IB DP Biology D3.3 Homeostasis Study Notes - New Syllabus -2025
IB DP Biology D3.3 Homeostasis Study Notes – New syllbaus
IB DP Biology D3.3 Homeostasis Study Notes at IITian Academy focus on specific topic and type of questions asked in actual exam. Study Notes focus on IB Biology syllabus with guiding questions of
- How are constant internal conditions maintained in humans?
- What are the benefits to organisms of maintaining constant internal conditions?
Standard level and higher level: 2 hours
Additional higher level: 2 hours
D3.3.1 – Homeostasis: Maintenance of the Internal Environment
🧬 What is Homeostasis?
- Homeostasis is the process by which an organism keeps its internal environment stable.
- It involves keeping key variables within narrow, preset limits, even when the external environment changes.
- This stability is vital for cells and organs to function properly.
📌 Key Homeostatic Variables in Humans
| Variable | Normal Range / Set Point | Importance |
|---|---|---|
| Body temperature | Around 37°C | Enzymes work best at this temperature; too high or low damages cells |
| Blood pH | Around 7.4 (slightly alkaline) | pH affects enzyme activity and oxygen transport |
| Blood glucose concentration | ~4-6 mmol/L (fasting) | Provides steady energy supply; too high or low is harmful |
| Blood osmotic concentration | ~300 mOsm/L | Maintains fluid balance and cell size |
🌿 How Does Homeostasis Work?
Body uses feedback systems to monitor and adjust these variables.
Typically involves three parts:
- Receptor: Detects change (e.g., temperature sensors in skin).
- Coordinator (Control center): Usually brain or endocrine glands; processes info.
- Effector: Produces response to restore balance (e.g., sweat glands, muscles).
🔍 Examples of Homeostasis in Action
| Variable | Change | Response | Effect |
|---|---|---|---|
| Body temperature | Rises (hot environment) | Sweat production, vasodilation of skin blood vessels | Heat loss, temperature returns to normal |
| Blood glucose | Increases after meal | Insulin released by pancreas | Cells take up glucose, blood level lowers |
| Blood pH | Drops (acidosis) | Increased breathing rate to expel CO₂ | Raises blood pH back to normal |
| Blood osmotic concentration | Increases (dehydration) | Thirst stimulated, ADH hormone released | Water intake and retention restore balance |
🧠 Why Is Homeostasis Important?
- Ensures enzymes and cells function optimally.
- Protects against harmful extremes (too hot/cold, acidic/basic).
- Maintains fluid and electrolyte balance.
- Supports overall health and survival.
D3.3.2 – Negative Feedback Loops in Homeostasis
🧬 What is Negative Feedback?
- Negative feedback is a control mechanism that reverses any change in a homeostatic variable to bring it back to its normal level (set point).
- It acts like a thermostat in your home: if the temperature goes too high or too low, it triggers actions to restore balance.
- Negative feedback maintains stability by correcting deviations both above and below the set point.
🌿 Why Negative Feedback?
- It prevents extreme fluctuations in the body.
- Keeps variables within narrow, safe limits.
- Ensures a stable internal environment, which is essential for cell function.
- Positive feedback, in contrast, amplifies changes, which is usually unstable and rare in homeostasis (except in special cases like blood clotting or childbirth).
