NEET Biology - Unit 5- Excretory products and their elimination- Study Notes - New Syllabus
NEET Biology – Unit 5- Excretory products and their elimination- Study Notes – New Syllabus
Key Concepts:
- Excretory products and their elimination: Modes of excretion- Ammonotelism, ureotelism, uricotelism; Human excretory system-structure and fuction; Urine formation, Osmoregulation; Regulation of kidney function-Renin-angiotensin, Atrial Natriuretic Factor, ADH and Diabetes insipidus; Role of other organs in excretion; Disorders; Uraemia, Renal failure, Renal calculi, Nephritis; Dialysis and artificial kidney.
Modes of Excretion
🌱 Introduction
All organisms produce nitrogenous wastes while breaking down proteins and nucleic acids.
Major wastes include ammonia, urea, and uric acid.
These are toxic and must be removed. The excretory mode depends on:
- Habitat (aquatic or terrestrial)
- Water availability
- Energy available
- Toxicity tolerance of the organism
This gives three major modes of excretion.
🌊 1. Ammonotelism
Meaning: Excretion of nitrogenous wastes mainly as ammonia.
Properties of Ammonia
- Highly toxic
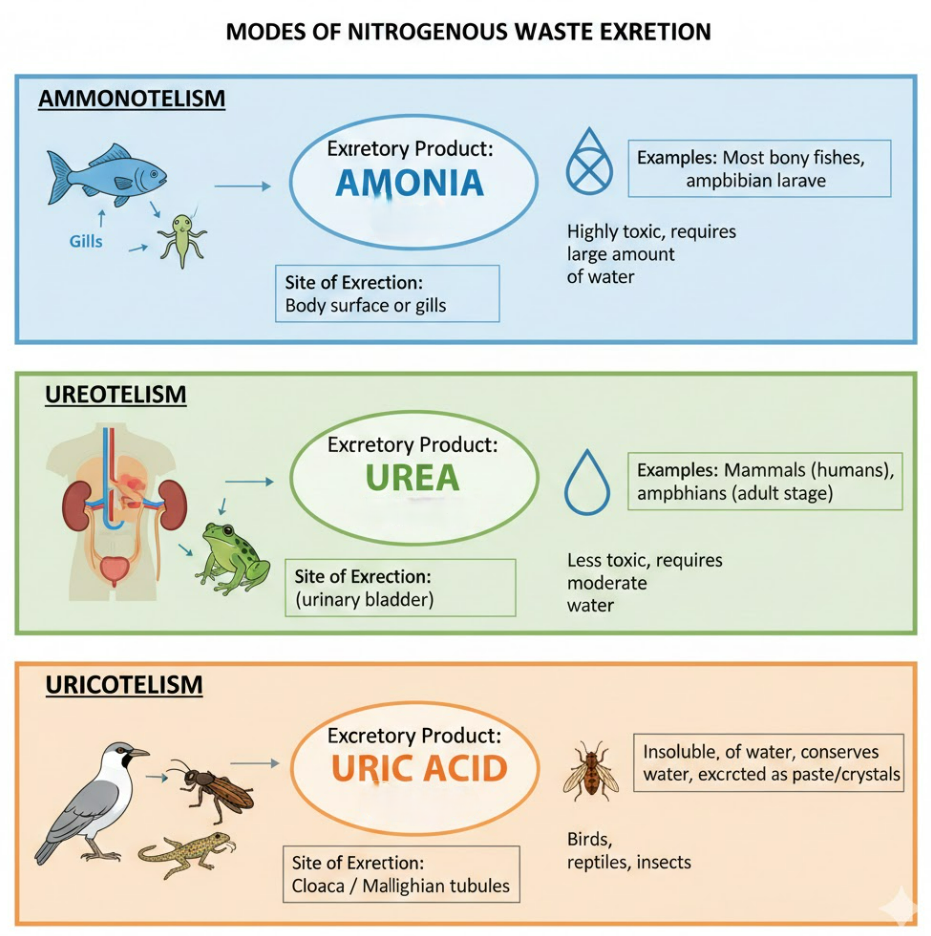
- Very soluble in water
- Cannot be stored in body
- Requires maximum water for removal
Why aquatic animals are ammonotelic
- Surrounded by water for easy diffusion
- Very low energy requirement
Mechanism of excretion
- Diffusion through body surface
- Diffusion through gills (main route in fishes)
Examples
- Bony fishes (teleosts)
- Tadpoles
- Aquatic invertebrates
⭐ Key Points
- Needs maximum water
- Diffusion is the main method
- Most toxic, cannot be stored
🧪 2. Ureotelism
Meaning: Excretion of nitrogenous waste mainly as urea.
Properties of Urea
- Moderately toxic
- Needs moderate water
- Can be stored for short periods
Why useful for terrestrial life
- Helps conserve water
Formation (Urea Cycle)
- Formed in liver through Ornithine Cycle
- Ammonia → Urea → Blood → Kidneys → Urine
Examples
- Mammals (including humans)
- Adult amphibians
- Many marine fishes
⭐ Key Points
- More energy used than ammonotelism
- Needs less water than ammonia
- Major excretory product in humans
🕊️ 3. Uricotelism
Meaning: Excretion of nitrogenous waste mainly as uric acid.
Properties of Uric Acid
- Least toxic
- Needs minimum water
- Excreted as semi-solid paste or crystals
Why useful
- Perfect for dry habitats
- Ideal for egg-laying species because uric acid is non-toxic inside eggs
Examples
- Birds
- Reptiles
- Land snails
- Most insects
⭐ Key Points
- Maximum water conservation
- Lowest toxicity
- Excreta is semi-solid
🧩 Why 3 Modes Exist
| Waste | Toxicity | Water Needed | Energy Needed | Suitable For |
|---|---|---|---|---|
| Ammonia | Very high | Very high | Least | Aquatic animals |
| Urea | Moderate | Moderate | Moderate | Mammals, amphibians |
| Uric acid | Lowest | Very low | Highest | Birds, reptiles, insects |
🗂️ Summary Table: Modes of Excretion
| Mode | Main Waste | Toxicity | Water Requirement | Examples | Special Notes |
|---|---|---|---|---|---|
| Ammonotelism | Ammonia | Highest | Max | Bony fishes, tadpoles | Diffusion via gills/skin |
| Ureotelism | Urea | Moderate | Moderate | Humans, mammals | Urea cycle in liver |
| Uricotelism | Uric acid | Lowest | Minimum | Birds, reptiles, insects | Semisolid paste, saves water |
🧠 Quick Recap
Ammonotelic → ammonia, aquatic animals, most toxic, needs maximum water.
