NEET Biology - Unit 6- Human Reproduction- Study Notes - New Syllabus
NEET Biology – Unit 6- Human Reproduction- Study Notes – New Syllabus
Key Concepts:
- Human Reproduction: Male and female reproductive systems; Microscopic anatomy of testis and ovary; Gametogenesis-spermatogenesis & oogenesis; Menstrual cycle; Fertilisation, embryo development upto blastocyst formation, implantation; Pregnancy and placenta formation (Elementary idea); Parturition (Elementary idea); Lactation (Elementary idea)
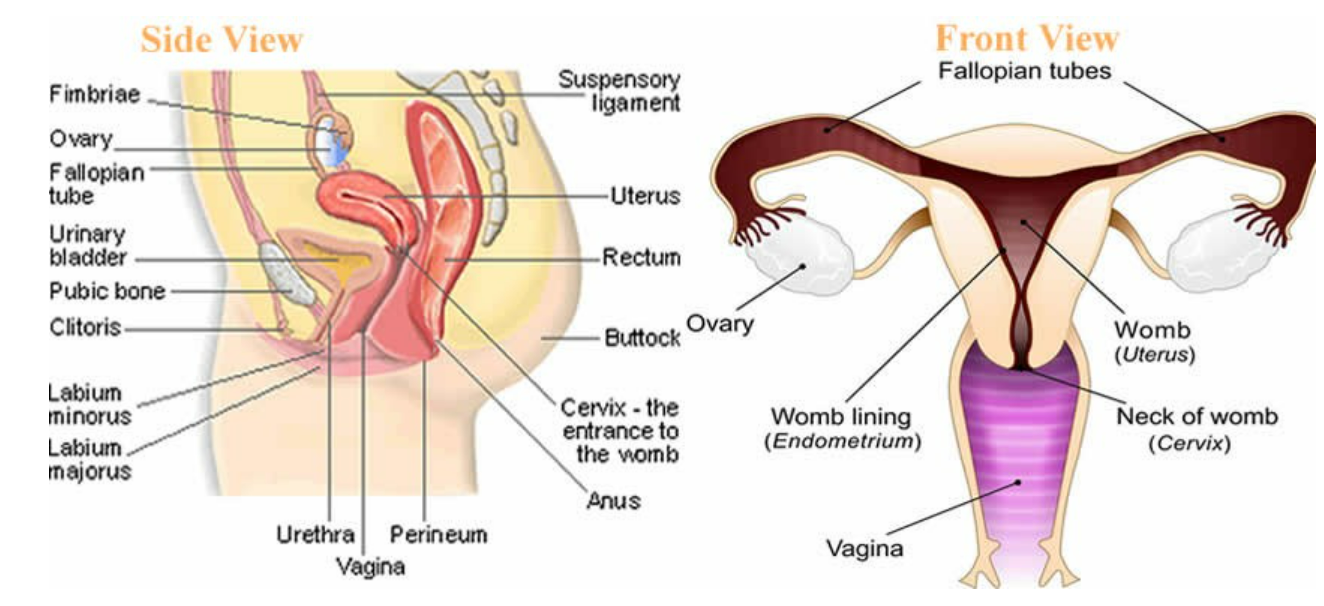
Human Reproduction: Male and Female Reproductive Systems
🌱 Introduction
Human reproduction is sexual and involves fusion of male and female gametes.
Humans are diploid, gametes are haploid → diploid number restored after fertilization.
Reproduction ensures continuation of species.
