NEET Biology - Unit 5- Body fluids and circulation- Study Notes - New Syllabus
NEET Biology – Unit 5- Body fluids and circulation- Study Notes – New Syllabus
Key Concepts:
- Body fluids and circulation: Composition of blood, blood groups, coagulation of blood; Composition of lymph and its function; Human circulatory system-Structure of human heart and blood vessels; Cardiac cycle, cardiac output, ECG, Double circulation; Regulation of cardiac activity; Disorders of circulatory system-Hypertension, Coronary artery disease, Angina pectoris, Heart failure.
Body Fluids and Circulation
🩸Composition of Blood
Blood is a fluid connective tissue that transports substances throughout the body.
It has two main components:
📌 A. Plasma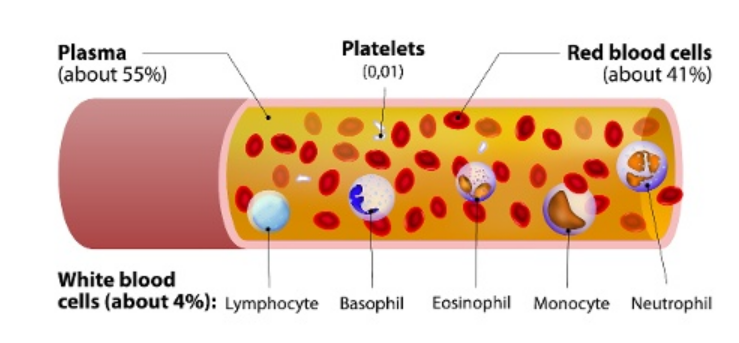
- Pale yellow, fluid part of blood
- Makes about 55 percent of blood
- Mostly water (90 to 92 percent)
- Contains:
- Proteins
- Albumins: maintain osmotic pressure
- Globulins: defense (antibodies)
- Fibrinogen: blood clotting
- Minerals: Na+, Ca2+, Mg2+, HCO3–
- Nutrients: glucose, amino acids, lipids
- Waste products: urea, uric acid
- Hormones and enzymes
Function: Helps transport materials, maintain pH and osmotic balance.
📌 B. Formed Elements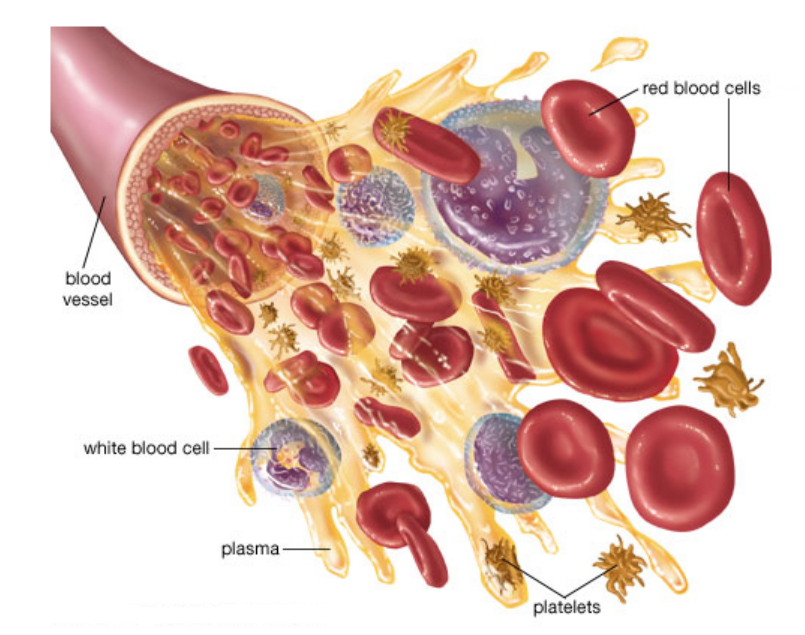
Make up 45 percent of blood.
Includes RBCs, WBCs and Platelets.
1. RBCs (Erythrocytes)
- Most abundant blood cells
- Formed in red bone marrow
- Biconcave, no nucleus
- Contain haemoglobin (Hb)
- Carry O₂ and CO₂
- Lifespan: 120 days
2. WBCs (Leucocytes)
- Nucleated, colourless
- Provide immunity
- Two types:
Granulocytes
- Neutrophils: most abundant, phagocytic
- Eosinophils: allergy response
- Basophils: least abundant, release histamine/serotonin during inflammation
Agranulocytes
- Lymphocytes: B and T cells (antibody formation and immunity)
- Monocytes: largest WBC, phagocytic
3. Platelets (Thrombocytes)
- Small cell fragments
- Essential for blood clotting
- Low count leads to excessive bleeding
🧬 Blood Groups
Blood grouping is mainly based on ABO system and Rh system.
A. ABO Blood Group System
Based on the presence or absence of A and B antigens on RBCs.
| Blood Group | Antigen on RBC | Antibody in Plasma | Can Receive | Can Donate |
|---|---|---|---|---|
| A | A | Anti-B | A, O | A, AB |
| B | B | Anti-A | B, O | B, AB |
| AB | A and B | None | All | AB |
| O | None | Anti-A + Anti-B | O | All |
O = universal donor
AB = universal recipient
B. Rh Factor (Positive / Negative)
- Rh antigen present → Rh+
- Rh antigen absent → Rh−
🔶 Rh Incompatibility
- Occurs when Rh− mother carries Rh+ fetus.
- First pregnancy safe
- During delivery → mixing of blood → mother forms anti-Rh antibodies
- Second Rh+ pregnancy → antibodies attack fetal RBCs
This causes Erythroblastosis Foetalis (fetal anemia + jaundice).
Prevented by giving anti-Rh antibodies to mother after 1st delivery.
