NEET Biology - Unit 5- Locomotion and Movement- Study Notes - New Syllabus
NEET Biology – Unit 5- Locomotion and Movement- Study Notes – New Syllabus
Key Concepts:
- Locomotion and Movement: Types of movement- ciliary, fiagellar, muscular; Skeletal muscle- contractile proteins and muscle contraction; Skeletal system and its functions (To be dealt with the relevant practical of Practical syllabus); Joints; Disorders of muscular and skeletal system-Myasthenia gravis, Tetany, Muscular dystrophy, Arthritis, Osteoporosis, Gout.
Locomotion and Movement
🌱 Introduction
Movement is a fundamental feature of living organisms.
- Locomotion → movement that results in change of position or location.
- Examples: walking, running, climbing.
🧬 Types of Movement
| Type | How it Occurs | Examples / Function |
|---|---|---|
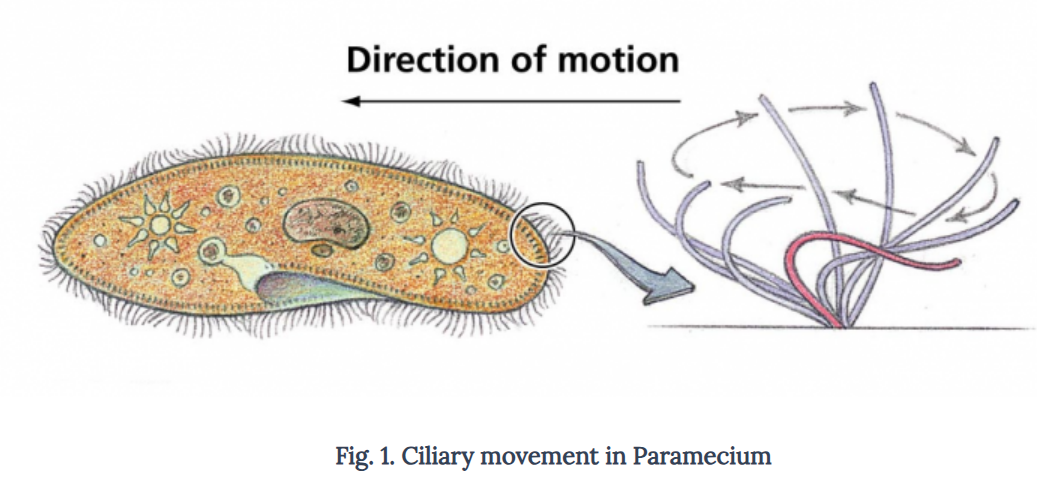
| Ciliary Movement | Movement of cilia present on cell surfaces or internal tubular organs. | Moves dust in respiratory tract, moves ova in fallopian tube, locomotion in Paramecium. |
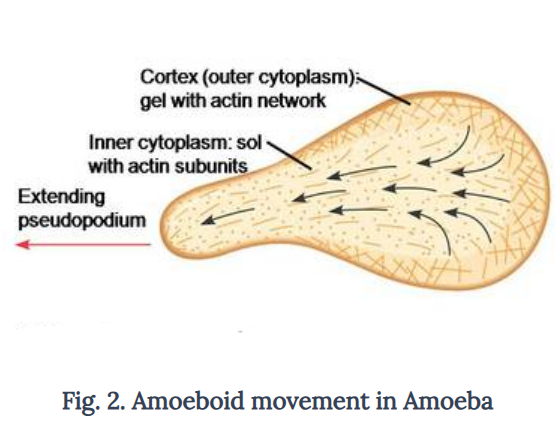
| Amoeboid Movement | Movement by extending pseudopodia (false feet). | Observed in Amoeba and immune cells like macrophages, leukocytes. |
| Muscular Movement | Movement of body parts by muscles. Involves muscle + skeletal + neural system. | Tongue, jaws, limbs; walking, running, posture maintenance. |
💪 Muscle – The Tissue of Movement
- Origin: Mesodermal tissue
- Function: Produces movement by contraction
Types of Muscle:
| Type | Appearance | Control | Location / Function |
|---|---|---|---|
| Skeletal / Striated | Cross-striated | Voluntary | Attached to bones via tendons; locomotion & posture |
| Smooth / Visceral | Non-striated | Involuntary | Walls of alimentary canal, reproductive tract, blood vessels |
| Cardiac | Striated, branched | Involuntary | Heart wall; rhythmic contraction |
🧬 Structure of Skeletal Muscle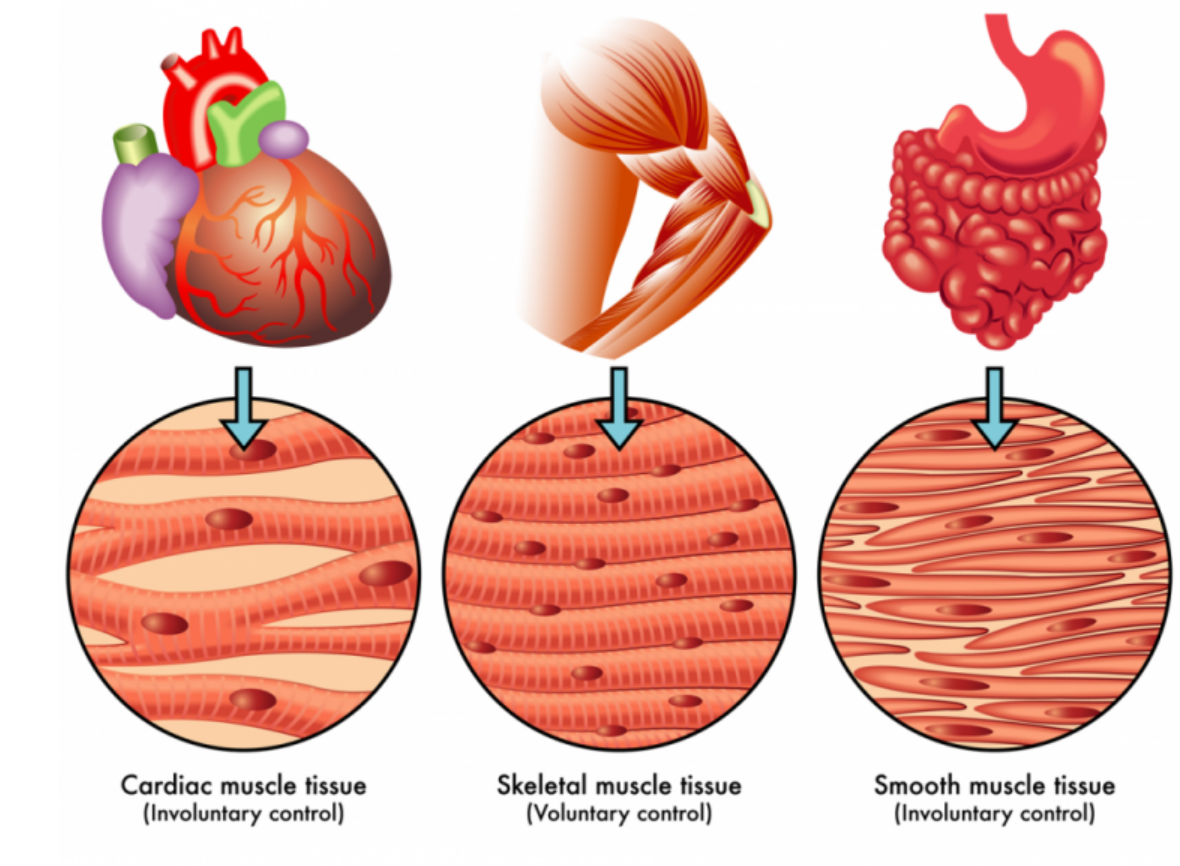
- Muscle → Fascicles (bundles) → Muscle fibers
- Muscle Fiber: Multi-nucleated syncytium, surrounded by sarcolemma