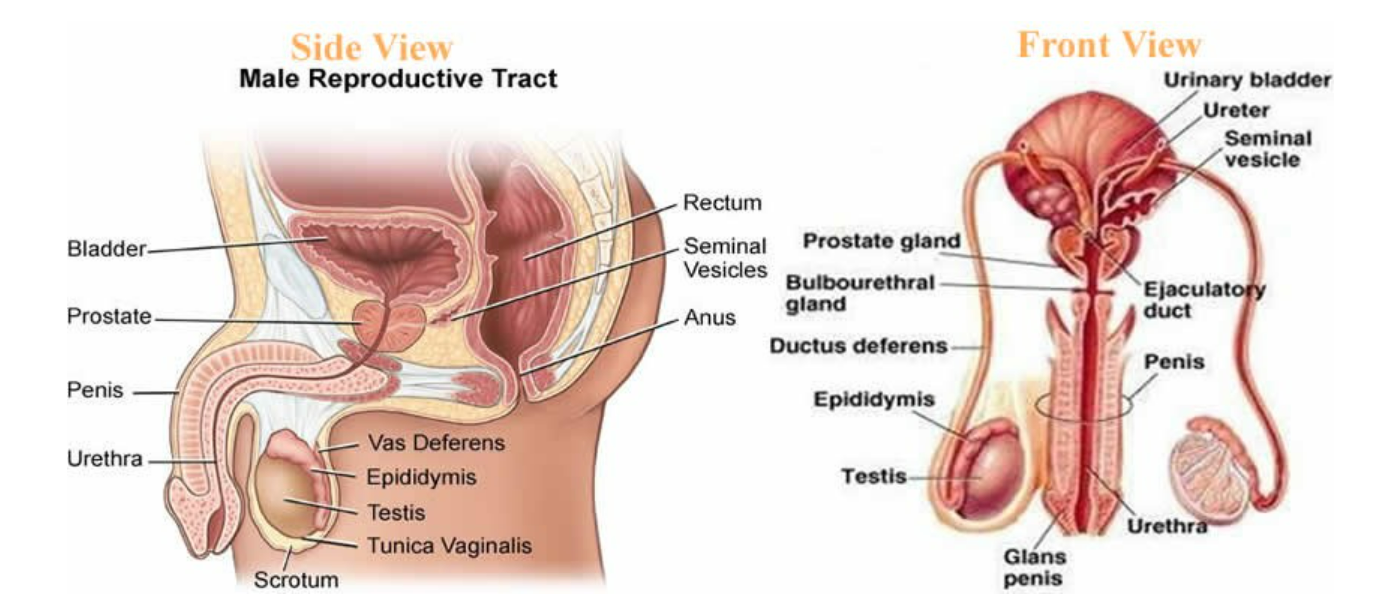
1. Male Reproductive System
Primary Reproductive Organ (Testes)
- Paired, oval, located in scrotum.
- Produce sperm (male gamete) and testosterone (male sex hormone).
- Contain seminiferous tubules → site of spermatogenesis.
Accessory Reproductive Organs
| Organ | Structure & Function |
|---|---|
| Epididymis | Coiled tube on testes; stores sperm and allows them to mature |
| Vas deferens | Muscular tube connecting epididymis to urethra; transports sperm during ejaculation |
| Seminal vesicles | Paired glands; secrete fructose-rich fluid, energy source for sperm |
| Prostate gland | Surrounds urethra; secretes alkaline fluid for sperm motility & protection from acidic vagina |
| Bulbourethral (Cowper’s) gland | Secretes mucus for lubrication & neutralizing urine traces in urethra |
External Genitalia
- Penis: Copulatory organ, delivers sperm into female tract.
- Urethra: Common pathway for semen and urine (not simultaneously).
Spermatogenesis
- Occurs in seminiferous tubules.
- Process: Spermatogonia (2n) → Primary spermatocytes (2n) → Secondary spermatocytes (n) → Spermatids (n) → Spermatozoa (n).
- Hormones: FSH → spermatogenesis, LH → testosterone production.
Sperm Structure
- Head → nucleus + acrosome (penetrates egg)
 Middle piece → mitochondria (energy)
Middle piece → mitochondria (energy)- Tail → flagellum (motility)
2. Female Reproductive System
Primary Reproductive Organs (Ovaries)
- Paired, oval, in pelvic cavity.
- Produce ova (eggs) and hormones: estrogen & progesterone.
- Contain follicles, each with an oocyte.
Accessory Reproductive Organs
| Organ | Structure & Function |
|---|---|
| Fallopian tubes / Oviducts | Connect ovary to uterus; site of fertilization |
| Uterus | Muscular, pear-shaped; implantation of zygote; supports fetus |
| Cervix | Narrow opening of uterus into vagina; protects uterus |
| Vagina | Muscular tube; receives penis; passage for childbirth and menstruation |
Oogenesis
- Occurs in ovaries.
- Process: Oogonia (2n) → Primary oocyte (2n) → Secondary oocyte (n) + Polar body → Ovum (n).
- Begins before birth, completes after fertilization.