🩹Coagulation of Blood (Blood Clotting)
Blood clotting prevents excessive blood loss after injury.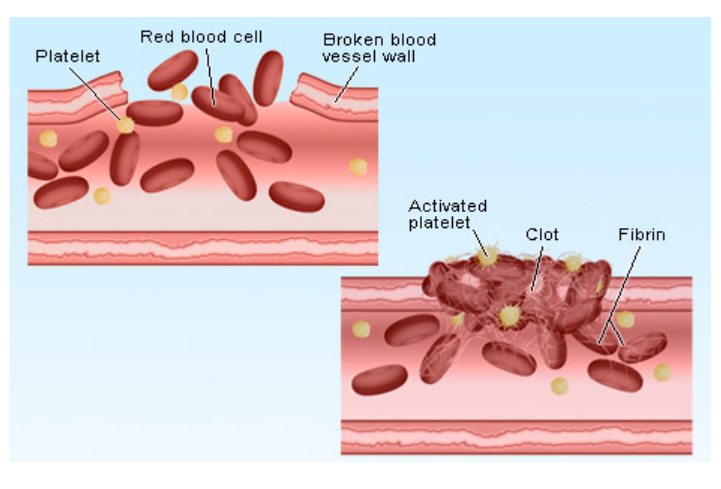
Steps in Clotting
- Injury to blood vessel → platelets release clotting factors
- Prothrombin (inactive) → gets converted to Thrombin (requires Thrombokinase + Ca2+)
- Thrombin converts Fibrinogen → Fibrin
- Fibrin forms a mesh that traps RBCs → forms a clot
Vitamin K is essential for making clotting proteins.
Calcium ions (Ca2+) activate various clotting steps.
📘 Quick Recap
Blood = plasma + formed elements
Plasma contains proteins (albumin, globulin, fibrinogen), nutrients, minerals
RBC: haemoglobin, O₂ transport, no nucleus
WBC: immunity (neutrophils phagocytic, lymphocytes antibody production)
Platelets: clotting
ABO groups: based on A/B antigens
Rh system important in pregnancy
Coagulation: prothrombin → thrombin → fibrin → clot
Lymph: Composition and Functions
🧪 Introduction
Lymph is a pale, slightly yellow fluid flowing inside lymphatic vessels.
It forms when some part of the fluid leaks out of blood capillaries into tissues.
The lymphatic system collects this leaked fluid and returns it to the bloodstream.
🧬 Composition of Lymph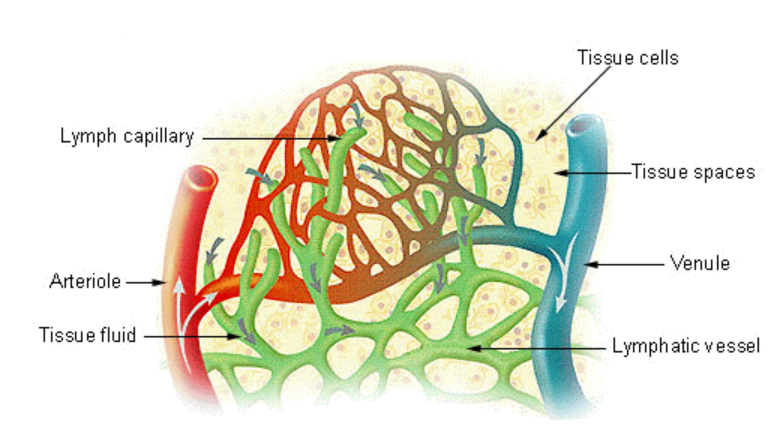
Lymph is similar to plasma but contains fewer proteins. It has the following components:
- Water – forms the major portion
- Proteins – low concentration, mostly antibodies
- Ions – Na+, K+, Ca2+, Cl-, HCO3-
- Lymphocytes – mainly T and B cells involved in immunity
- Fats – absorbed from intestine as chyle, giving lymph a milky look
- Glucose and amino acids – similar to plasma
- Cell debris and waste materials – collected from tissues
- Very few RBCs or platelets – almost absent normally
🌟 Functions of Lymph
1. Helps in Immunity
- Rich in lymphocytes
- Lymph nodes filter bacteria and viruses
- Important in antibody formation
2. Transports Fat from Intestine
- Intestinal villi contain lacteals that absorb dietary fats
- Fats enter lymph as chylomicrons
- Released into blood circulation later
3. Maintains Fluid Balance
- Collects excess tissue fluid
- Returns it to the venous system
- Prevents swelling or edema
4. Removes Waste from Tissues
- Clears cell debris and metabolic waste
- Keeps tissue spaces clean
5. Transports Hormones
- Carries hormones from glands to target organs
- Helps coordinate body functions
6. Provides Defence at Local Sites
- Lymph nodes trap microbes
- Node swelling shows active immune response
📘 Summary Table
| Feature | Details |
|---|---|
| Main Components | Water, low proteins, ions, lymphocytes, fats, glucose, waste |
| Cells Present | Mostly lymphocytes, very few RBCs or platelets |
| Appearance | Pale yellow, milky when rich in fats |
| Key Functions | Immunity, fat transport, fluid balance, waste removal, hormone transport |
📘 Quick Recap
Lymph is leaked tissue fluid collected by lymph vessels
Low in proteins, rich in lymphocytes
Transports fats from intestine through lacteals
Maintains tissue fluid balance and prevents edema
Removes waste and cell debris
Lymph nodes filter pathogens and support immunity
Also helps carry hormones across the body
Human Circulatory System
❤️ Structure of Human Heart
The human circulatory system is a closed, double circulation system.
It includes the heart, blood vessels, and blood.
Its main role is to transport oxygen, nutrients, hormones, and waste materials throughout the body.