- Sarcoplasm: Cytoplasm of muscle fiber
- Sarcoplasmic Reticulum: Stores Ca²⁺ ions for contraction
- Myofibrils / Myofilaments: Parallel filaments → actin (thin) & myosin (thick)
Sarcomere – Functional Unit
- Segment between two Z-lines
- Light bands (I-bands) → actin
- Dark bands (A-bands) → myosin
- Sliding of actin over myosin → muscle contraction
🔬 Structure of Contractile Proteins
| Protein | Structure | Function |
|---|---|---|
| Actin | Monomer: G-actin → polymer: F-actin, with tropomyosin & troponin | Forms thin filament; binds myosin |
| Myosin | Globular head (ATPase activity) + long tail | Thick filament; binds actin to form cross-bridges |
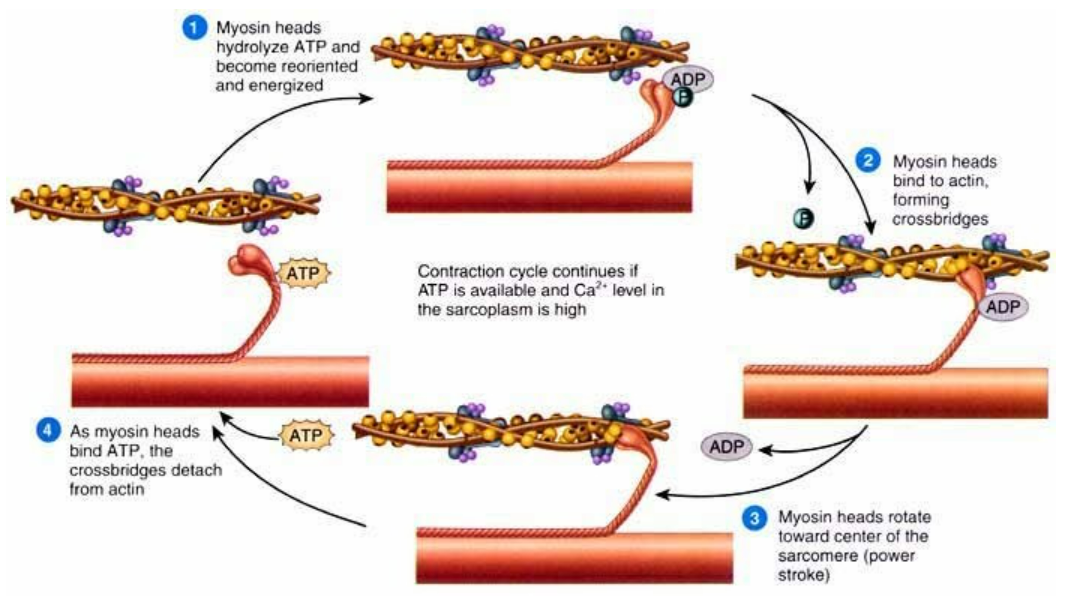
⚡ Mechanism of Muscle Contraction
- Sliding Filament Theory
- Motor neuron releases acetylcholine at neuromuscular junction
- Action potential → Ca²⁺ release from sarcoplasmic reticulum
- Ca²⁺ binds troponin → exposes actin binding sites
- Myosin heads attach → cross-bridge formation
- ATP hydrolysis → sliding of actin → sarcomere shortens → contraction
- Relaxation → Ca²⁺ pumped back → actin sites covered
Lactic Acid Formation
- Occurs during anaerobic muscle activity
- Example: Running, lifting weights
- Glycogen → lactic acid → muscle fatigue
🦴 Skeletal System – Framework for Locomotion
- Bones: Hard due to calcium salts
- Cartilage: Flexible due to chondroitin sulfate
- Total bones in humans: 206
Divisions
| Division | Bones | Function |
|---|---|---|
| Axial Skeleton (80) | Skull, vertebral column, sternum, ribs | Supports body, protects brain & organs |
| Appendicular Skeleton (126) | Limbs & girdles | Movement of limbs |
✅ Quick Recap
✔ Locomotion: Movement causing change in location
✔ Ciliary: Paramecium, ova movement
✔ Amoeboid: Pseudopodia, immune cells
✔ Muscular: Muscles + skeleton + nerves → voluntary & involuntary movement
✔ Skeletal muscle: Sarcomere = functional unit; actin + myosin
✔ Contraction: Sliding filament theory → ATP + Ca²⁺
✔ Skeleton: Axial = support & protection; Appendicular = limb movement