- Hormones: FSH → follicle development, LH → ovulation, estrogen & progesterone → regulate menstrual cycle & pregnancy.
Female Gamete (Ovum) Structure
- Nucleus → genetic material
- Cytoplasm → nutrients for early embryo
- Zona pellucida → glycoprotein layer; sperm recognition
- Corona radiata → surrounding follicle cells
Key Differences Between Male & Female Reproductive Systems
| Feature | Male | Female |
|---|---|---|
| Primary organ | Testes | Ovaries |
| Gamete | Sperm | Ovum |
| Hormones | Testosterone | Estrogen, Progesterone |
| Gamete production | Continuous from puberty | Cyclic, limited number of eggs |
| Fertilization site | External (penis delivers sperm) | Internal (oviduct) |
| Accessory glands | Seminal vesicles, prostate, Cowper’s | None like male, mainly secretory cells in vagina/uterus |
🔑 Quick Recap
Humans reproduce sexually, involving male (sperm) & female (ovum) gametes.
Testes → sperm + testosterone; Ovaries → ovum + estrogen & progesterone.
Spermatogenesis → continuous; Oogenesis → cyclic & limited.
Fertilization occurs in fallopian tube, zygote implants in uterus.
Accessory organs aid in transport, nourishment, and protection of gametes.
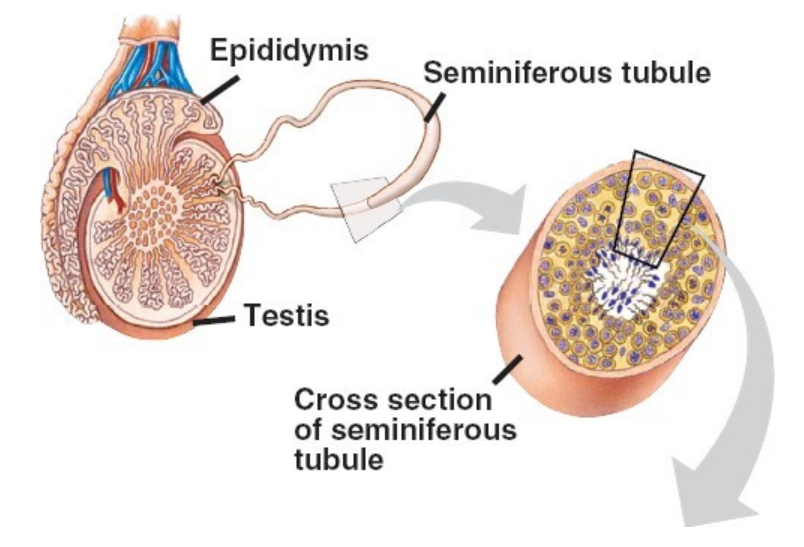
Microscopic Anatomy of Testis and Ovary
🌱 Introduction
Microscopic study helps understand spermatogenesis and oogenesis at cellular level.
Both organs have specialized structures for gamete formation and hormone secretion.
Microscopic Anatomy of Testis
1. Seminiferous Tubules
- Structure: Coiled tubes (~30–70 cm each), lined with germinal epithelium.

- Function: Site of sperm formation (spermatogenesis).