🌱 Basic Features
- Muscular, hollow pumping organ
- About the size of a fist
- Located slightly left in the thoracic cavity
- Enclosed in double-walled pericardium with pericardial fluid that reduces friction
🫀 Chambers of the Heart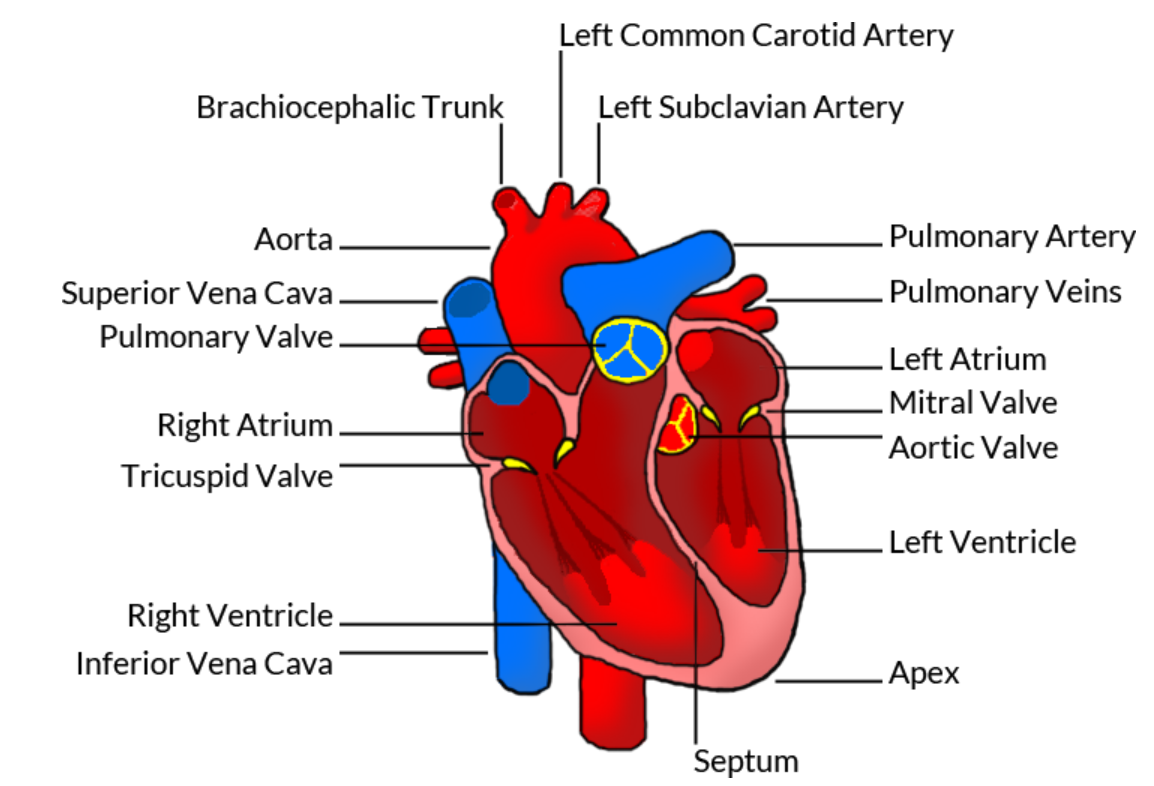
The heart has four chambers:
1. Right Atrium
- Receives deoxygenated blood from:
- Superior vena cava
- Inferior vena cava
- Coronary sinus
- Thin-walled chamber
2. Right Ventricle
- Pumps deoxygenated blood to lungs through pulmonary artery
- Thicker walls than atrium
3. Left Atrium
- Receives oxygenated blood from lungs via pulmonary veins
- Thin-walled
4. Left Ventricle
- Thickest cardiac wall
- Pumps oxygenated blood to the entire body through aorta
📌 Why is left ventricle thicker?
It pumps blood to the entire body, so it needs stronger muscles.
🔒 Heart Valves (One-way movement)
1. Tricuspid valve
- Between right atrium and right ventricle
- Prevents backflow into right atrium
2. Bicuspid / Mitral valve
- Between left atrium and left ventricle
- Prevents backflow into left atrium
3. Semilunar valves
- Present at openings of:
- Aorta
- Pulmonary artery
- Prevent backflow into ventricles
Nodal System (Pacemaker of the Heart)
- SA Node (Sinoatrial Node) – in right atrium, generates impulse, natural pacemaker
- AV Node (Atrioventricular Node) – receives impulse from SA node, delays it for ventricular filling
- AV Bundle (Bundle of His) and Purkinje Fibres – spread impulse throughout ventricles for coordinated contraction
Impulse pathway:
SA Node → AV Node → Bundle of His → Purkinje Fibres
🫀 Blood Vessels
🌱 Types of Blood Vessels
1. Arteries
- Carry blood away from the heart
- Usually carry oxygenated blood (except pulmonary artery)
- Thick, muscular, elastic walls
- High pressure
- Narrow lumen
2. Veins
- Carry blood toward the heart
- Usually carry deoxygenated blood (except pulmonary vein)
- Thin, less elastic walls
- Contain valves to prevent backflow
- Low pressure
- Wide lumen
3. Capillaries
- Microscopic thin-walled vessels
- Connect arteries and veins
- Single layer of endothelium
- Main site for exchange of gases, nutrients, and wastes
📊 Summary Table: Arteries vs Veins vs Capillaries
| Feature | Arteries | Veins | Capillaries |
|---|---|---|---|
| Direction | Away from heart | Toward heart | Connect arteries and veins |
| Oxygen content | Mostly oxygenated | Mostly deoxygenated | Mixed exchange |
| Wall thickness | Thick, muscular | Thin, less muscular | One-cell thick |
| Pressure | High | Low | Very low |
| Valves | Absent | Present | Absent |
| Lumen | Narrow | Wide | Very narrow |
| Function | Distribution | Collection | Exchange |
📦 Quick Recap
Heart has four chambers: RA, RV, LA, LV
Tricuspid valve on right side, bicuspid valve on left
Semilunar valves guard aorta and pulmonary artery
SA node is the natural pacemaker
Arteries carry blood away, veins bring blood back
Capillaries are the exchange sites
Left ventricle has the thickest wall
Cardiac Cycle, Cardiac Output, ECG and Double Circulation
🌱 Introduction
The heart works in a rhythmic sequence of contraction and relaxation to pump blood.