Ureotelic → urea, mammals, moderate toxicity and water loss.
Uricotelic → uric acid, birds and reptiles, least toxic, least water.
Toxicity: Ammonia > Urea > Uric acid.
Water requirement follows same sequence.
Energy needed is highest for uric acid.
Human Excretory System
🌱 Introduction
The human excretory system removes nitrogenous wastes and maintains water, salt, and acid–base balance to keep the body in homeostasis.
Major wastes:
- Urea
- Uric acid
- Creatinine
- Excess salts, ions, water
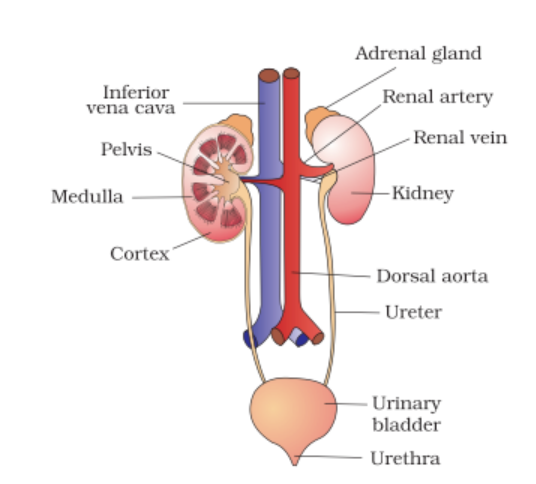
The excretory system includes:
- Kidneys
- Ureters
- Urinary bladder
- Urethra
- Nephrons (functional unit)
🧬 1. Kidneys
Structure
- Two bean-shaped organs in the abdominal cavity on either side of the vertebral column.
- Right kidney slightly lower due to liver.
- Outer surface convex, inner surface concave.

Hilum
A notch on inner concave side, serving as entry/exit for:
- Renal artery
- Renal vein
- Ureter
- Nerves
Internal Structure
Kidney has two major zones:
Renal Cortex
- Outer dark region
- Contains most nephrons (glomerulus + PCT + DCT)
- Highly vascular
Renal Medulla
- Inner lighter region
- Contains 8 to 18 medullary pyramids
- Pyramid tips end as renal papillae opening into minor calyces
Renal Pelvis
- Funnel-shaped cavity collecting urine from calyces
- Continues as ureter
🔁 2. Nephron: Structural and Functional Unit
Each kidney has about 1–1.5 million nephrons.
Parts of a Nephron
A. Renal Corpuscle
Glomerulus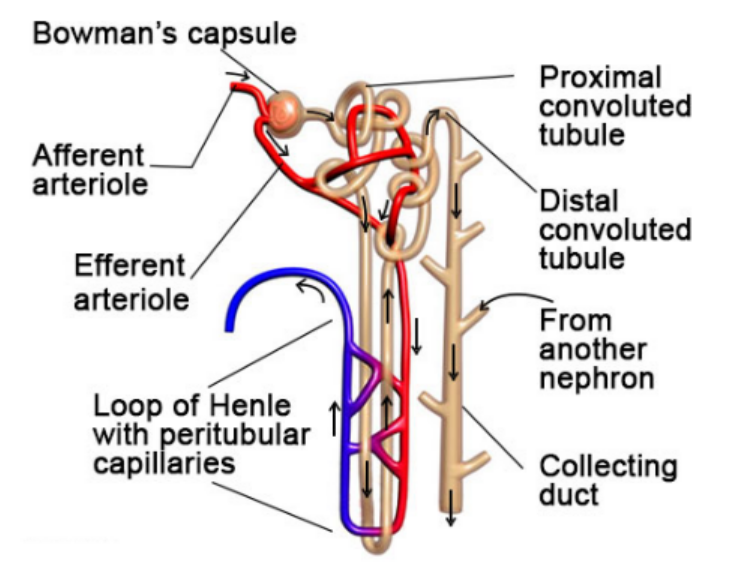
- Tuft of capillaries
- Afferent arteriole brings blood; efferent removes it
- High pressure aids filtration
Bowman’s Capsule
- Double-walled cup-like structure
- Inner layer has podocytes with filtration slits
B. Renal Tubule
Proximal Convoluted Tubule (PCT)
- Highly coiled
- Brush-border cells increase absorption area
Loop of Henle
- Descending limb: permeable to water
- Ascending limb: impermeable to water, transports ions
Distal Convoluted Tubule (DCT)
- Makes final adjustments to ion balance
- Hormone-sensitive
Collecting Duct
- Receives urine from multiple nephrons
- Concentrates urine via water reabsorption
📌 Types of Nephrons
| Type | Location | Loop of Henle | Function |
|---|---|---|---|
| Cortical | Cortex | Short | Normal urine formation |
| Juxtamedullary | Near medulla | Long | Concentrated urine (counter-current mechanism) |
🚿 3. Ureters
- Slender muscular tubes (25–30 cm)
- Carry urine from renal pelvis to bladder via peristalsis
- Oblique entry prevents backflow
🫙 4. Urinary Bladder
- Hollow muscular organ for urine storage
- Has detrusor muscle
- Stores 300–500 ml urine comfortably
🚪 5. Urethra
- Carries urine out of body
- Internal sphincter: involuntary
- External sphincter: voluntary
- Males: longer, for urine + semen
- Females: shorter, only for urine
⚙️ Functions of the Human Excretory System
1. Removal of Nitrogenous Wastes
- Urea formed in liver (urea cycle)
- Excreted by kidneys
2. Regulation of Water Balance
- Kidneys adjust water reabsorption
- ADH controls water reabsorption
3. Regulation of Ion Balance
- Maintains sodium, potassium, calcium, chloride, bicarbonate levels
4. Maintenance of Acid–Base Balance
- Reabsorbs bicarbonate
- Excretes hydrogen ions
5. Regulation of Blood Pressure
- Juxtaglomerular cells release renin
- Activates RAAS, increases BP
6. Removal of Toxins and Drugs
- Filters harmful chemicals and medicines
7. Hormone Secretion
- Erythropoietin
- Renin
- Calcitriol
🗂️ Summary Table: Human Excretory System Components
| Part | Structure | Key Function |
|---|---|---|
| Kidneys | Bean-shaped, cortex + medulla | Filtration, reabsorption, secretion, urine formation |
| Nephron | Glomerulus + tubules | Functional urine-forming unit |
| Ureters | Muscular tubes | Conduct urine to bladder |
| Urinary bladder | Stretchable sac | Stores urine |
| Urethra | Exit tube | Releases urine |
📦 Quick Recap
Kidneys filter 1100–1200 ml blood per minute.