Cell Types in Germinal Epithelium
- Spermatogenic cells → form sperm
- Spermatogonia (2n) → stem cells
- Primary spermatocytes (2n) → undergo meiosis I
- Secondary spermatocytes (n) → undergo meiosis II
- Spermatids (n) → differentiate into spermatozoa
Sertoli cells (Sustentacular cells)
- Tall, columnar cells
- Support, nourish, and protect developing sperm
- Secrete inhibin → regulates FSH
Leydig cells (Interstitial cells)
- Found in interstitial tissue between tubules
- Secrete testosterone → secondary sexual characteristics & spermatogenesis
2. Basement Membrane & Connective Tissue
- Surrounds seminiferous tubules
- Contains blood vessels, lymphatics, and nerves
3. Spermiogenesis
- Transformation of spermatids → spermatozoa
- Involves formation of head (nucleus + acrosome), middle piece (mitochondria), and tail (flagellum)
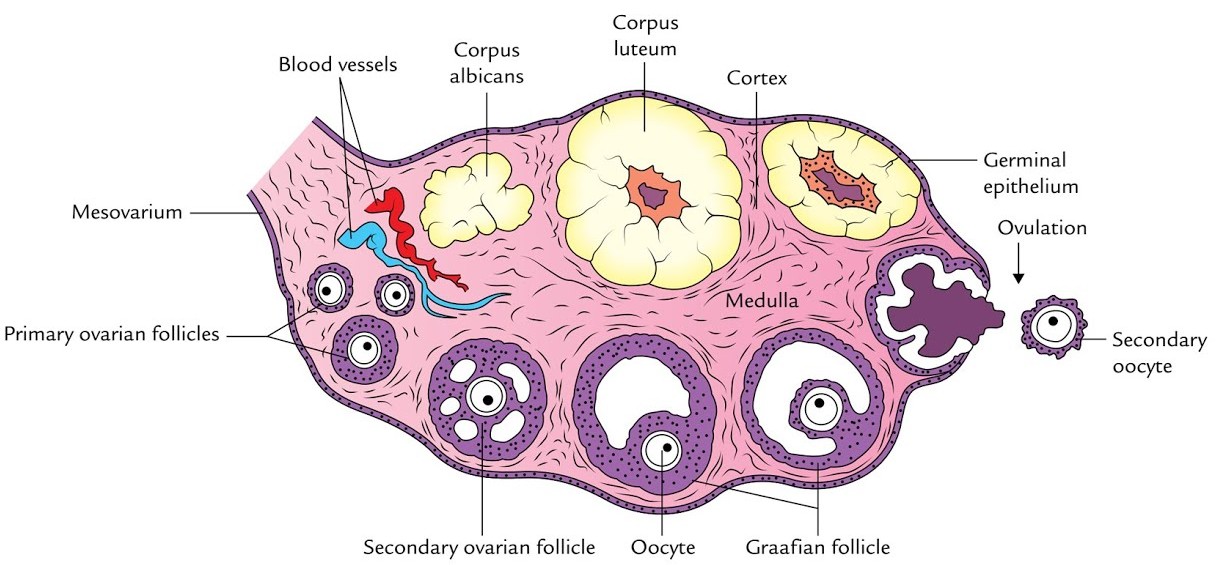
Microscopic Anatomy of Ovary
1. Ovarian Cortex
- Outer region containing follicles at different stages:
- Primordial follicle → single layer of squamous follicular cells around oocyte

- Primary follicle → cuboidal follicular cells, zona pellucida appears
- Secondary follicle → multiple layers (granulosa cells), theca cells form
- Graafian (mature) follicle → antrum appears, ready for ovulation
- Primordial follicle → single layer of squamous follicular cells around oocyte
- Function: Site of oogenesis and follicle maturation
2. Ovarian Medulla
- Inner region of ovary
- Contains blood vessels, lymphatics, and connective tissue
- Supports cortex
3. Follicular Cells
- Granulosa cells → surround oocyte, produce estrogen, nourish oocyte
- Theca cells → form outer layer, produce androgens (converted to estrogen by granulosa cells)
4. Corpus Luteum & Corpus Albicans
- Corpus luteum → formed from post-ovulation follicle; secretes progesterone and some estrogen
- Corpus albicans → degenerated corpus luteum if pregnancy does not occur
📊 Key Comparison: Testis vs Ovary Microscopic Structure
| Feature | Testis | Ovary |
|---|---|---|
| Primary tissue | Seminiferous tubules | Follicles in cortex |
| Gamete formation | Continuous | Cyclic |
| Supporting cells | Sertoli cells (nourish sperm), Leydig cells (testosterone) | Granulosa cells (nourish oocyte, secrete estrogen), Theca cells (androgen → estrogen) |
| Hormone secretion | Testosterone | Estrogen, Progesterone |
| Interstitial tissue | Between tubules, contains Leydig cells | Medulla, vascular connective tissue |
🔑 Quick Recap
Testis → seminiferous tubules + Leydig cells → sperm + testosterone
Spermatogenesis → spermatogonia → primary → secondary → spermatids → spermatozoa
Ovary → cortex (follicles) + medulla (supportive tissue)
Oogenesis → primordial → primary → secondary → Graafian → ovulation
Corpus luteum → secretes progesterone, corpus albicans → degenerates
Both organs have specialized supporting cells for gamete nutrition and hormone secretion
Gametogenesis and Menstrual Cycle
🌱 Introduction
Gametogenesis → formation of haploid gametes (sperm and ovum) from diploid germ cells.