This complete sequence in one heartbeat is known as the cardiac cycle.
Understanding it helps explain blood movement, heart sounds, and ECG wave formation.
🔄 Cardiac Cycle
What is a cardiac cycle?
One complete heartbeat that includes atrial systole, ventricular systole, and joint diastole.
⏱ Duration: 0.8 seconds
- Atrial systole: 0.1 s
- Ventricular systole: 0.3 s
- Joint diastole: 0.4 s
🫀 Phases of the Cardiac Cycle
1. Atrial Systole (0.1 sec)
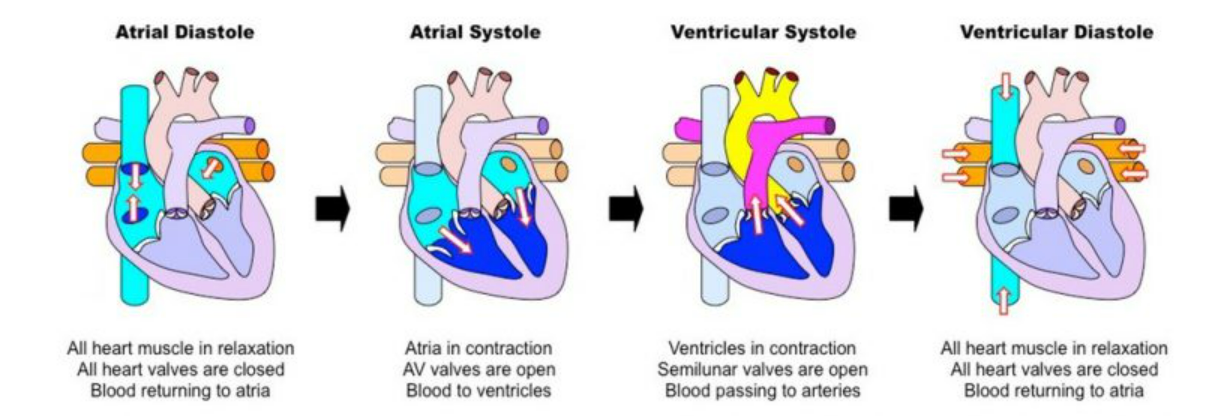
- SA node triggers contraction of atria
- Blood moves into ventricles
- AV valves remain open
- Semilunar valves stay closed
2. Ventricular Systole (0.3 sec)
- Ventricles contract powerfully
- AV valves close
- Produces the first heart sound “Lubb”
- Semilunar valves open
- Blood moves into:
- Aorta (from left ventricle)
- Pulmonary artery (from right ventricle)
3. Joint Diastole (0.4 sec)
- Atria and ventricles relax together
- Semilunar valves close
- Produces the second heart sound “Dubb”
- AV valves open
- Ventricles fill passively with blood
❤️🔥 Cardiac Output
What is Cardiac Output (CO)?
Amount of blood pumped by each ventricle per minute.
Formula
Cardiac Output = Stroke Volume × Heart Rate
- Stroke Volume (SV): approx 70 ml per beat
- Heart Rate (HR): approx 72 beats/min
Normal CO
70 ml × 72 = ~5000 ml/min (5 L/min)
This means the heart pumps almost the entire blood volume every minute.
🫀 ECG (Electrocardiogram)
What is ECG?
A graphical record of electrical activity of the heart during each cardiac cycle.
Helps diagnose:
- Arrhythmia
- Heart block
- Damage to heart muscle
🔋 Waves of ECG
1. P Wave
- Represents atrial depolarization
- Atria prepare to contract
2. QRS Complex
- Represents ventricular depolarization
- Ventricles contract
- Largest spike due to thicker ventricular walls
3. T Wave
- Represents ventricular repolarization
- Ventricles relax
Atrial repolarization is hidden by the QRS complex.
🔁 Double Circulation
What is Double Circulation?
Blood passes through the heart twice during one full circulation of the body.
This occurs because humans have two separate circuits.
1. Pulmonary Circulation
Right ventricle → Pulmonary artery → Lungs → Pulmonary veins → Left atrium
Purpose:
- CO2 is released
- O2 is absorbed
2. Systemic Circulation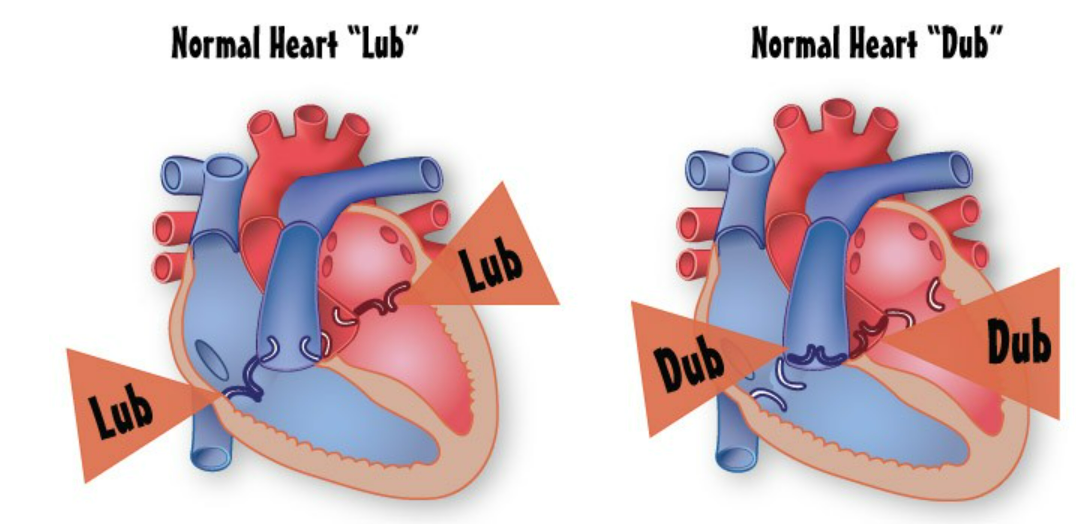
Left ventricle → Aorta → Body organs → Vena cava → Right atrium
Purpose:
- Supplies oxygen and nutrients to tissues
⭐ Importance of Double Circulation
- Prevents mixing of oxygenated and deoxygenated blood
- Maintains high pressure for efficient transport
- Supports warm-blooded metabolism
📊 Summary Table
| Concept | Key Points |
|---|---|
| Cardiac Cycle | Atrial systole → Ventricular systole → Joint diastole (0.8 sec) |
| Heart Sounds | Lubb: AV valves close, Dubb: Semilunar valves close |
| Cardiac Output | SV × HR = ~5 L/min |
| ECG Waves | P: atria, QRS: ventricles contract, T: ventricles relax |
| Double Circulation | Pulmonary + Systemic circuits |
📦 Quick Recap
Cardiac cycle = 0.8 seconds
Atrial systole → Ventricular systole → Joint diastole
Cardiac Output ≈ 5 L/min
ECG waves: P, QRS, T
Double circulation: Pulmonary + Systemic loops
Regulation of Cardiac Activity
🌱 Introduction
The heart beats automatically due to its pacemaker (SA node).