Nephron = filtration + reabsorption + secretion.
Cortex has most nephrons; medulla has pyramids.
Juxtamedullary nephrons with long loop concentrate urine.
Ureters use peristalsis to move urine.
Bladder stores urine; urethra removes it.
Kidneys maintain water, salts, pH, and BP.
Produce renin, erythropoietin, calcitriol.
Urine Formation & Osmoregulation
🌱 Introduction
The kidneys filter blood to remove nitrogenous wastes and maintain water and ion balance.
Urine formation happens inside nephrons and ensures body stays chemically stable.
🧪 1. Urine Formation
Urine formation occurs in three sequential steps:
A. Ultrafiltration (Glomerular Filtration)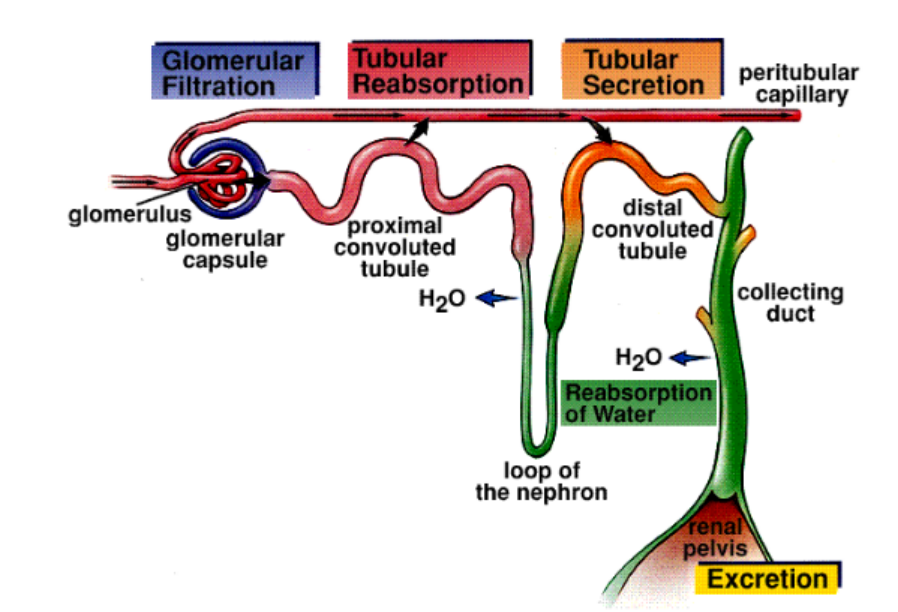
Where: Glomerulus + Bowman’s capsule
What happens:
- Blood enters glomerulus under high pressure
- Plasma minus proteins filtered into Bowman’s capsule
- Filtrate formed = glomerular filtrate
Key Points:
- Glomerular Filtration Rate (GFR) = 125 mL/min
- Daily filtrate = ~180 L
- Filtration barrier:
- Endothelium of glomerular capillaries
- Basement membrane
- Podocytes with filtration slits
Mnemonic: EBP → Endothelium, Basement membrane, Podocytes
B. Selective Reabsorption
Where: PCT, Loop of Henle, DCT, Collecting duct
What happens: Useful substances reabsorbed into blood
In PCT:
- Maximum reabsorption
- Glucose, amino acids, vitamins → 100%
- Na+, K+, Cl– actively absorbed
- Water follows by osmosis
- Brush border increases surface area
In Loop of Henle:
- Descending limb → permeable to water
- Ascending limb → permeable to salts
- Creates medullary concentration gradient
In DCT & Collecting Duct:
- Hormone-controlled reabsorption (aldosterone, ADH)
C. Tubular Secretion
Where: DCT and Collecting Tubule
What happens:
- H+, K+, creatinine, drugs secreted into filtrate
- Maintains acid-base balance
Final Urine Composition:
- Water
- Urea
- Creatinine
- Uric acid
- Variable salts
⚖️ 2. Osmoregulation
Osmoregulation ensures correct water and salt balance in the body.