Ensures sexual reproduction and genetic variation.
Includes spermatogenesis (male) and oogenesis (female).
Menstrual cycle → cyclical changes in female reproductive system to prepare for fertilization and pregnancy.
Spermatogenesis (Male Gametogenesis)
Definition
Process by which spermatozoa are formed from spermatogonia in the seminiferous tubules of testis.
Stages of Spermatogenesis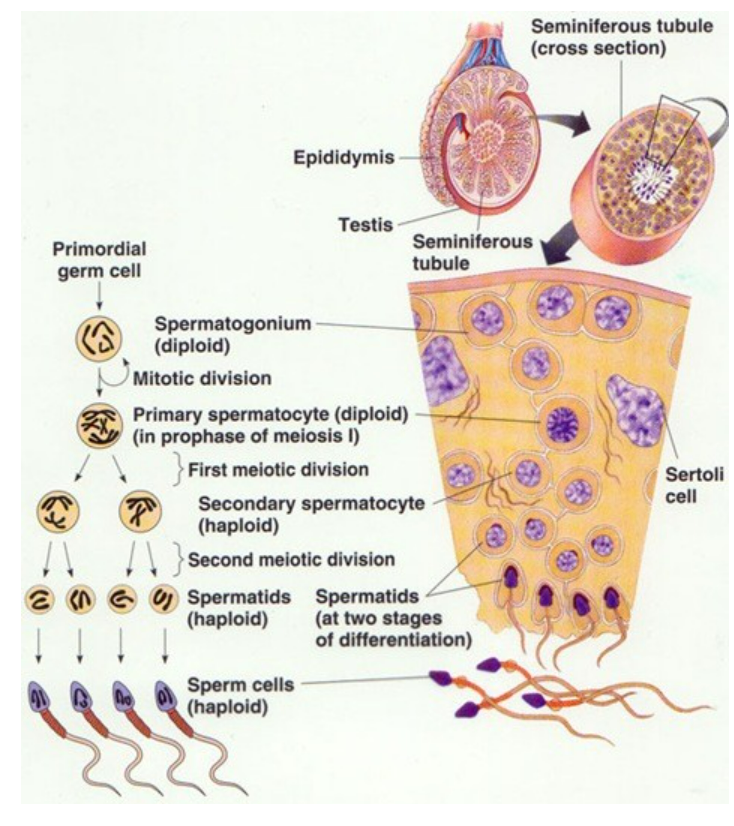
Spermatogonial Phase (Mitotic Division)
- Spermatogonia (2n) divide by mitosis
- Forms type A (stem cells) → maintain population
- Type B → differentiate into primary spermatocytes
Spermatocyte Phase (Meiotic Division)
- Primary spermatocyte (2n) → Meiosis I → Secondary spermatocytes (n)
- Secondary spermatocyte (n) → Meiosis II → Spermatids (n)
Spermatid Phase (Spermiogenesis / Differentiation)
- Spermatids → spermatozoa
- Formation of head (nucleus + acrosome), middle piece (mitochondria), tail (flagellum)
- Duration: ~64 days
Hormonal Regulation
- FSH → stimulates Sertoli cells → spermatogenesis
- LH → stimulates Leydig cells → testosterone
- Testosterone → supports maturation & secondary sexual characteristics
Oogenesis (Female Gametogenesis)
Definition
Formation of ova from oogonia in ovary.