🔍 How Negative Feedback Works: Basic Steps
| Step | Description | Example |
|---|---|---|
| 1. Stimulus | Change occurs, e.g., body temperature rises | Heat from environment |
| 2. Receptor | Detects change, e.g., temperature sensors in skin | Thermoreceptors |
| 3. Control center | Processes info, e.g., hypothalamus in brain | Receives signal |
| 4. Effector | Produces response to reverse change | Sweat glands activate to cool skin |
| 5. Response | Variable returns toward set point | Body temperature lowers to normal |
📌 Example: Blood Glucose Regulation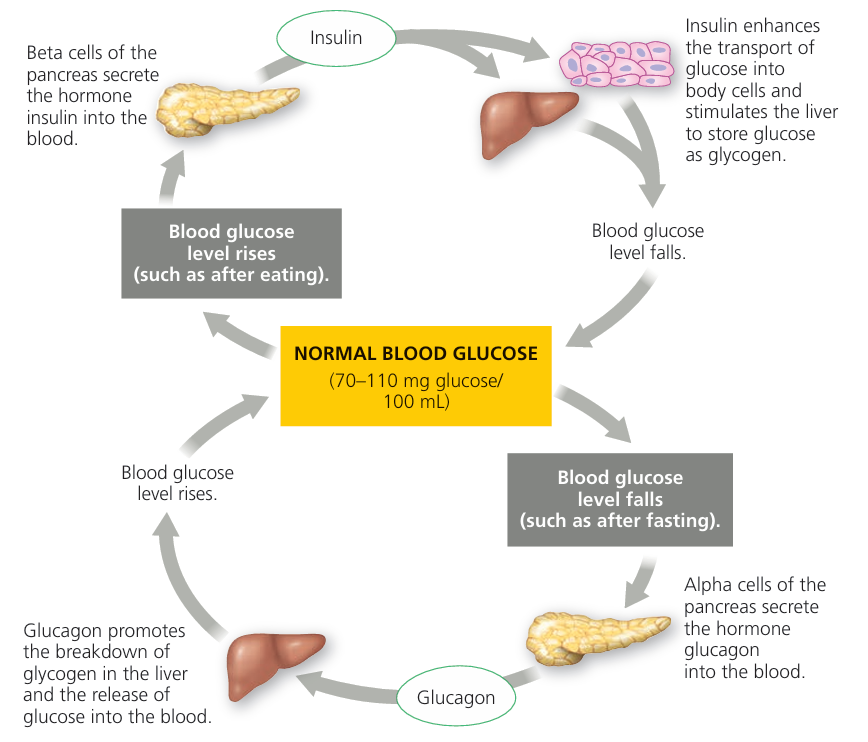
If blood glucose rises after eating:
Pancreas releases insulin.
Insulin promotes glucose uptake by cells.
Blood glucose falls back to normal.
If blood glucose drops:
Pancreas releases glucagon.
Glucagon triggers glucose release from liver.
Blood glucose rises to normal.
📊 Negative Feedback vs Positive Feedback
| Feature | Negative Feedback | Positive Feedback |
|---|---|---|
| Effect on change | Reverses change | Amplifies change |
| Role in homeostasis | Maintains stability | Rare, triggers rapid events |
| Examples | Temperature, blood glucose | Blood clotting, childbirth contractions |
| Outcome | Returns variable to set point | Drives process to completion |
D3.3.3 – Regulation of Blood Glucose: Hormonal Control in Homeostasis
🧬 Why Regulate Blood Glucose?
- Glucose is the main energy source for cells.
- Blood glucose levels must stay within a narrow range (~4–6 mmol/L).
- Too high or low glucose levels can disrupt cell function and be harmful.
🌿 Key Hormones Involved
| Hormone | Source | Role in Blood Glucose Regulation |
|---|---|---|
| Insulin | Beta cells of the pancreas | Lowers blood glucose |
| Glucagon | Alpha cells of the pancreas | Raises blood glucose |
🔬 How Insulin Works
Released when blood glucose is high (e.g., after eating).
Transported in blood to target cells (muscle, liver, fat).
Effects on target cells:
- Increases glucose uptake (muscle and fat cells).
- Stimulates conversion of glucose to glycogen (glycogenesis) in the liver.
- Promotes fat storage.
Result: Blood glucose levels decrease back to normal.
🧪 How Glucagon Works
Released when blood glucose is low (e.g., between meals or fasting).
Travels via blood to the liver (main target).
Effects:
- Stimulates breakdown of glycogen to glucose (glycogenolysis).
- Promotes formation of glucose from non-carbohydrate sources (gluconeogenesis).
Result: Blood glucose levels increase back to normal.
📍 Control of Hormone Secretion
Pancreatic endocrine cells detect blood glucose changes directly.