A. Role of ADH (Antidiuretic Hormone)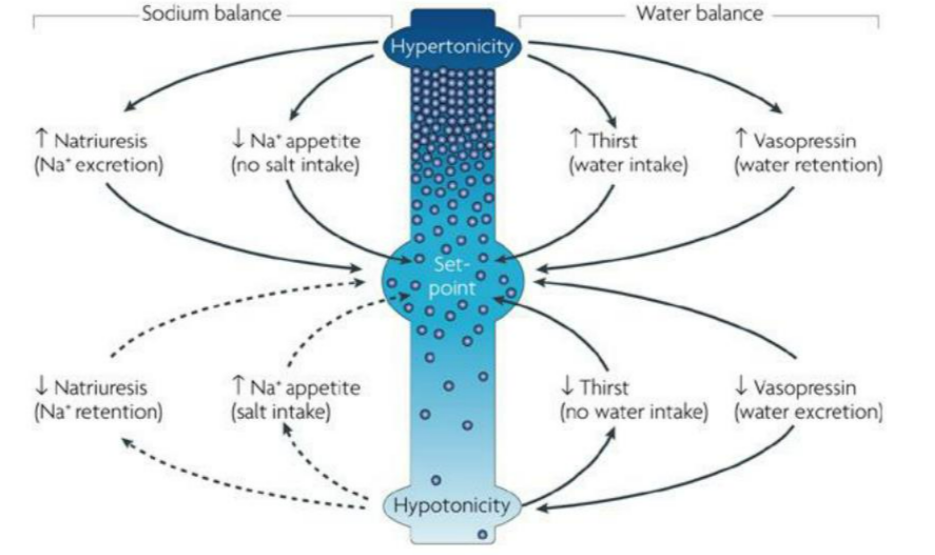
- Released from posterior pituitary
- Increases water reabsorption in collecting ducts
- Makes urine concentrated
- Low ADH → large volume of dilute urine (diabetes insipidus)
B. Aldosterone
- Released from adrenal cortex
- Reabsorbs Na+, secretes K+ in DCT and collecting duct
- Water follows sodium indirectly
- Maintains blood pressure and volume
C. Counter-Current Mechanism
- Created by Loop of Henle (descending vs ascending) and Vasa recta
- Descending limb loses water
- Ascending limb pumps out salts
- Vasa recta maintains gradient (opposite flow)
- Leads to highly concentrated medulla → helps produce concentrated urine
Simple trick: Loop creates gradient, Vasa recta preserves it.
📊 Summary Table
| Process | Location | Key Features |
|---|---|---|
| Ultrafiltration | Glomerulus | High pressure filtration of blood |
| Selective Reabsorption | PCT, Loop, DCT | Useful substances recovered |
| Tubular Secretion | DCT, CT | Removal of extra ions, toxins, drugs |
| ADH Action | Collecting duct | Water reabsorption; prevents dehydration |
| Aldosterone | DCT, CT | Na+ reabsorption; K+ secretion |
| Counter-current Mechanism | Loop + Vasa recta | Medullary gradient → concentrated urine |
📦 Quick Recap
✔ Urine formation = Filtration + Reabsorption + Secretion
✔ GFR = 125 mL/min
✔ PCT → Maximum reabsorption
✔ Loop → Creates concentration gradient
✔ ADH → Water retention
✔ Aldosterone → Sodium retention
✔ Counter-current → Concentrated urine
Regulation of Kidney Function
🌱 Introduction
Kidneys maintain blood volume, water-salt balance, and pH by regulating filtration, reabsorption, and excretion. This regulation is controlled by hormones and neural signals.
The main regulators are:
- Renin-Angiotensin-Aldosterone system (RAAS)
- Atrial Natriuretic Factor (ANF)
- Antidiuretic Hormone (ADH)
- Disorders like Diabetes Insipidus
🔹 1. Renin-Angiotensin-Aldosterone System (RAAS)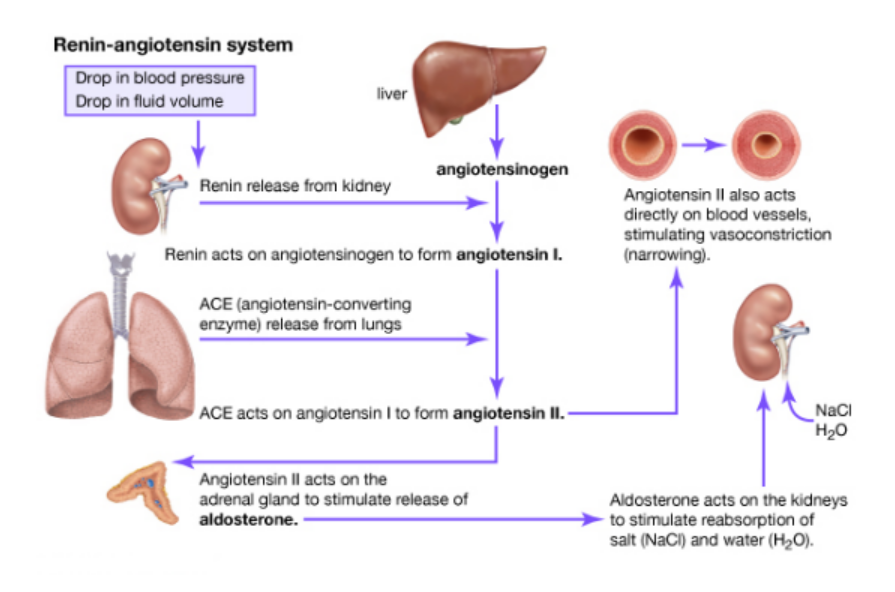
Purpose: Increase blood pressure and blood volume.