Stages of Oogenesis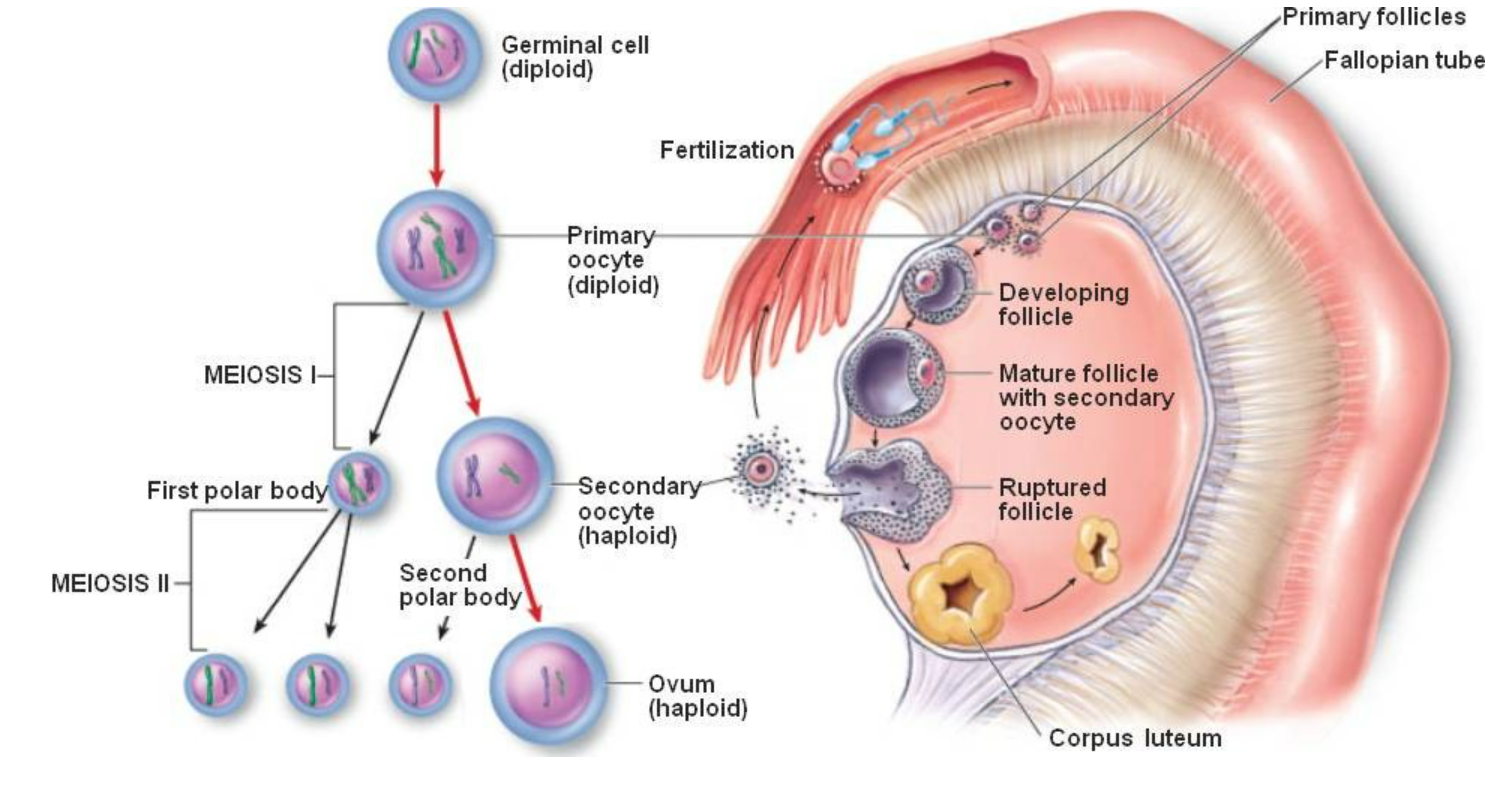
- Oogonia (2n) → multiply by mitosis during fetal life
- Primary oocyte (2n) → begins meiosis I, arrested in prophase I until puberty
- Secondary oocyte (n) + first polar body → completes meiosis I at ovulation
- Ovum (n) + second polar body → forms after fertilization when meiosis II completes
Key Points
- Cyclic process (unlike continuous spermatogenesis)
- Limited number of oocytes (~400 mature ovulated in lifetime)
- Hormones: FSH → follicle development, LH → ovulation, Estrogen & Progesterone → menstrual cycle regulation
🔑 Quick Recap
Gametogenesis: spermatogenesis (continuous, testes) & oogenesis (cyclic, ovaries)
Spermatogenesis: Spermatogonia → Primary → Secondary → Spermatid → Sperm
Oogenesis: Oogonia → Primary → Secondary → Ovum (fertilization completes meiosis II)
Menstrual Cycle
🌱 Introduction
The menstrual cycle is a recurrent, cyclic series of changes in the female reproductive system.
Prepares the uterus for implantation of a fertilized egg.