Heart activity is modified according to body needs and controlled by:
- Nervous system
- Hormones
- Reflexes (feedback mechanisms)
- Temperature & ions
Purpose: Maintain blood pressure, oxygen supply, and tissue perfusion.
1. Intrinsic Pacemaker: SA Node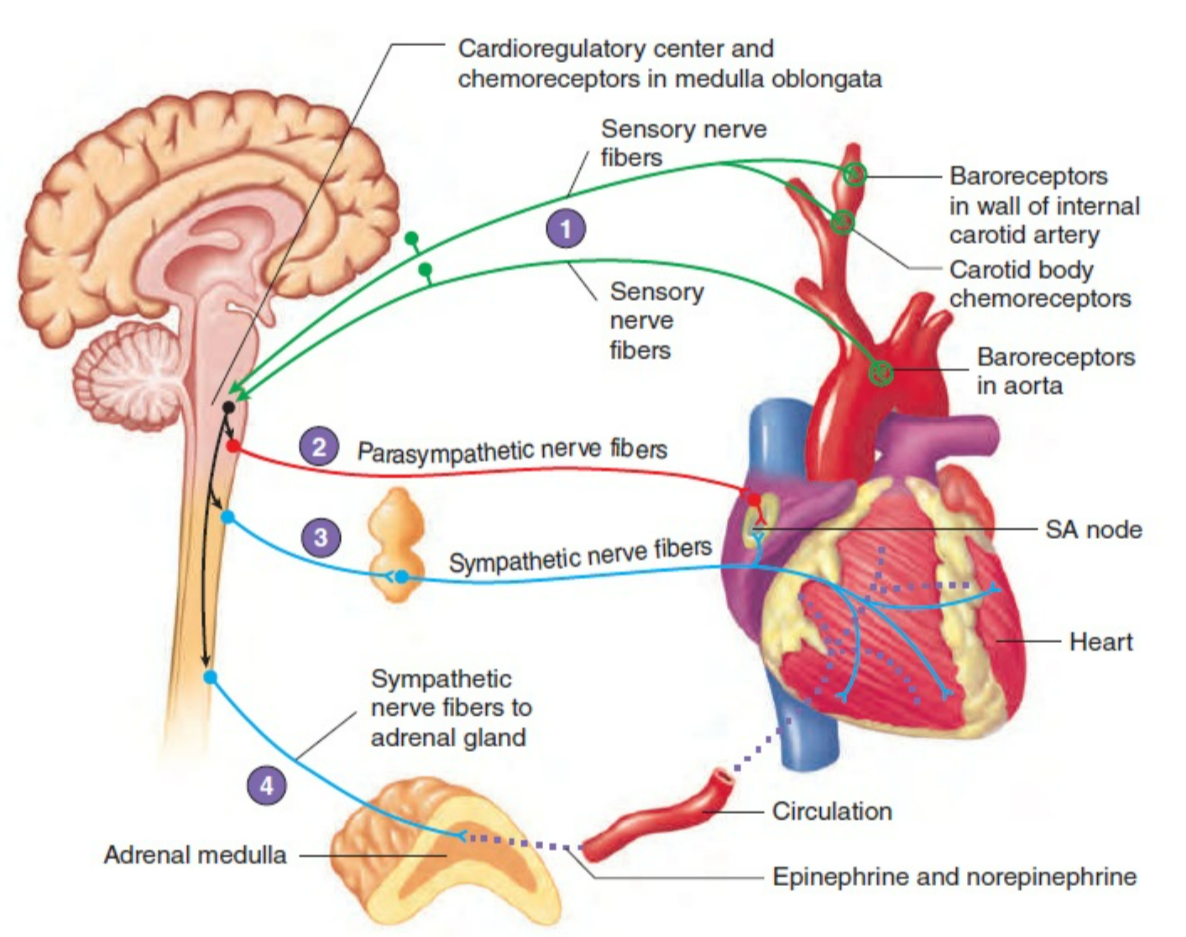
- Location: Right atrium near superior vena cava
- Function: Generates electrical impulses → sets basic heart rhythm (~70 bpm)
- Significance: Heart can beat independently, but needs modulation during exercise, stress, or rest
2. Nervous Regulation of Heartbeat
The Autonomic Nervous System (ANS) modifies SA node activity:
a) Sympathetic Nervous System (SNS)
- Function: Increases heart activity
- Nerve: Accelerator nerve
- Effects:
- ↑ Heart rate (HR)
- ↑ Force of contraction → ↑ Stroke volume → ↑ Cardiac output (CO)
- Neurotransmitter: Noradrenaline (Norepinephrine)
- Active during: Exercise, stress, fear, low BP
- Mnemonic: “Stress & Sprint” → heart beats faster and stronger
b) Parasympathetic Nervous System (PNS)
- Function: Decreases heart activity
- Nerve: Vagus nerve
- Effects:
- ↓ Heart rate
- Slight ↓ in contraction force
- Conserves energy
- Neurotransmitter: Acetylcholine
- Active during: Rest, relaxation, sleep
- Mnemonic: “Pause & Nap” → heart slows down
Key Point: SNS → “fight or flight,” affects rate & force; PNS → “rest & digest,” mainly affects rate
3. Hormonal Regulation
| Hormone | Source | Effect on Heart | When Active |
|---|---|---|---|
| Adrenaline / Noradrenaline | Adrenal medulla | ↑ HR, ↑ Stroke volume, ↑ CO | Stress, fear, excitement |
| Thyroxine | Thyroid gland | ↑ HR, ↑ Force of contraction | High metabolic rate, chronic effect |
Mechanism: Adrenaline → β1 receptors of SA node & myocardium → faster & stronger heartbeats; Thyroxine ↑ metabolic rate → stronger, faster beats