Skeletal Muscle: Contractile Proteins & Muscle Contraction
🌱 1. Skeletal Muscle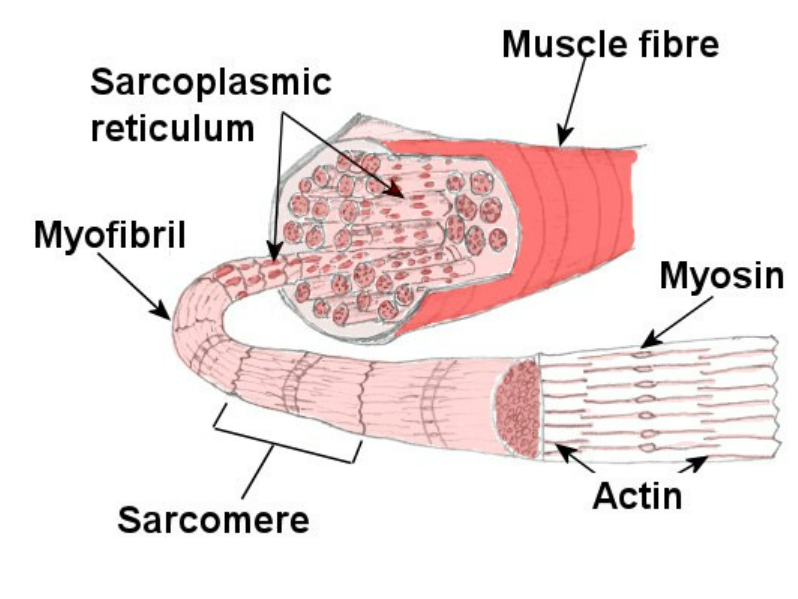
- Type: Striated, voluntary muscle
- Attached to bones via tendons
- Function: Locomotion, posture, voluntary movements
- Structure: Muscle → Fascicles → Muscle fibers → Myofibrils → Sarcomeres
🧬 2. Contractile Proteins in Skeletal Muscle
| Protein | Structure | Location | Function |
|---|---|---|---|
| Actin (Thin filament) | Monomer: G-actin → Polymer: F-actin; associated with tropomyosin and troponin | I-band | Forms thin filaments; binds myosin for contraction |
| Tropomyosin | Fibrous protein | Along F-actin | Covers myosin binding sites on actin at rest |
| Troponin | Complex of 3 subunits: TnT, TnI, TnC | On actin filament | Regulates actin-myosin interaction; binds Ca²⁺ |
| Myosin (Thick filament) | Composed of meromyosins (head + tail); head has ATPase activity | A-band | Forms thick filaments; head binds actin & hydrolyzes ATP to produce contraction |
🧬 3. Structure of Sarcomere
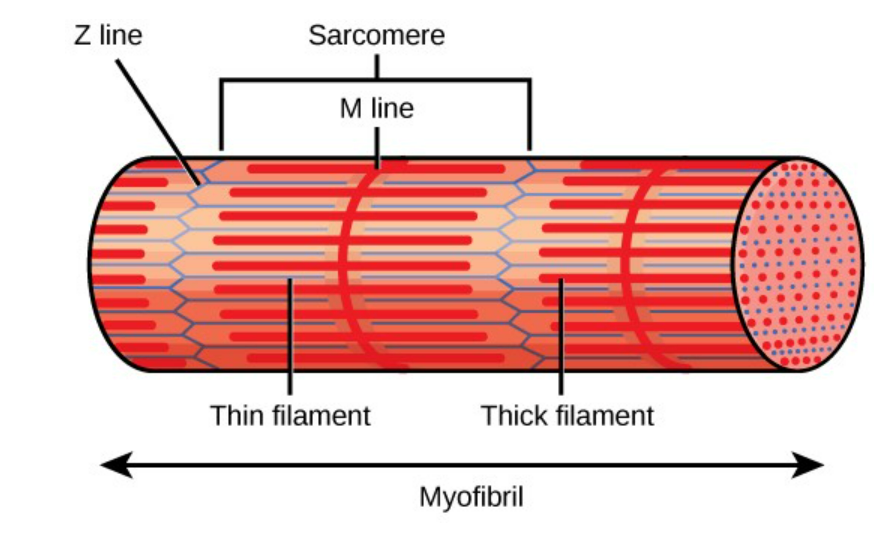
- Functional unit of skeletal muscle
- Bounded by Z-lines
- Bands:
- I-band: Light, actin only
- A-band: Dark, myosin (with some overlap with actin)
- H-zone: Central part of A-band, only myosin
- M-line: Middle of H-zone, anchors myosin
⚡ 4. Mechanism of Muscle Contraction
- Sliding Filament Theory
 Impulse Generation: Motor neuron releases acetylcholine (ACh) at neuromuscular junction
Impulse Generation: Motor neuron releases acetylcholine (ACh) at neuromuscular junction- Action Potential: Travels along sarcolemma → T-tubules → sarcoplasm
- Calcium Release: Sarcoplasmic reticulum releases Ca²⁺ ions
- Troponin Activation: Ca²⁺ binds troponin → tropomyosin moves → exposes myosin-binding sites on actin
- Cross-Bridge Formation: Myosin head attaches to actin → forms cross-bridge
- Power Stroke: Myosin head bends, pulls actin → sarcomere shortens
- ATP Role:
- ATP binds myosin head → detaches from actin
- ATP hydrolysis → re-cocks myosin head