High glucose → stimulates beta cells to release insulin.
Low glucose → stimulates alpha cells to release glucagon.
Both hormones work antagonistically to maintain glucose balance.
🔍 Feedback Loop Summary
| Change in Blood Glucose | Hormonal Response | Effect on Blood Glucose |
|---|---|---|
| Blood glucose rises | Insulin secreted | Lowers glucose by uptake & storage |
| Blood glucose falls | Glucagon secreted | Raises glucose by glycogen breakdown & synthesis |
🧠 Why Is This Important?
Maintains a constant energy supply to cells, especially the brain.
Prevents damage caused by hyperglycemia (high glucose) and hypoglycemia (low glucose).
Illustrates hormonal control as a key homeostatic mechanism.
Blood glucose is tightly regulated by insulin and glucagon, secreted by pancreatic endocrine cells.
Insulin lowers glucose by increasing uptake and storage.
Glucagon raises glucose by breaking down glycogen and making new glucose.
This negative feedback system keeps blood glucose within a healthy range.
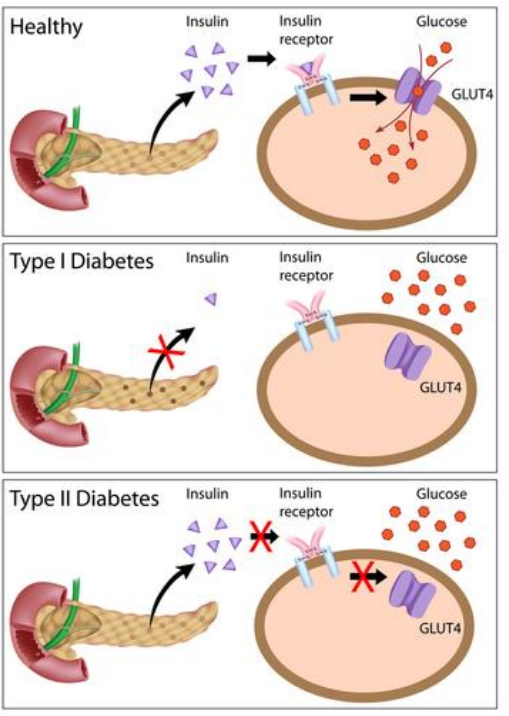
D3.3.4 – Physiological Changes in Type 1 and Type 2 Diabetes
🧠 What is Diabetes?
- Diabetes is a chronic condition where the body cannot regulate blood glucose properly.
- Results in high blood glucose (hyperglycemia).
- Two main types: Type 1 and Type 2 diabetes.
🌿 Type 1 Diabetes
| Aspect | Details |
|---|---|
| Cause | Autoimmune destruction of beta cells in the pancreas |
| Effect | Little or no insulin production |
| Result | Blood glucose remains high because glucose can’t enter cells |
| Risk Factors | Genetic predisposition, autoimmune triggers (unknown exact cause) |
| Common Age of Onset | Usually childhood or adolescence |
| Treatment | Requires insulin injections to regulate blood glucose |
| Prevention | Currently no known prevention |
🌿 Type 2 Diabetes
| Aspect | Details |
|---|---|
| Cause | Insulin resistance: body cells respond poorly to insulin Eventually, pancreas may produce less insulin |
| Effect | High blood glucose due to ineffective glucose uptake |
| Risk Factors | Obesity, sedentary lifestyle, poor diet, age, genetics |
| Common Age of Onset | Usually adults, but increasing in younger people due to lifestyle |
| Treatment | Lifestyle changes (diet, exercise), oral medications, sometimes insulin |
| Prevention | Healthy diet, regular physical activity, weight management |
🔬 Physiological Changes in Both Types
| Change | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Insulin levels | Low or absent | Normal, high initially, then may decrease |
| Blood glucose | High | High |
| Glucose uptake by cells | Severely reduced | Reduced due to resistance |
| Effects on metabolism | Cells starve for glucose, use fats → weight loss, ketoacidosis risk | Cells starve for glucose but less severe initially |
🔍 Why Diabetes is Dangerous
- High blood glucose damages blood vessels and nerves.