4. Reflex Control (Feedback Mechanisms)
Maintains homeostasis by monitoring BP, O₂, CO₂, and pH:
a) Baroreceptor Reflex
- Location: Carotid sinus & aorta
- BP ↑ → Parasympathetic ↑ → HR ↓
- BP ↓ → Sympathetic ↑ → HR ↑
b) Chemoreceptor Reflex
- Location: Carotid & aortic bodies
- Detects O₂, CO₂, and pH changes
- Low O₂ / High CO₂ / Low pH → Sympathetic ↑ → HR ↑
- Ensures oxygen delivery matches tissue needs
5. Temperature and Ion Effects
| Factor | Effect on Heart |
|---|---|
| High body temperature | ↑ HR (faster metabolism) |
| Low body temperature | ↓ HR |
| K⁺ (excess) | Slows or stops heart (hyperkalemia) |
| Ca²⁺ | ↑ Force of contraction (positive inotrope) |
| Na⁺ | Alters excitability |
| Mg²⁺ | Excess → slows HR |
Note: Ions are crucial for cardiac action potential generation
⚡ Quick Recap
SA Node → Pacemaker, intrinsic rhythm
SNS → ↑ HR & force, Noradrenaline, active during exercise/stress
PNS → ↓ HR, Acetylcholine, active during rest/sleep
Hormones → Adrenaline & Thyroxine ↑ HR & force
Baroreceptor Reflex → BP feedback → HR adjustment
Chemoreceptor Reflex → O₂/CO₂/pH feedback → HR adjustment
Temperature/Ions → ↑ Temp → ↑ HR, K⁺ excess → slows HR, Ca²⁺ ↑ force
Disorders of the Circulatory System
🌱 Introduction
The circulatory system can develop problems when blood flow reduces, gets blocked, or when the heart becomes weak.
These disorders commonly arise due to lifestyle habits, ageing, stress, or genetic factors.
Here are the four major disorders you need to remember for exams.
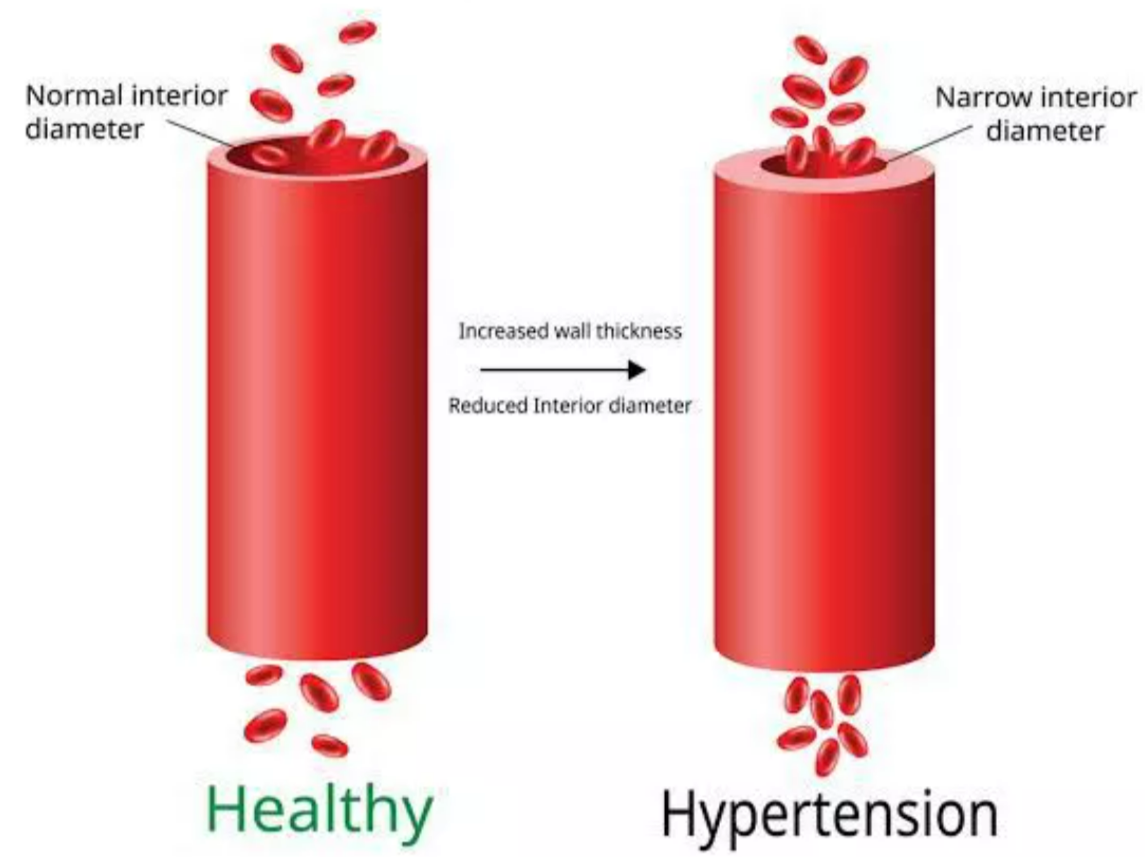
1. Hypertension (High Blood Pressure)
What it means
A condition where blood pressure stays higher than normal for a long time.