- Relaxation: Ca²⁺ pumped back into SR → troponin-tropomyosin complex covers actin → sarcomere returns to original length
📝 5. Important Points
- All-or-None Law: Single muscle fiber contracts fully or not at all
- Recruitment: Stronger contraction → more fibers activated
- Energy Source: ATP (from aerobic/anaerobic respiration)
- Lactic Acid Formation: Anaerobic activity → lactic acid → muscle fatigue
✅ Quick Recap
✔ Contractile proteins: Actin (thin), Myosin (thick)
✔ Regulatory proteins: Troponin, Tropomyosin
✔ Sarcomere: Z-line → functional unit
✔ Cross-bridge cycle: Ca²⁺ + ATP → actin-myosin interaction → contraction
✔ Relaxation: Ca²⁺ pumped back, tropomyosin covers actin
Skeletal System & Its Functions
📌 Introduction
Skeletal system = framework of body made of bones + cartilages.
Functions:
- Supports body shape & posture
- Protects vital organs (brain, heart, lungs)
- Aids movement by acting as levers for muscles
- Produces blood cells (RBCs & WBCs) in bone marrow
- Stores minerals (Ca²⁺, PO₄³⁻) & energy (lipids in yellow marrow)
Humans have 206 bones + some cartilages.
Bone → hard (Ca₃(PO₄)₂ + CaCO₃), Cartilage → flexible (chondroitin sulfate)
1. Components of Skeletal System
A. Bones
- Rigid, mineralized connective tissue
- Functions: Support, protection, movement, hematopoiesis, mineral & energy storage
B. Cartilage
- Flexible connective tissue
- Functions: Smooth surfaces at joints, flexibility, prevent friction
2. Divisions of Human Skeleton
| Division | Bones | Function / Notes |
|---|---|---|
| Axial Skeleton | Skull, Vertebral column, Ribs, Sternum (80 bones) | Supports head, neck, trunk; protects brain, heart, lungs |
| Appendicular Skeleton | Limbs + Girdles (Pectoral & Pelvic) (126 bones) | Movement, muscle attachment, locomotion |
3. Axial Skeleton (80 bones)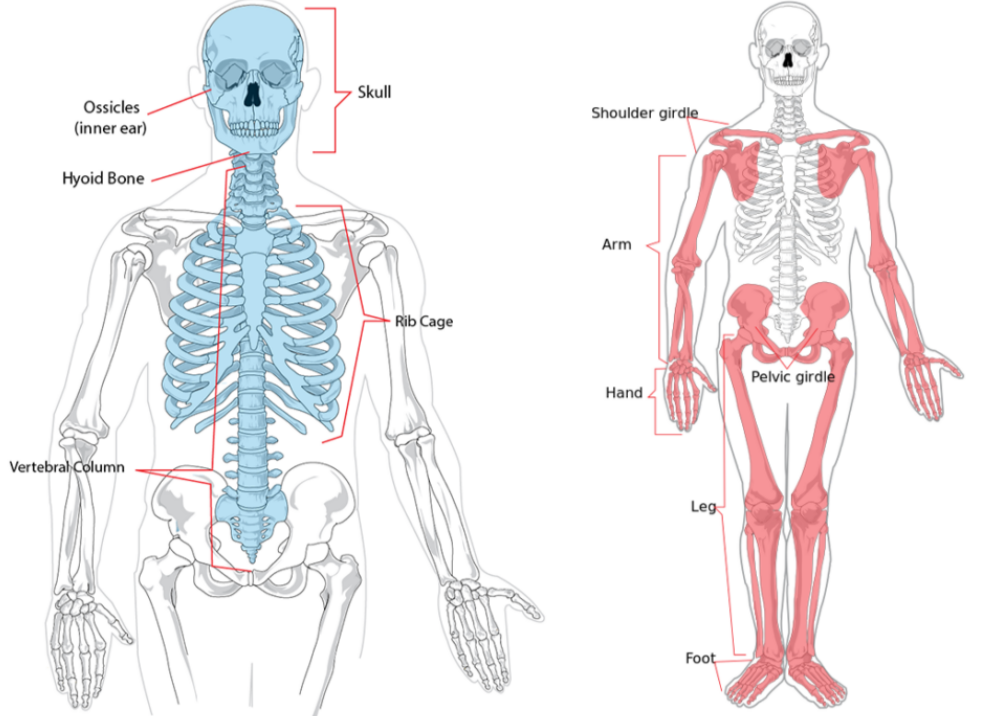
- Skull (22 bones)
- Cranial (8) → protects brain
- Facial (14) → forms front, supports jaw & face
- Hyoid → U-shaped, supports tongue
- Ear ossicles: Malleus, Incus, Stapes → transmit sound