- Leads to complications: heart disease, kidney failure, blindness, poor wound healing.
- Managing blood glucose is crucial to prevent these.
📌 Summary Table: Differences Between Type 1 & Type 2 Diabetes
| Feature | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune beta cell destruction | Insulin resistance + eventual insulin deficiency |
| Insulin Production | None or very low | Initially normal/high, then decreases |
| Onset Age | Usually young | Usually adult (but younger cases rising) |
| Risk Factors | Genetics, autoimmunity | Obesity, lifestyle, genetics |
| Treatment | Insulin injections | Lifestyle changes, meds, insulin if needed |
| Prevention | No known prevention | Healthy lifestyle can prevent/delay |
Type 1 diabetes is caused by loss of insulin production due to immune attack.
Type 2 diabetes is caused mainly by cells becoming resistant to insulin.
Both cause high blood glucose but differ in causes, risk factors, and treatment.
Prevention focuses on lifestyle changes for type 2; type 1 currently has no prevention.
Managing blood glucose is vital to avoid serious health complications.
D3.3.5 – Thermoregulation as an Example of Negative Feedback Control
🧬 What is Thermoregulation?
Thermoregulation is the process by which the body maintains a stable internal temperature (~37°C), despite changes in the external environment.
It is a classic example of negative feedback control.
🌿 Key Components of Thermoregulation
| Component | Role |
|---|---|
| Peripheral thermoreceptors | Detect temperature changes in the skin and send signals to the brain |
| Hypothalamus | Acts as the control center; compares signals with the set point and coordinates responses |
| Pituitary gland | Releases hormones like thyroid-stimulating hormone (TSH) to regulate metabolism |
| Thyroxin | Hormone from the thyroid gland that increases metabolic rate, producing heat |
🔬 How the Body Responds to Temperature Changes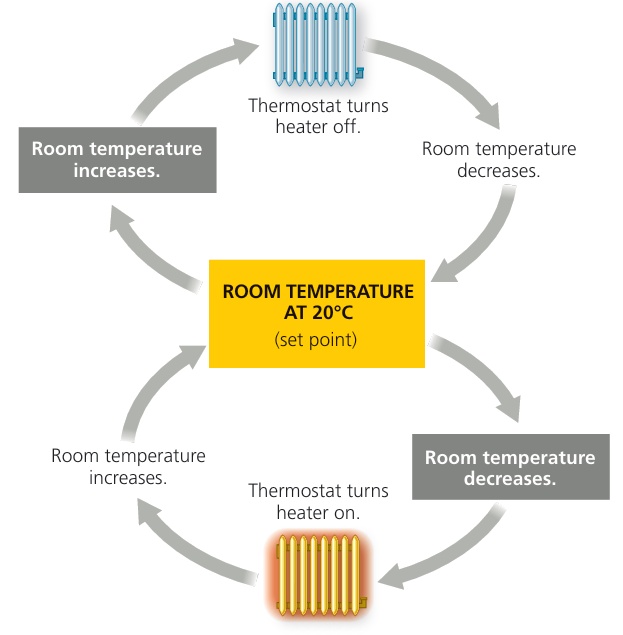
When Body Temperature Rises (Too Hot):
- Peripheral thermoreceptors detect increased skin temperature.
- Signals sent to hypothalamus trigger cooling mechanisms:
- Sweat glands produce sweat → evaporative cooling.
- Vasodilation of skin blood vessels → more heat lost through skin.
- Metabolic rate may decrease to reduce heat production.
When Body Temperature Falls (Too Cold):
- Peripheral thermoreceptors detect low temperature.
- Hypothalamus activates heat-producing responses:
- Muscle shivering: rapid muscle contractions generate heat.
- Vasoconstriction: skin blood vessels constrict to reduce heat loss.
- Thyroxin secretion increases, raising metabolic rate for more heat.
- Brown adipose tissue (brown fat) generates heat by burning fats (non-shivering thermogenesis).