Steps:
- Juxtaglomerular Apparatus (JGA) detects low blood pressure / low sodium
- Juxtaglomerular cells release Renin
- Renin converts angiotensinogen (from liver) → angiotensin I
- Angiotensin I → Angiotensin II by ACE enzyme (lungs)
- Angiotensin II effects:
- Potent vasoconstrictor → raises blood pressure
- Stimulates adrenal cortex → releases aldosterone → increases Na+ & water reabsorption in distal tubules
- Blood volume & pressure rise → negative feedback stops renin release
Key points:
- RAAS works mainly when blood pressure is low
- Aldosterone indirectly increases water retention by retaining sodium
🔹 2. Atrial Natriuretic Factor (ANF)
Purpose: Lower blood pressure / reduce blood volume
Produced by: Atria of the heart when stretched due to high blood volume
Effects:
- Vasodilation → reduces blood pressure
- Inhibits renin release → suppresses RAAS
- Inhibits aldosterone → reduces Na+ reabsorption
- Increases Na+ & water excretion → more urine
Key concept: ANF works as negative feedback against RAAS
🔹 3. Antidiuretic Hormone (ADH / Vasopressin)
Produced by: Hypothalamus, stored & released by posterior pituitary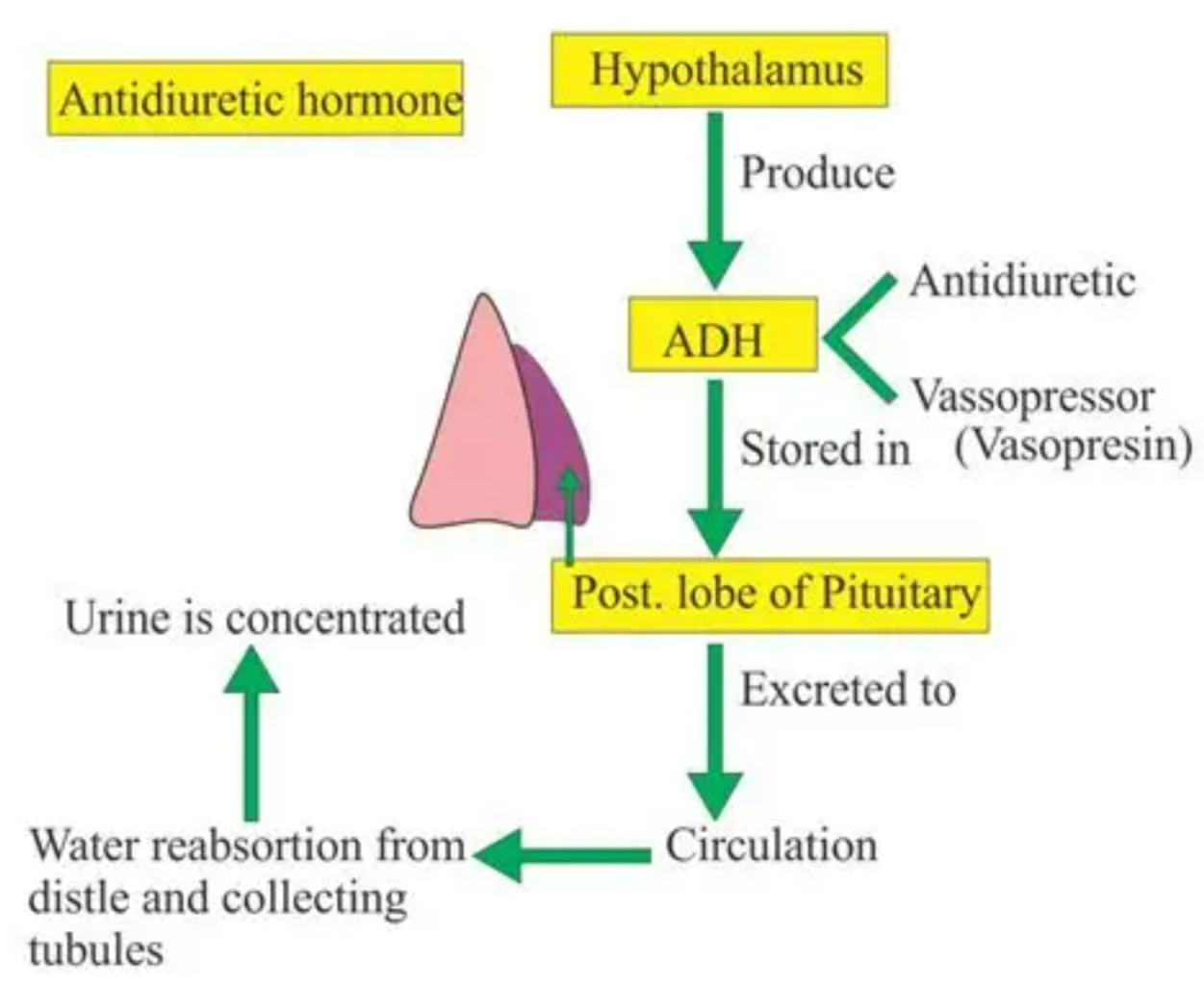
Stimulus for release:
- High blood osmolarity (dehydration)
- Low blood volume
Effects on kidney:
- Increases water permeability of collecting ducts → water reabsorbed → concentrated urine
- Low ADH → less water reabsorbed → dilute urine
Clinical relevance:
- Lack of ADH → Diabetes Insipidus (excessive urination, dehydration, low urine concentration)
🔹 4. Diabetes Insipidus (DI)
Definition: Disorder caused by deficient ADH or kidneys not responding to ADH
Symptoms:
- Polyuria (excessive urination)
- Polydipsia (excessive thirst)
- Dilute urine (low specific gravity)
- Dehydration risk
Types:
- Central DI – ADH deficiency (pituitary problem)
- Nephrogenic DI – Kidneys resistant to ADH
Treatment:
- Central DI → ADH analogs (Desmopressin)
- Nephrogenic DI → High water intake, thiazide diuretics
📊 Summary Table
| Regulator | Site of Action | Effect | Outcome |
|---|---|---|---|
| Renin-Angiotensin-Aldosterone | Kidney, blood vessels, adrenal cortex | Vasoconstriction + Na+ reabsorption | ↑ BP, ↑ Blood volume |
| ANF | Heart (atria) | Vasodilation + inhibits renin/aldosterone | ↓ BP, ↑ Na+ & water excretion |
| ADH | Collecting ducts | ↑ Water reabsorption | Concentrated urine, prevents dehydration |
| Diabetes Insipidus | ADH deficiency or renal resistance | ↓ Water reabsorption | Polyuria, dehydration, dilute urine |
📦 Quick Recap
✔ RAAS → raises BP & volume (Renin → Angiotensin II → Aldosterone)
✔ ANF → lowers BP & volume, opposite of RAAS
✔ ADH → controls water reabsorption in collecting ducts
✔ DI → ADH deficiency → polyuria & dehydration
Role of Other Organs in Excretion
🌱 Introduction
Excretion is the removal of metabolic waste products from the body. While kidneys are the primary excretory organs, other organs also help remove wastes in specific forms. These organs ensure detoxification, osmoregulation, and maintaining homeostasis.