- Normal BP: 120/80 mm Hg
 Hypertension: 140/90 mm Hg or above (persistent)
Hypertension: 140/90 mm Hg or above (persistent)
Why it happens
- Stress
- High salt intake
- Obesity
- Lack of exercise
- Smoking and alcohol
- Heredity
- Kidney diseases
Effects on the body
- Damages blood vessels
- Can lead to stroke
- Increases risk of heart attack
- Affects kidney function
- Causes thickening of artery walls
Symptoms
- Usually silent (no symptoms)
- Sometimes headache, dizziness, tiredness
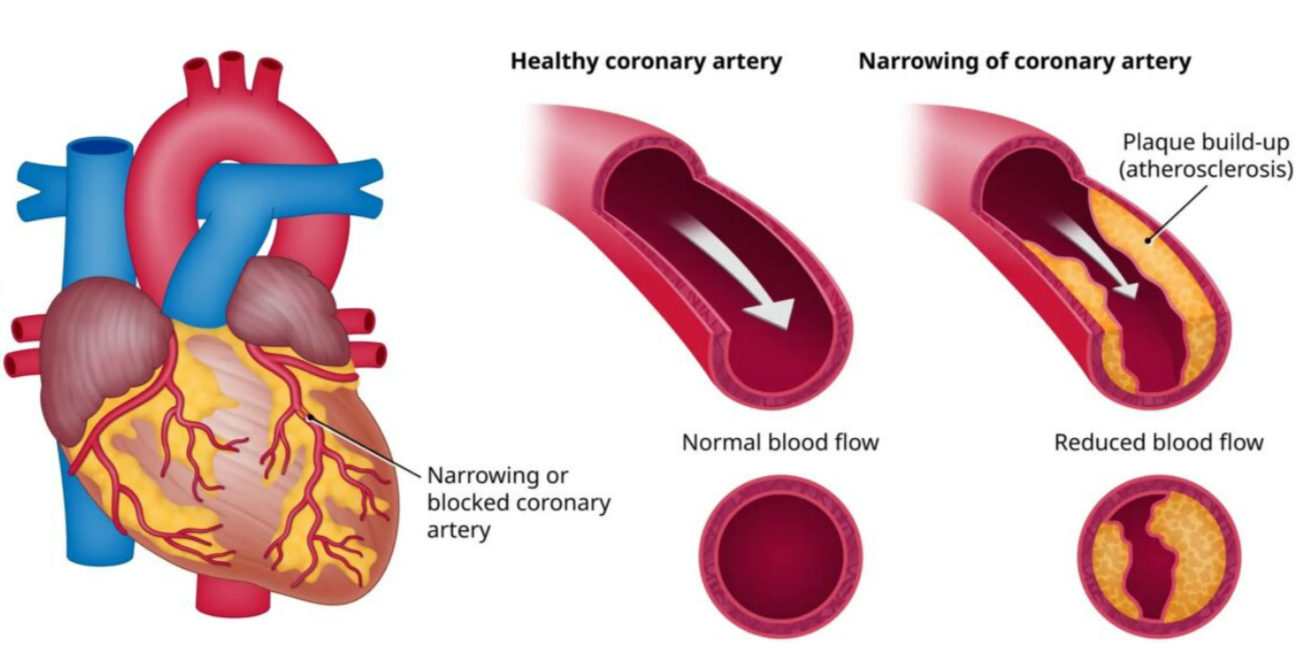
2. Coronary Artery Disease (CAD)
What it means
Also called atherosclerosis.
Fatty deposits (plaques) build up in coronary arteries, narrowing them and reducing blood supply to heart muscles.