📍 Role of Effectors: Muscle and Adipose Tissue
| Effector | Function |
|---|---|
| Skeletal muscles | Shivering produces heat by rapid contractions |
| Brown adipose tissue | Specialized fat that generates heat without muscle movement (especially in infants) |
🔍 Summary of Negative Feedback Loop in Thermoregulation
| Step | Description |
|---|---|
| 1. Stimulus | Body temperature deviates from set point |
| 2. Receptors | Peripheral thermoreceptors detect change |
| 3. Control center | Hypothalamus processes info and coordinates response |
| 4. Effectors | Sweat glands, muscles, blood vessels, thyroid gland respond |
| 5. Response | Body temperature returns to normal |
🧠 Why Is Thermoregulation Important?
Keeps enzymes working optimally.
Prevents damage from extreme temperatures.
Maintains overall homeostasis and survival.
Thermoregulation is controlled by a negative feedback system involving sensors (thermoreceptors), control center (hypothalamus), and effectors.
Sweating, vasodilation, shivering, vasoconstriction, and hormone regulation work together to maintain temperature.
Thyroxin increases metabolic heat production.
Muscle activity and brown fat play important roles in generating heat when cold.
D3.3.6 – Thermoregulation Mechanisms in Humans
🧬 How Humans Regulate Body Temperature
Humans maintain a stable internal temperature (~37°C) through a mix of physiological and behavioural responses.
These responses help balance heat gain and heat loss to adapt to changing environments.
🌿 Physiological Mechanisms of Thermoregulation
| Mechanism | Description | Effect on Body Temperature |
|---|---|---|
| Vasodilation | Blood vessels near the skin widen (dilate) | Increases blood flow to skin → more heat lost by radiation and convection → cools body |
| Vasoconstriction | Blood vessels near the skin narrow (constrict) | Reduces blood flow to skin → less heat lost → conserves heat |
| Shivering | Rapid involuntary muscle contractions | Generates heat through increased metabolic activity |
| Sweating | Sweat glands release sweat onto skin | Evaporation of sweat removes heat, cooling the body |
| Hair erection (piloerection) | Tiny muscles at hair follicles contract, making hairs stand up | Traps a layer of air for insulation → reduces heat loss |
| Uncoupled respiration in brown adipose tissue (BAT) | BAT cells use fat to generate heat instead of ATP | Produces heat without muscle movement (non-shivering thermogenesis) |
🔬 How These Mechanisms Work Together
| Condition | Response | Purpose |
|---|---|---|
| Too hot | Vasodilation, sweating, hair lies flat | Lose excess heat |
| Too cold | Vasoconstriction, shivering, hair stands up, BAT activation | Generate and conserve heat |
📍 Additional Behavioural Adaptations (Brief Mention)
Seeking shade or shelter
Wearing or removing clothing
Changing activity levels (e.g., resting when hot)
🧠 Why These Mechanisms Are Important
Keep internal conditions stable for enzyme function.
Protect against heat stress or hypothermia.
Ensure overall homeostasis and survival.
Humans use vasodilation, vasoconstriction, sweating, shivering, hair erection, and brown fat activity to control temperature.
These are mainly physiological responses regulated by the nervous and endocrine systems.
Behavioural changes also help but are outside the scope of detailed study.
Together, these keep body temperature within narrow, safe limits.
D3.3.7 – Role of the Kidney in Osmoregulation and Excretion
🧠 Key Definitions
Excretion: The process of removing metabolic waste products from the body (e.g., urea, carbon dioxide).
Osmoregulation: The process of maintaining the balance of water and dissolved solutes (osmotic concentration) in body fluids.
🌿 Osmotic Concentration
Osmotic concentration is measured in osmoles per litre (osmol L⁻¹).
It refers to the total concentration of dissolved particles (solutes) in a solution.
Cells and tissues must keep osmotic concentration within limits to maintain proper hydration and cell function.