1. Skin
Structure & Function:
- Skin is a multilayered organ with sweat glands (eccrine and apocrine)
- Sweat glands help in excretion of water, salts (Na⁺, K⁺, Cl⁻), urea, and lactic acid
- Sweat helps in thermoregulation and removal of nitrogenous wastes
Key Points:
- 1 liter of sweat may contain ~1 g urea/day
- Excretion through skin is minor but continuous
- Sweat also removes excess electrolytes and helps maintain osmotic balance
2. Lungs
Function in Excretion:
- Lungs excrete carbon dioxide (CO₂) and water vapor
- CO₂ is a major metabolic waste produced during cellular respiration
- Excretion occurs via alveolar gas exchange
Mechanism:
- CO₂ diffuses from blood (high pCO₂) → alveoli (low pCO₂)
- Expired air removes CO₂ from the body
- Water vapor is lost during respiration, contributing to insensible water loss
Key Points:
- ~200 ml water/day lost via lungs
- Vital for maintaining acid-base balance (CO₂ + H₂O ↔ H₂CO₃ ↔ H⁺ + HCO₃⁻)
3. Liver
Function in Excretion:
- Liver is a detoxification organ, not a direct excretory organ, but plays a major role:
Conversion of toxic substances:
- Ammonia → Urea (via Urea Cycle) → excreted by kidneys
- Bilirubin formation from breakdown of hemoglobin → excreted in bile
Drug metabolism:
- Liver modifies drugs, alcohol, and toxins → water-soluble forms → excreted via kidneys or bile
Bile excretion:
- Bile contains bilirubin, bile salts, cholesterol, and heavy metals
- Excreted into small intestine → feces
Key Points:
- Liver prevents ammonia toxicity
- Bilirubin excretion prevents jaundice
4. Intestine
Function in Excretion:
- Large intestine excretes undigested food, bile pigments (bilirubin derivatives), and water
- Bile pigments give color to feces
- Some nitrogenous wastes like creatinine are also eliminated in feces
Key Points:
- Feces contain ~30% dead cells and microbial biomass
- Works in conjunction with liver for bile-based excretion
5. Other Minor Excretory Organs
| Organ | Waste Removed | Notes |
|---|---|---|
| Salivary glands | Excess ions, some drugs | Minor role |
| Mammary glands | Water, salts, urea, milk lipids | Excretion in lactation |
| Lymphatic system | Metabolic wastes, dead cells | Indirect excretion; drains into blood |
📦 Quick Recap
✔ Skin: Sweat → water, salts, urea
✔ Lungs: CO₂, water vapor → maintains pH & removes respiratory wastes
✔ Liver: Detoxifies ammonia → urea, bile pigments, drugs → fecal & urinary excretion
✔ Intestine: Feces → undigested material + bilirubin
✔ Others: Minor role in ions, drugs, lactation wastes
Disorders of Human Excretory System
🌱 Introduction
Disorders of the excretory system occur when kidneys or urinary tract fail to remove wastes and excess water, leading to accumulation of toxic substances like urea, creatinine, and uric acid.
1. Uraemia
Definition:
