sinoatrial node (SA node) the heart’s natural pacemaker.
🔁 Sequence of Events in the Cardiac Cycle (Left Side)
| Stage | Event | Description |
|---|---|---|
| 1. Atrial systole | Atria contract | – SA node fires, sending electrical impulse Left atrium contracts → blood pushed into left ventricle through bicuspid valve |
| 2. Ventricular systole | Ventricle contracts | – Impulse reaches AV node, travels via Bundle of His → Purkinje fibers Left ventricle contracts → blood pushed into aorta through aortic valve Bicuspid valve closes to prevent backflow |
| 3. Diastole (whole heart) | Relaxation phase | – Both atrium and ventricle relax Aortic valve closes to prevent backflow Blood starts to fill the atrium again from pulmonary vein Cycle repeats |
This unidirectional flow is maintained by valves and coordinated muscle contractions.
📈 Systolic vs Diastolic Blood Pressure
| Term | Definition | Typical Value |
|---|---|---|
| Systolic Pressure | Pressure in arteries during ventricular contraction | ~120 mmHg |
| Diastolic Pressure | Pressure in arteries during relaxation | ~80 mmHg |
Measured as: Systolic / Diastolic (e.g. 120/80 mmHg)
🩺 Interpreting Blood Pressure Readings:
- High systolic = may indicate strain on arteries.
- Low diastolic = poor blood flow or dehydration.
- Pulse pressure = Systolic – Diastolic (should be ~40 mmHg).
📊 Graph of Pressure Changes During Cardiac Cycle
| Region | What happens |
|---|---|
| Atrial pressure | Slight rise during atrial systole |
| Ventricular pressure | Rises sharply during systole, drops in diastole |
| Aortic pressure | Follows ventricular pressure but stays relatively high due to elastic recoil |
The SA node starts the heartbeat → triggers atrial then ventricular systole.
Valves ensure blood moves in one direction.
Systole = contraction, Diastole = relaxation.
Blood pressure measures force in arteries:
→ Systolic (high point) during ventricular contraction
→ Diastolic (low point) during relaxation
B3.2.17 – Generation of Root Pressure in Xylem Vessels
🧪 What Is Root Pressure?
Root pressure is a positive pressure that helps push water upward through xylem vessels.
It plays a supporting role when transpiration is low or absent, e.g.:
- High humidity
- Springtime in deciduous plants (before leaves open)

🧬 How Root Pressure Is Generated
🌱 Step-by-Step Process:
- Active transport of mineral ions (like nitrates, K⁺, etc.) from root cells into xylem.
- Requires energy (ATP).
- Increases solute concentration in xylem.
- This creates a water potential gradient:
- Water moves into the xylem by osmosis from surrounding root cells.
- The incoming water creates a positive hydrostatic pressure.
- This is root pressure.
- Root pressure helps push water up the stem, even without transpiration pull.
🔍 Example Situations:
| Condition | Why Root Pressure Is Important |
|---|---|
| High humidity | Transpiration is very low → root pressure drives water upward |
| Spring (no leaves) | No transpiration yet → root pressure helps rehydrate plant tissues |
📌 Quick Comparison: Root Pressure vs Transpiration Pull
| Feature | Root Pressure | Transpiration Pull |
|---|---|---|
| Driven by | Active transport of ions | Water loss from leaves |
| Pressure type | Positive | Negative (tension) |
| When important | Low transpiration (humid, spring) | Normal or high transpiration |
| Energy required? | Yes (active transport) | No (passive) |
🧠 Summary Box:
Root pressure is a positive pressure in xylem caused by active ion transport and osmosis.
It helps maintain water movement when transpiration is low.
Essential in early spring or humid conditions.
Works alongside transpiration pull to maintain upward water transport.
B3.2.18 – Adaptations of Phloem Sieve Tubes and Companion Cells
🧪 What Is Translocation?
Translocation is the active transport of sap (mainly sugars like sucrose) through phloem from:
Source = where sugars are made (e.g. leaves) → Sink = where sugars are used/stored (e.g. roots, fruits, growing shoots)
Sap = mix of sugars, amino acids, hormones, ions, etc.
🌿 Phloem Structure Overview
Phloem is made of:
- Sieve tube elements
- Companion cells
- Parenchyma & fibers (support)
📌 Adaptations of Sieve Tube Elements
| Adaptation | Function |
|---|---|
| Sieve plates (perforated end walls) | Allow easy flow of sap between cells |
| Reduced cytoplasm | More space for sap flow |
| No nucleus or ribosomes | No obstruction to flow |
| Long tube-like cells | Form a continuous transport system |
⚠️ Sieve tube elements are living but cannot survive alone due to lack of nucleus – they rely on companion cells.
🔋 Adaptations of Companion Cells
| Adaptation | Function |
|---|---|
| Many mitochondria | Provide ATP for active loading/unloading of sucrose |
| Nucleus & full organelles | Control metabolism of both themselves & sieve tubes |
| Plasmodesmata (cytoplasmic connections) | Allow exchange of substances between companion cells and sieve tubes |
🔄 How Adaptations Help in Translocation
| Process | Explanation |
|---|---|
| Loading (at source) | Companion cells use ATP to pump sucrose into sieve tubes → decreases water potential → water enters by osmosis → generates pressure |
| Flow through sieve tubes | Adaptations (no nucleus, sieve plates) reduce resistance → sap flows by pressure |
| Unloading (at sink) | Sugars actively or passively removed → water follows by osmosis → pressure drops → keeps flow going |
🧠 Key Takeaways:
Sieve tube elements are adapted for flow:
No nucleus, thin cytoplasm, sieve plates
Companion cells support them:
Mitochondria for energy, plasmodesmata for transfer
These adaptations ensure efficient pressure-driven flow of sugar-rich sap.
Translocation moves materials from sources to sinks based on plant needs.