🔬 Kidney Functions
| Function | Description | Importance |
|---|---|---|
| Excretion | Removes nitrogenous wastes like urea from the blood by filtering and producing urine | Prevents toxic build-up |
| Osmoregulation | Controls the water and salt balance by adjusting the volume and concentration of urine | Maintains blood osmotic concentration within narrow limits |
📍 How Kidneys Perform Osmoregulation
- Blood enters the kidney and is filtered through the glomerulus.
- Useful substances (glucose, salts, water) are reabsorbed into the blood as needed.
- Antidiuretic hormone (ADH) regulates the amount of water reabsorbed in the collecting ducts:
- High ADH → more water reabsorbed → concentrated urine → less water lost.
- Low ADH → less water reabsorbed → dilute urine → more water lost.
- This adjusts the osmotic concentration of blood.
🔍 Summary of Kidney Roles
| Process | What It Controls | Outcome |
|---|---|---|
| Excretion | Removes metabolic waste (urea) | Keeps blood clean and non-toxic |
| Osmoregulation | Regulates water and solute balance | Keeps blood osmotic concentration stable |
🧠 Why This is Important
Maintaining osmotic balance prevents cell shrinkage or swelling.
Removing wastes prevents toxicity and damage to organs.
Kidneys are vital for overall homeostasis and health.
Excretion removes harmful metabolic wastes; osmoregulation controls water and solute balance.
Kidneys filter blood, selectively reabsorb water and salts, and produce urine.
ADH hormone plays a key role in adjusting urine concentration to maintain blood osmotic balance.
Osmotic concentration is measured in osmoles per litre (osmol L⁻¹).
D3.3.8 – Role of Glomerulus, Bowman’s Capsule, and Proximal Convoluted Tubule in Excretion
🧬 Key Structures in Kidney Excretion
| Structure | Location | Function |
|---|---|---|
| Glomerulus | Network of capillaries inside Bowman’s capsule | Filters blood plasma under high pressure (ultrafiltration) |
| Bowman’s capsule | Cup-shaped structure surrounding the glomerulus | Collects the filtrate (filtered fluid) from blood |
| Proximal convoluted tubule (PCT) | Twisted tubule after Bowman’s capsule | Reabsorbs useful substances back into the blood |
🌿 Ultrafiltration at the Glomerulus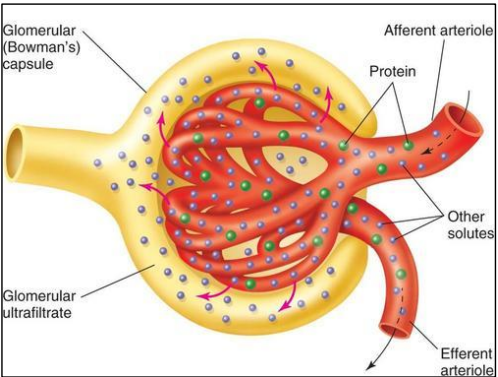
- Blood enters the glomerulus at high pressure.
- Small molecules (water, glucose, ions, urea) pass through capillary walls into Bowman’s capsule.
- Large molecules (proteins, blood cells) stay in the blood.
- This process is called ultrafiltration—it filters plasma based on size.
🔍 Filtrate in Bowman’s Capsule
The filtrate contains:
Water
Glucose
Ions (Na⁺, K⁺, Cl⁻)
Urea and other wastes
This fluid moves from Bowman’s capsule into the proximal convoluted tubule.
🧪 Reabsorption in the Proximal Convoluted Tubule
Most useful substances are actively and passively reabsorbed into blood:
- Glucose (all of it, normally)
- Ions (sodium, chloride, potassium)
- Water (by osmosis)
- Waste products like urea and toxins remain in the filtrate.
- Reabsorption keeps body fluids balanced and prevents loss of valuable molecules.