- Vertebral Column (26 bones)
- Protects spinal cord, forms trunk framework
- Regions: Cervical 7 (Atlas, Axis), Thoracic 12, Lumbar 5, Sacral 1 (fused), Coccygeal 1
- Sternum → Flat bone on ventral midline of thorax
- Ribs (12 pairs)
- True ribs 1–7 → attached to sternum
- False ribs 8–10 → indirect attachment
- Floating ribs 11–12 → not attached
- Rib cage = thoracic vertebrae + ribs + sternum → protection + respiration
4. Appendicular Skeleton
- Pectoral Girdle: Clavicle + Scapula → Glenoid cavity forms ball & socket joint with humerus → shoulder movement
- Pelvic Girdle: Ilium + Ischium + Pubis → Acetabulum forms ball & socket joint with femur → supports weight & movement
- Forelimbs (30 bones each): Humerus, Radius + Ulna, Carpals 8, Metacarpals 5, Phalanges 14
- Hindlimbs (30 bones each): Femur, Tibia + Fibula, Tarsals 7, Metatarsals 5, Phalanges 14, Patella (knee cap)
5. Types of Joints
| Type | Structure | Example | Movement |
|---|---|---|---|
| Fibrous | Bones joined by fibrous tissue | Skull sutures | Immovable |
| Cartilaginous | Bones joined by cartilage | Vertebrae | Slightly movable |
| Synovial | Fluid-filled capsule | Knee, Shoulder | Freely movable |
Synovial Joints: Ball & Socket → Shoulder/Hip, Hinge → Elbow/Knee, Pivot → Atlas-Axis, Gliding → Carpals/Tarsals
6. Functions of Skeletal System
- Support → Maintains shape & posture
- Protection → Brain, heart, lungs, spinal cord
- Movement → Bones act as levers for muscles
- Hematopoiesis → RBC & WBC formation in marrow
- Mineral storage → Calcium & phosphorus
- Energy storage → Lipids in yellow marrow
✅ Quick Recap
Skeletal System = Bones + Cartilage
Axial Skeleton (80) → Skull, Vertebrae, Ribs, Sternum → support & protection
Appendicular Skeleton (126) → Limbs + Girdles → movement & muscle attachment
Bone Functions → Support, Protection, Movement, Hematopoiesis, Mineral & Energy storage
Joints → Fibrous (immobile), Cartilaginous (slightly movable), Synovial (freely movable: ball & socket, hinge, pivot, gliding)
Joints (Articulations)
🌱 1. What are Joints?