Causes
- High cholesterol
- Smoking

- Diabetes
- Hypertension
- Obesity
- Unhealthy diet
- Sedentary lifestyle
Effects
- Less oxygen reaches heart muscles
- Can cause angina
- May lead to heart attack
- Can result in heart failure
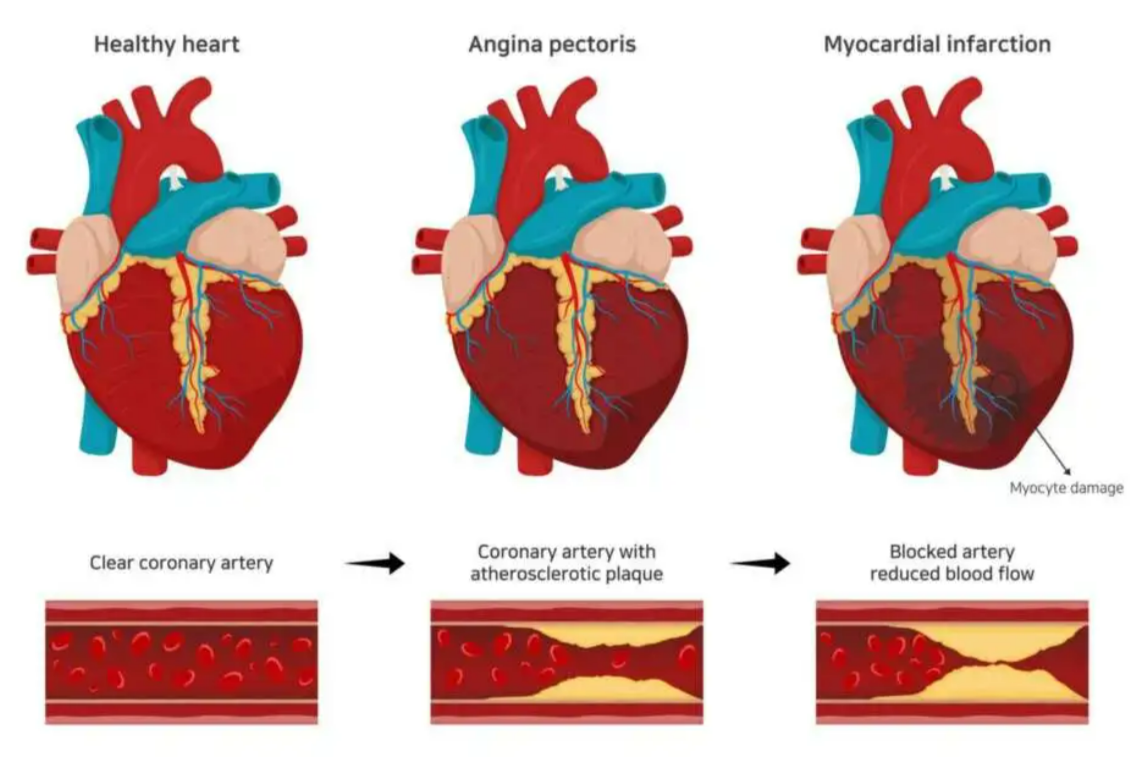
3. Angina Pectoris
What it means
A sudden chest pain caused by temporary lack of oxygen to heart muscles.
Occurs when coronary arteries are narrowed but not fully blocked.
When does it occur?
- During physical exertion

- Emotional stress
- After a heavy meal
- Exposure to cold
Symptoms
- Chest pain or tightness
- Pain spreading to arm, neck, or jaw
- Shortness of breath
Key point
Pain goes away with rest or nitroglycerin.
4. Heart Failure
What it means
Also called congestive heart failure (CHF).
The heart becomes too weak to pump enough blood to meet body needs.
Causes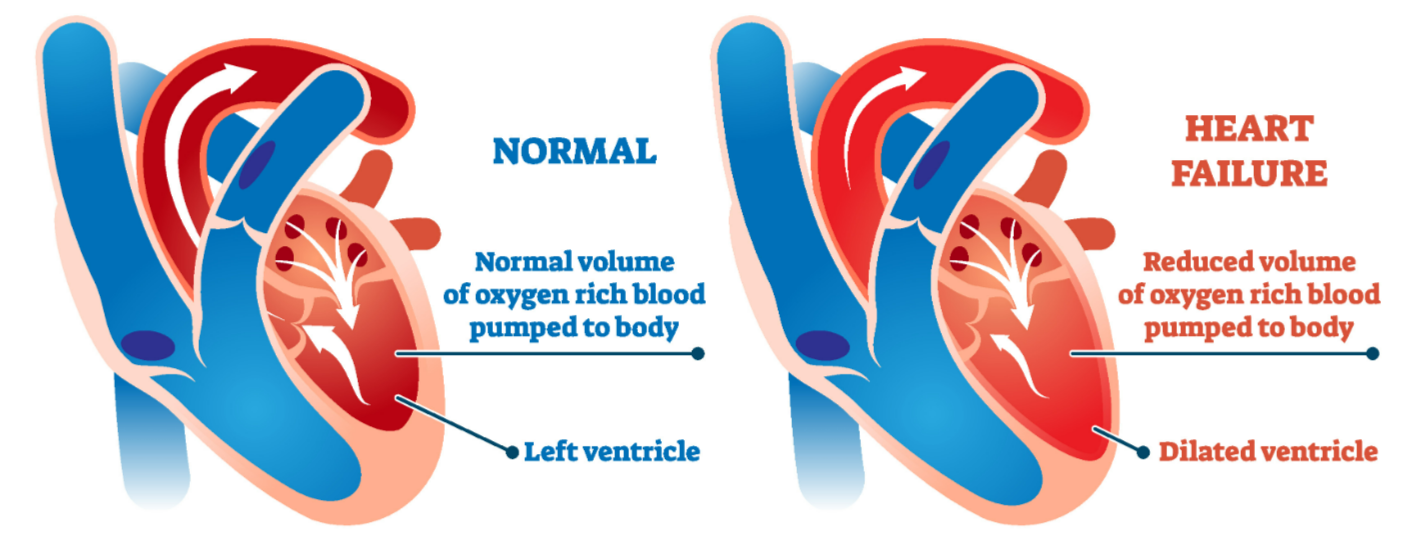
- Long-term hypertension
- Coronary artery disease
- Heart attack
- Valve disorders
- Cardiomyopathy
- Severe anemia or thyroid problems (rare)
Effects
- Fluid accumulation in lungs
- Swelling in legs (edema)
- Fatigue
- Difficulty breathing
- Reduced exercise capacity
Types
- Left-side failure: breathlessness, lung congestion
- Right-side failure: swelling in legs, liver enlargement
🗂️ Summary Table
| Disorder | What Happens | Main Cause | Key Features |
|---|---|---|---|
| Hypertension | Persistent high BP | Lifestyle, heredity | Silent, damages vessels |
| CAD | Coronary arteries narrow | Fat + cholesterol deposition | Less blood to heart |
| Angina | Temporary chest pain | Reduced coronary supply | Pain relieved by rest |
| Heart Failure | Heart too weak to pump | CAD, hypertension | Breathlessness, edema |
📦 Quick Recap
Hypertension: High BP above 140/90, damages vessels and organs
CAD: Fat deposits narrow coronary arteries, reduces oxygen to heart
Angina: Chest pain during exertion, relieved by rest or medication
Heart Failure: Weak pumping action, causes edema and breathlessness