📌 Summary of Filtration and Reabsorption
| Process | What Happens | Purpose |
|---|---|---|
| Ultrafiltration | Blood plasma filtered through glomerulus into Bowman’s capsule | Removes plasma fluid and small solutes from blood |
| Reabsorption | Useful molecules reabsorbed in proximal tubule | Retains nutrients and balances ions and water |
| Excretion | Waste and excess substances remain in filtrate to be excreted | Removes toxins from body |
🧠 Why These Steps Are Important
Prevents loss of valuable substances like glucose and ions.
Ensures removal of metabolic wastes and toxins.
Maintains fluid and chemical balance in the body.
Glomerulus and Bowman’s capsule perform ultrafiltration to remove plasma fluid and small solutes.
Proximal convoluted tubule reabsorbs useful substances back into blood.
This process separates waste from useful molecules for excretion in urine.
Essential for maintaining body’s chemical balance and health.
D3.3.9 – Role of the Loop of Henle
🧠 What is the Loop of Henle?
A U-shaped part of the nephron tubule in the kidney.
Key role in concentrating urine and conserving water.
🌿 Structure of the Loop of Henle
| Part | Feature | Function |
|---|---|---|
| Descending limb | Permeable to water, impermeable to salts | Water leaves by osmosis into surrounding tissue |
| Ascending limb | Impermeable to water, actively transports sodium ions out | Pumps out Na⁺ to create high osmotic concentration in medulla |
🔬 How the Loop of Henle Works
- Active transport of sodium ions (Na⁺) in the ascending limb pumps Na⁺ into the medulla.
- This creates a high osmotic concentration in the surrounding medulla tissue.
- The high osmolarity draws water out of the descending limb and collecting ducts by osmosis.
- This mechanism allows kidneys to reabsorb water, producing concentrated urine and conserving water.
📍 Key Points
- The active transport of Na⁺ is essential to maintain the osmotic gradient.
- Water reabsorption happens where membranes are permeable (descending limb and collecting duct).
- Helps in water balance and preventing dehydration.
The loop of Henle establishes a high osmotic concentration in the medulla by pumping out sodium ions in the ascending limb.
This gradient allows water to be reabsorbed from the descending limb and collecting ducts.
Critical for concentrating urine and conserving body water.
D3.3.10 – Osmoregulation by Water Reabsorption in the Collecting Ducts
🧬 Key Concept: Osmoregulation via Water Reabsorption
The collecting ducts in the kidney control water reabsorption to maintain blood osmotic concentration.
This process is regulated by the hormone antidiuretic hormone (ADH).
🌿 Role of Osmoreceptors in the Hypothalamus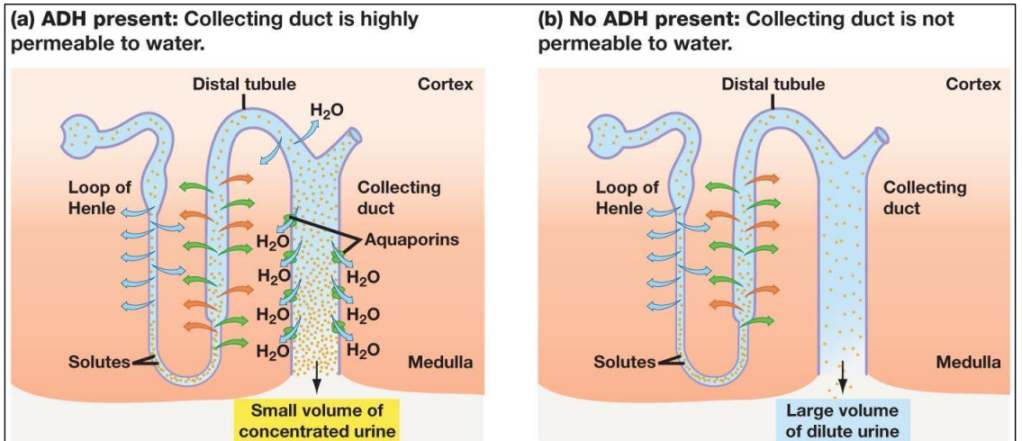
- Osmoreceptors are specialized nerve cells in the hypothalamus.
- They detect changes in blood osmotic concentration (how concentrated the blood is).