- Points of connection between two or more bones
- Function: Allow movement, provide stability, and absorb shock
🧬 2. Classification of Joints
| Type | Structure / Features | Movement | Example |
|---|---|---|---|
| Fibrous (Immovable / Synarthrosis) | Bones connected by fibrous connective tissue, no joint cavity | No movement | Skull sutures, Tooth in jaw (gomphosis) |
| Cartilaginous (Slightly Movable / Amphiarthrosis) | Bones joined by cartilage, no joint cavity | Slight movement | Vertebrae (intervertebral discs), Pubic symphysis |
| Synovial (Freely Movable / Diarthrosis) | Bones enclosed in joint capsule filled with synovial fluid | Free movement | Shoulder, Knee, Hip |
🌸 3. Structure of Synovial Joint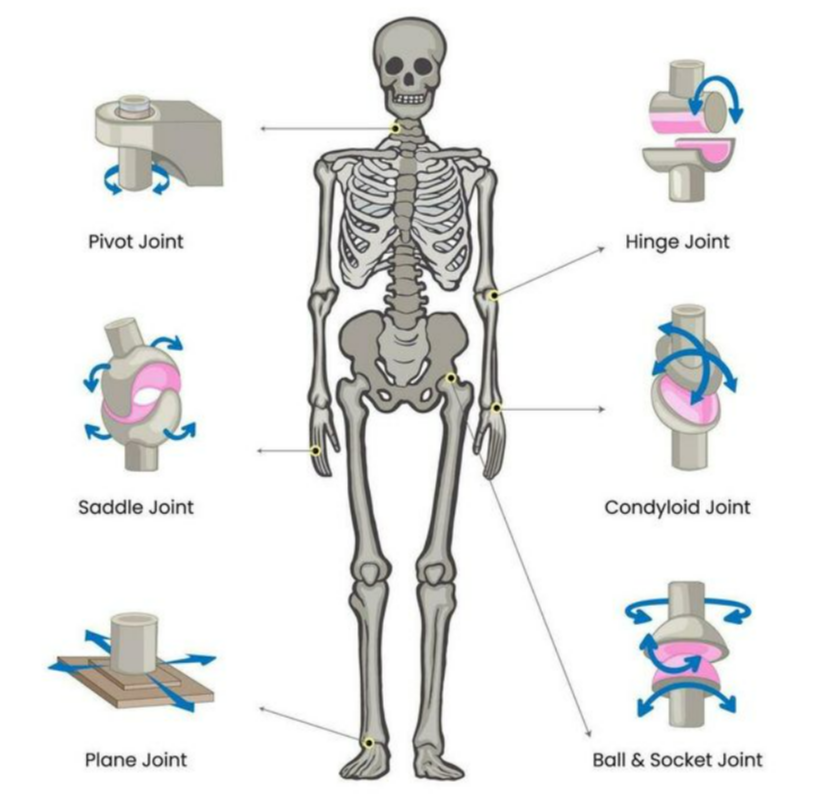
- Articular cartilage: Covers bone ends → reduces friction
- Synovial membrane: Secretes synovial fluid for lubrication
- Joint capsule: Tough fibrous tissue → encloses joint
- Ligaments: Connect bone to bone → provide stability
- Bursa: Fluid-filled sac → reduces friction
- Meniscus (optional): Fibrocartilage → cushions & distributes weight
🧬 4. Types of Synovial Joints & Movements
| Joint Type | Movement | Example |
|---|---|---|
| Hinge | Flexion & Extension | Elbow, Knee, Phalanges |
| Ball & Socket | Flexion, Extension, Rotation, Abduction, Adduction | Shoulder, Hip |
| Pivot | Rotation around a central axis | Atlas-Axis (neck) |
| Saddle | Flexion, Extension, Abduction, Adduction | Base of thumb |
| Gliding / Plane | Sliding / Gliding | Carpals, Tarsals |
| Condyloid / Ellipsoid | Flexion, Extension, Adduction, Abduction | Wrist joint |
🧬 5. Functions of Joints
- Movement: Allow bones to move efficiently