- Accumulation of urea and other nitrogenous wastes in blood due to impaired kidney function
Causes:
- Chronic kidney disease
- Glomerulonephritis
- Obstruction in urinary tract
Symptoms:
- Fatigue, weakness
- Nausea and vomiting
- Swelling in ankles and around eyes
- Breath may have urine-like odor
Treatment:
- Dialysis (temporary removal of waste)
- Kidney transplant in severe cases
- Restriction of protein in diet
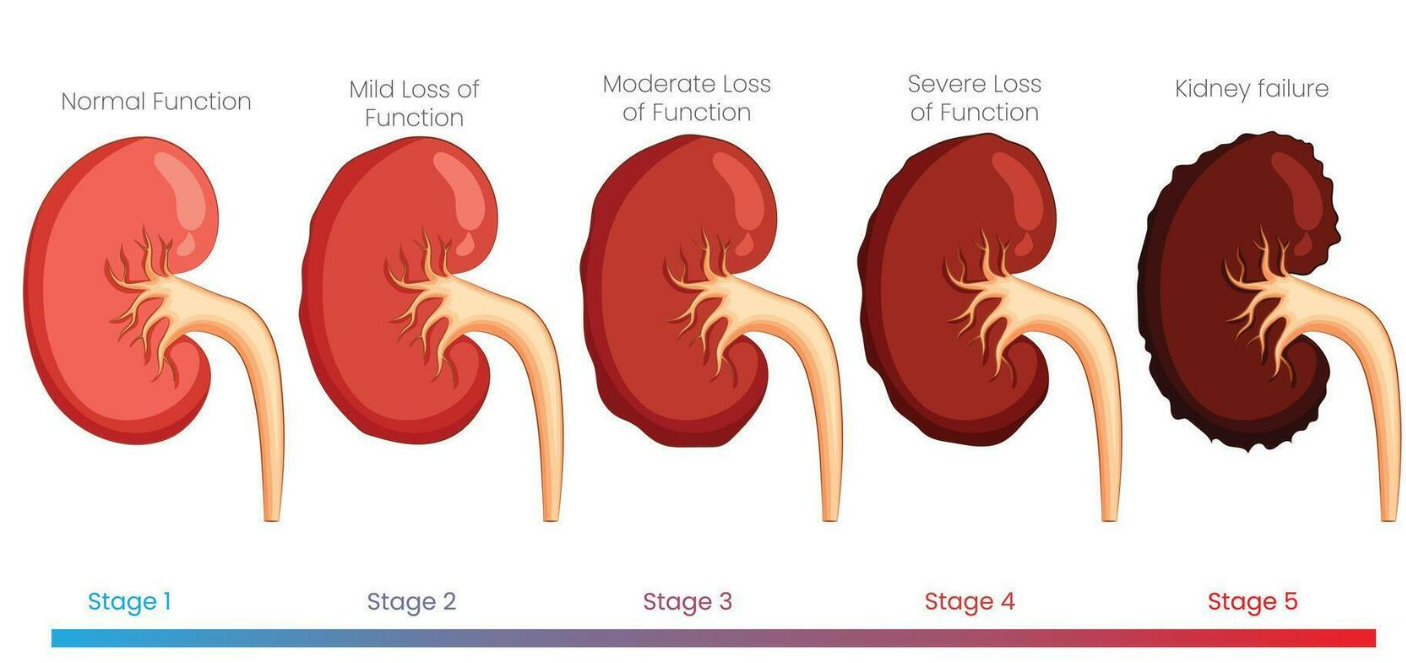
2. Renal Failure
Definition:
- Condition where kidneys lose the ability to filter blood properly, leading to accumulation of toxins
Types:
- Acute Renal Failure (ARF): Sudden loss of kidney function, reversible

- Chronic Renal Failure (CRF): Gradual loss over months/years, often irreversible
Causes:
- Severe infection
- Low blood flow to kidneys
- Long-term diabetes or hypertension
Symptoms:
- Reduced urine output (oliguria)
- Fluid retention → swelling
- High blood pressure
- Weakness, nausea, confusion
Treatment:
- Dialysis to remove toxins
- Kidney transplant for CRF
- Medications to manage symptoms
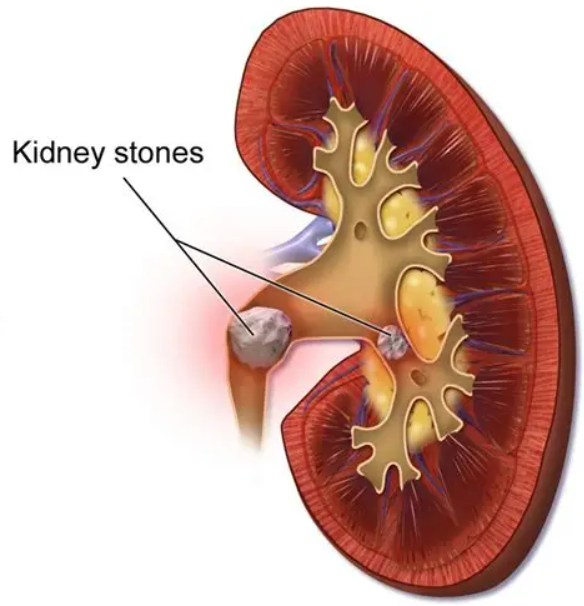
3. Renal Calculi (Kidney Stones)
Definition:
- Hard deposits formed from crystals of calcium, oxalate, or uric acid in kidneys or urinary tract

Causes:
- High calcium or oxalate intake
- Dehydration → concentrated urine
- High purine diet → uric acid stones
- Genetic factors
Symptoms:
- Severe lower back or abdominal pain (renal colic)
- Blood in urine (hematuria)
- Nausea and vomiting
Treatment:
- High water intake to flush stones
- Medications to dissolve stones
- Lithotripsy (shock-wave to break stones)
- Surgical removal if large
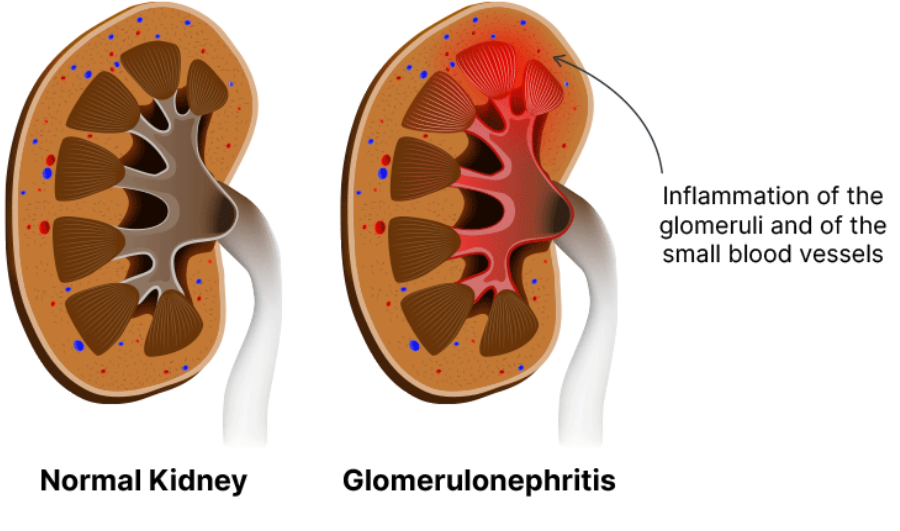
🔹 4. Nephritis
Definition:
- Inflammation of kidneys, affecting glomeruli or tubules
Causes:
- Infection (bacterial or viral)
- Autoimmune disorders (e.g., lupus)

- Post-streptococcal infection
Symptoms:
- Swelling (edema), especially in face and ankles
- Blood in urine (hematuria)
- Reduced urine output
- High blood pressure
Treatment:
- Antibiotics for infection
- Anti-inflammatory drugs
- Dietary restrictions (salt, protein)
- Dialysis in severe cases
📦 Quick Recap
✔ Uraemia: Waste accumulation → fatigue, nausea; treat with dialysis/kidney transplant
✔ Renal Failure: Loss of kidney function → oliguria, edema; dialysis/transplant
✔ Renal Calculi: Crystals in kidneys → severe pain, hematuria; treat with hydration, lithotripsy
✔ Nephritis: Kidney inflammation → swelling, hematuria, high BP; treat with antibiotics & anti-inflammatories
Dialysis and Artificial Kidney
🌱 Introduction
When kidneys fail to remove waste products, excess salts, and water, dialysis is used as a life-saving procedure. It mimics the filtering function of kidneys. The machine used is called an artificial kidney.