- If blood becomes too concentrated (high osmolarity), osmoreceptors send signals to increase ADH secretion.
- If blood is too dilute (low osmolarity), ADH secretion is reduced.
🔬 ADH Secretion by the Pituitary Gland
- ADH is released from the posterior pituitary gland into the bloodstream.
- The amount of ADH secreted depends on signals from osmoreceptors.
- More ADH → more water reabsorbed; less ADH → less water reabsorbed.
🧪 Aquaporins and Water Permeability
- Cells in the collecting ducts have aquaporin proteins that form water channels.
- Without ADH, aquaporins are mostly stored inside cells in intracellular vesicles → low water permeability → dilute urine.
- With ADH, aquaporins move to the cell membrane, increasing water permeability → more water reabsorbed → concentrated urine.
📍 How This Process Works
| Condition | Osmoreceptor Response | ADH Level | Aquaporins | Urine | Blood Osmolarity |
|---|---|---|---|---|---|
| High blood osmolarity (dehydrated) | Stimulated | Increased | Inserted into membrane | Concentrated (less water) | Decreases toward normal |
| Low blood osmolarity (overhydrated) | Inhibited | Decreased | Removed from membrane | Dilute (more water) | Increases toward normal |
🧠 Why This Mechanism Is Vital
- Prevents dehydration by conserving water.
- Prevents overhydration by excreting excess water.
- Maintains stable osmotic concentration of blood for normal cell function.
Osmoreceptors in the hypothalamus detect blood osmolarity changes and control ADH release.
ADH regulates water permeability of collecting duct cells by moving aquaporins to/from the membrane.
This system adjusts urine concentration to maintain water balance and osmotic homeostasis.
D3.3.11 – Changes in Blood Supply to Organs with Activity
🧬 Why Does Blood Supply Change?
- Blood flow adjusts to meet the changing demands of different organs during various states (sleep, rest, exercise).
- This ensures organs receive enough oxygen and nutrients and removes waste efficiently.
🌿 Patterns of Blood Supply to Key Organs
| Organ | During Sleep | During Wakeful Rest | During Vigorous Physical Activity |
|---|---|---|---|
| Skeletal muscles | Low blood flow (low demand) | Moderate blood flow | High blood flow to support increased activity |
| Gut (digestive system) | Moderate blood flow | Moderate to high blood flow | Reduced blood flow as digestion slows |
| Brain | Maintains relatively constant blood flow | Maintains steady blood flow | Blood flow remains constant to support brain function |
| Kidneys | Moderate blood flow (normal filtration) | Moderate blood flow | Reduced blood flow as blood is prioritized elsewhere |
🔍 Explanation of Changes
- Skeletal muscles:
- At rest or sleep, muscles need less oxygen → less blood flow.
- During exercise, muscles require more oxygen → vasodilation increases blood flow.
- Gut:
- Blood flow supports digestion, so it’s higher during eating and rest.
- During exercise, blood supply decreases as digestion slows and blood is redirected to muscles.
- Brain:
- Brain blood flow is kept constant to maintain vital functions regardless of activity.
- Kidneys:
- Blood flow supports filtration and waste removal.
- Reduced during exercise to prioritize muscles, but quickly returns to normal at rest.
📌 Summary Table: Blood Flow Changes
| Organ | Blood Flow Change | Reason |
|---|---|---|
| Skeletal muscle | Increases with activity | More oxygen and nutrients needed |
| Gut | Decreases during exercise | Digestion slows, blood redirected |
| Brain | Remains constant | Continuous function required |
| Kidneys | Decreases during exercise | Blood prioritized for muscles |
🧠 Why Is This Important?
- Ensures efficient use of blood to match organ needs.
- Supports survival and performance in different physiological states.
- Prevents overloading or under-supplying organs with blood.
Blood flow changes dynamically during sleep, rest, and exercise.
Muscles receive more blood during activity; gut and kidneys get less.
Brain blood flow is stable to support constant function.
This regulation is critical for maintaining homeostasis and meeting metabolic demands.