- Support: Maintain posture and body alignment
- Shock Absorption: Cushion bones from impact
- Flexibility: Enable various complex movements
✅ Quick Recap
✔ Joints = Points of bone connection
✔ Types: Fibrous (immovable), Cartilaginous (slightly movable), Synovial (freely movable)
✔ Synovial Features: Articular cartilage, synovial membrane, ligaments, bursae, meniscus
✔ Synovial Movements: Hinge (elbow), Ball & Socket (shoulder), Pivot (atlas-axis), Saddle (thumb), Gliding (carpals), Condyloid (wrist)
Disorders of Muscular and Skeletal System
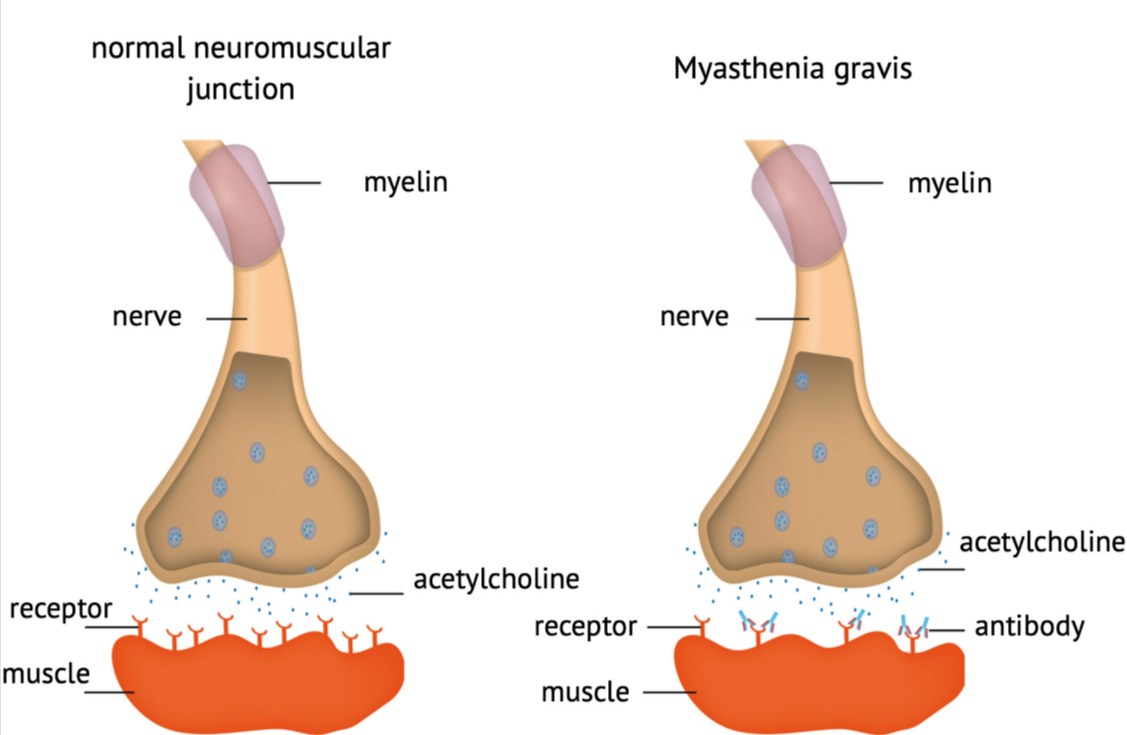
1. Myasthenia Gravis
- Type: Neuromuscular disorder

- Cause: Autoimmune disease → antibodies block acetylcholine receptors at neuromuscular junction
- Effect: Weakness of voluntary muscles, especially eyes, face, and throat
- Symptoms: Drooping eyelids, difficulty in swallowing, fatigue after activity
- Treatment: Acetylcholinesterase inhibitors, immunosuppressants
2. Tetany
- Type: Muscle disorder
- Cause: Low blood calcium levels (hypocalcemia) or low magnesium
- Effect: Continuous, involuntary muscle contractions
- Symptoms: Muscle cramps, spasms of hands and feet (carpopedal spasm), tingling sensation
- Treatment: Calcium and magnesium supplements
3. Muscular Dystrophy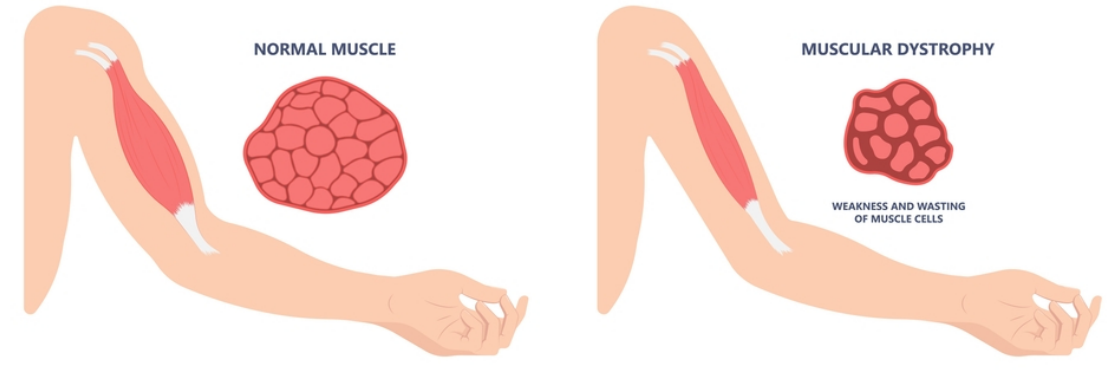
- Type: Genetic disorder affecting muscles
- Cause: Mutation in dystrophin gene → essential for muscle fiber stability
- Effect: Progressive muscle weakness and degeneration
- Symptoms: Difficulty in walking, frequent falls, respiratory issues in severe cases
- Common Type: Duchenne Muscular Dystrophy (DMD) – X-linked
- Treatment: Physiotherapy, corticosteroids, gene therapy (experimental)