🧪 1. Dialysis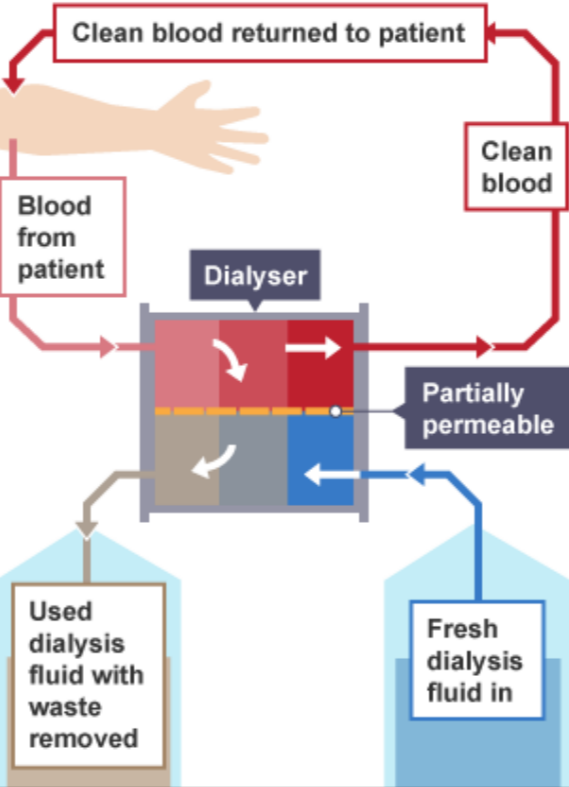
Definition:
- A medical process to remove nitrogenous wastes, extra salts, and water from blood when kidneys fail
Types of Dialysis:
| Type | How it Works | Key Points |
|---|---|---|
| Hemodialysis | Blood is pumped into a dialyzer (artificial kidney). Wastes diffuse into dialysate, and clean blood returns to body. | Usually 3–4 hours/session, 3 times a week |
| Peritoneal Dialysis | Uses the peritoneal membrane in abdomen as a natural filter. Dialysate absorbs wastes & water, then is drained. | Can be done at home, continuous or intermittent |
Advantages:
- Removes urea, creatinine, and excess water
- Maintains electrolyte balance
- Helps control blood pressure
Limitations:
- Temporary solution, not permanent
- Risk of infection (especially peritoneal)
- Expensive and time-consuming
🧬 2. Artificial Kidney
Definition:
- A machine that performs hemodialysis, acting as an external kidney
Components: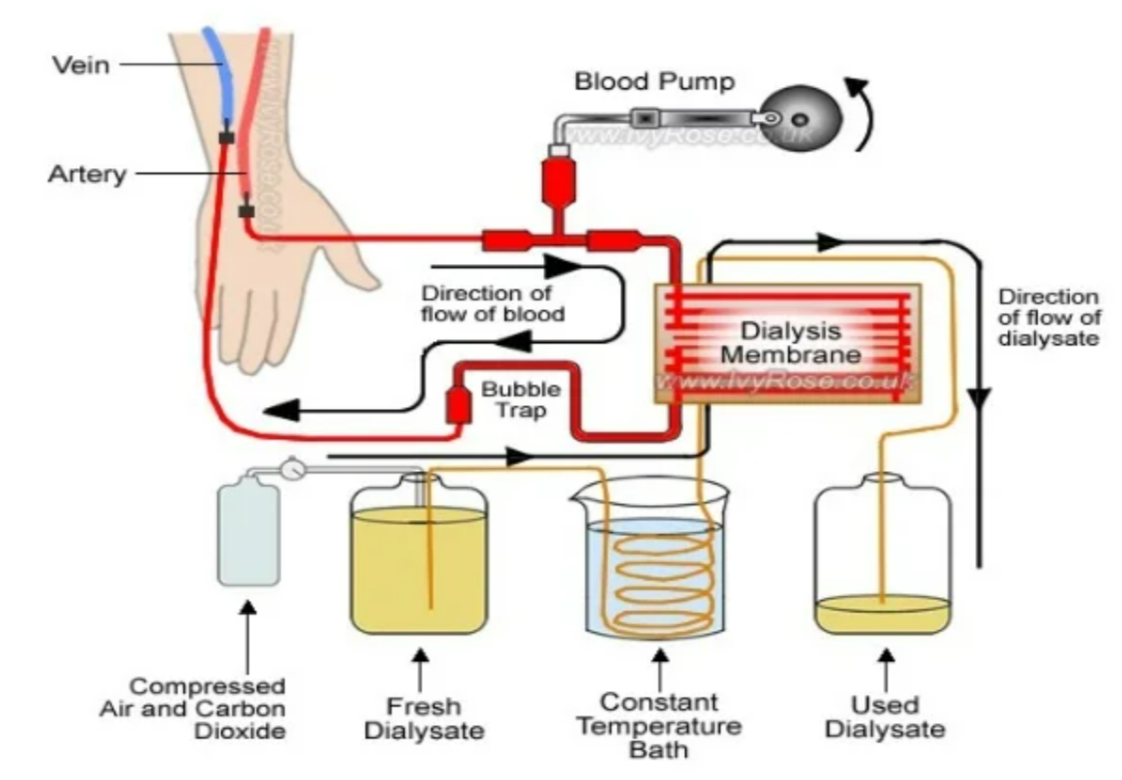
- Blood compartment – for patient’s blood
- Dialysate compartment – absorbs wastes
- Semipermeable membrane – separates blood & dialysate
- Pump & sensors – maintain blood flow & pressure
Working Principle:
- Wastes like urea, creatinine, potassium diffuse from blood → dialysate
- Excess water removed by ultrafiltration
- Clean blood is returned to the body
Use:
- For chronic kidney disease (CKD) patients
- Acts as a temporary support before kidney transplant
📦 Quick Recap
✔ Dialysis: Cleans blood when kidneys fail
✔ Hemodialysis: Blood pumped through artificial kidney
✔ Peritoneal Dialysis: Uses peritoneal membrane as filter
✔ Artificial Kidney: Machine that removes wastes and excess water
✔ Limitation: Temporary; kidney transplant is permanent solution