4. Arthritis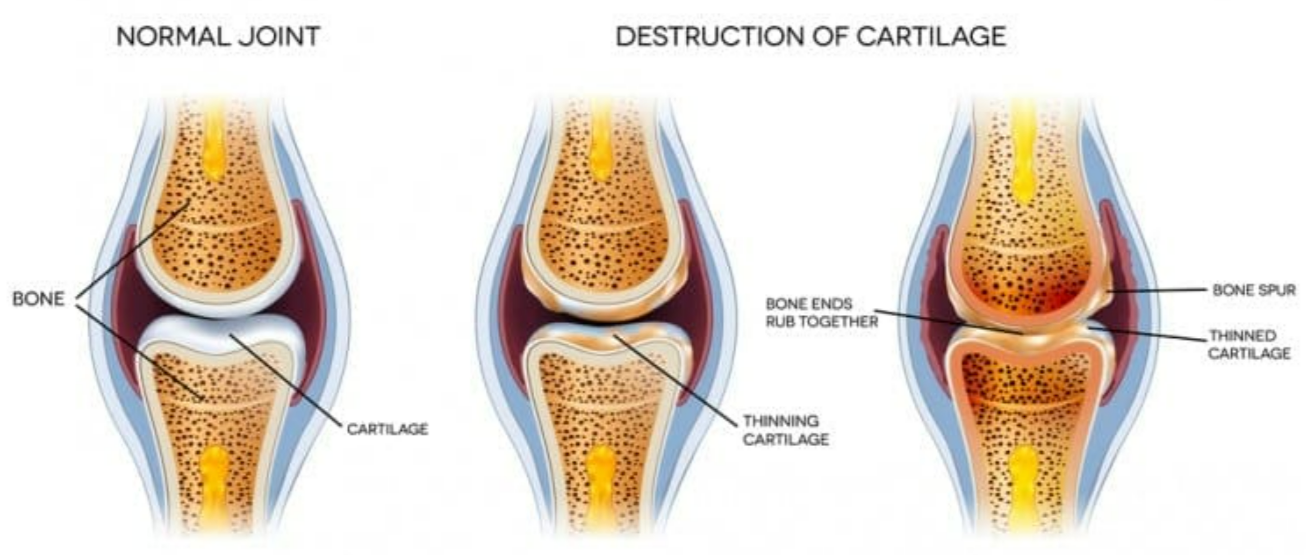
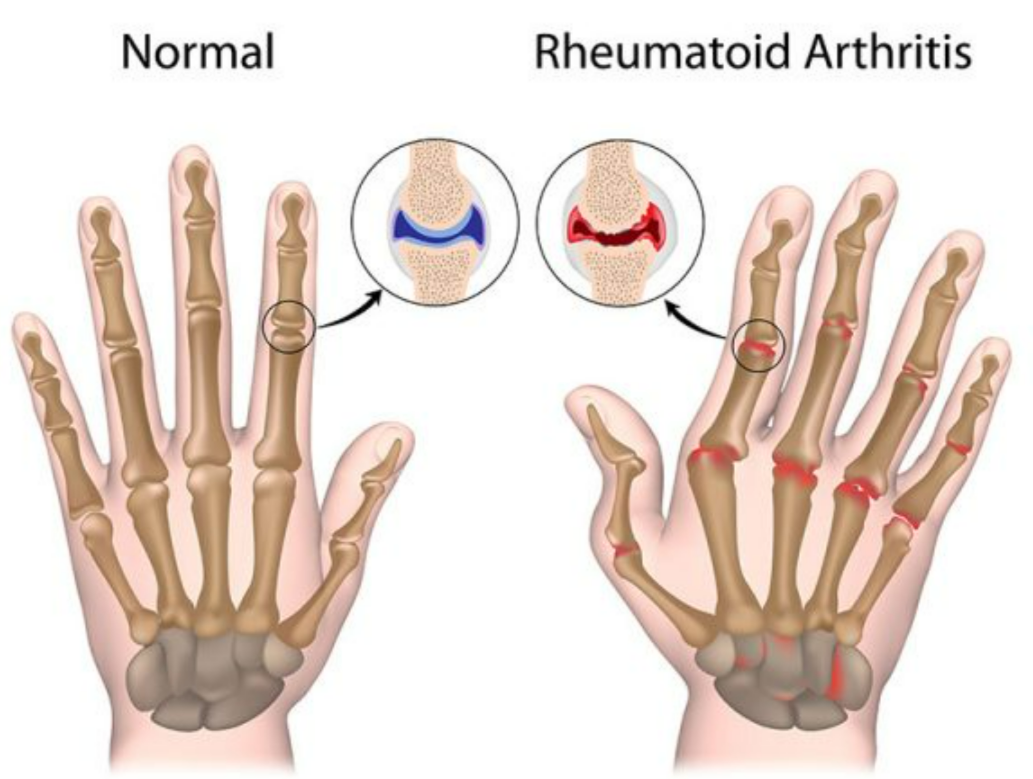
- Type: Inflammatory disorder of joints
- Causes & Types:
- Osteoarthritis: Wear and tear of cartilage
- Rheumatoid arthritis: Autoimmune attack on synovial membrane
- Symptoms: Joint pain, swelling, stiffness, reduced mobility
- Treatment: Painkillers, anti-inflammatory drugs, physiotherapy, joint replacement (severe)
5. Osteoporosis
- Type: Metabolic bone disease
- Cause: Low bone mineral density, often due to calcium or vitamin D deficiency
- Effect: Fragile bones → higher fracture risk
- Symptoms: Back pain, height reduction, bone fractures easily
- Treatment: Calcium & vitamin D supplementation, weight-bearing exercises, medications like bisphosphonates
6. Gout
- Type: Metabolic disorder
- Cause: High uric acid in blood → deposition of urate crystals in joints
- Effect: Inflammation, mainly in big toe (podagra)
- Symptoms: Severe pain, redness, swelling, and warmth in joints
- Treatment: Low purine diet, allopurinol (reduces uric acid), anti-inflammatory drugs
📊 Quick Recap
| Disorder | System Affected | Cause | Key Symptom |
|---|---|---|---|
| Myasthenia Gravis | Muscular | Autoimmune, blocks Ach receptors | Muscle weakness, drooping eyelids |
| Tetany | Muscular | Hypocalcemia | Muscle spasms, cramps |
| Muscular Dystrophy | Muscular | Genetic, dystrophin mutation | Progressive muscle weakness |
| Arthritis | Skeletal / Joints | Wear & tear or autoimmune | Joint pain, swelling |
| Osteoporosis | Skeletal | Low bone density | Fragile bones, fractures |
| Gout | Skeletal / Joints | High uric acid | Joint inflammation, especially big toe |