Duration: ~28 days (can vary 21–35 days).
Controlled by hormones from hypothalamus, pituitary, and ovary.
Phases of Menstrual Cycle
A. Ovarian Cycle – Changes in ovary
Follicular Phase (Day 1-13)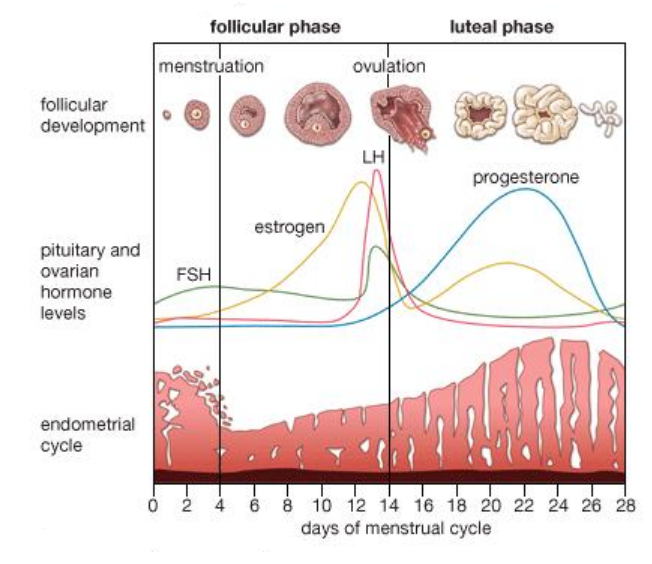
- Stimulus: FSH (from anterior pituitary)
- Growth of primary follicles → secondary follicles → Graafian follicle
- Follicular cells secrete estrogen → endometrium proliferation
- Key Event: Preparation of oocyte for ovulation
Ovulation (Day 14)
- Triggered by LH surge (from anterior pituitary)
- Release of secondary oocyte from Graafian follicle into fallopian tube
- Estrogen levels peak just before LH surge
Luteal Phase (Day 15-28)
- Post-ovulation, Graafian follicle transforms into corpus luteum
- Corpus luteum secretes progesterone + some estrogen
- Progesterone maintains secretory endometrium, preparing for implantation
B. Uterine (Endometrial) Cycle – Changes in uterus
Menstrual Phase (Day 1-5)
- Shedding of functional layer of endometrium
- Occurs if fertilization does not happen
- Blood, mucus, and epithelial cells expelled → menstrual flow
Proliferative Phase (Day 6-14)
- Endometrium regenerates and thickens under estrogen influence
- Glands and blood vessels develop in functional layer
Secretory Phase (Day 15-28)
- Under progesterone from corpus luteum
- Endometrium becomes thick, vascular, glandular → ready for implantation
Hormonal Regulation
| Hormone | Source | Function in Menstrual Cycle |
|---|---|---|
| GnRH | Hypothalamus | Stimulates FSH & LH secretion |
| FSH | Anterior pituitary | Stimulates follicle growth & estrogen secretion |
| LH | Anterior pituitary | Induces ovulation & corpus luteum formation |
| Estrogen | Ovarian follicles | Proliferation of endometrium, LH surge induction |
| Progesterone | Corpus luteum | Maintains secretory endometrium for implantation |
Key Points
- Average cycle length: 28 days
- Ovulation occurs ~Day 14
- Fertilization window: 12–24 hours after ovulation
- If fertilization does not occur → corpus luteum degenerates → progesterone ↓ → menstruation
- If fertilization occurs → corpus luteum persists → maintains early pregnancy
🔑 Quick Recap
Menstrual cycle = ovarian cycle + uterine cycle (~28 days)
Ovarian cycle: Follicular → Ovulation → Luteal phase
Uterine cycle: Menstrual → Proliferative → Secretory phase
Hormones: FSH → follicle, LH → ovulation, Estrogen → proliferation, Progesterone → secretory maintenance
Key concept: coordination of hormones ensures gamete release, endometrial preparation, and menstruation
Fertilization, Embryo Development, and Implantation
🌱 Introduction
Fertilization is the fusion of male and female gametes to form a zygote.
In humans, it occurs in the ampullary region of the fallopian tube.
Post-fertilization, the zygote undergoes cleavage, forms a morula, then a blastocyst, which implants into the uterus.
Fertilization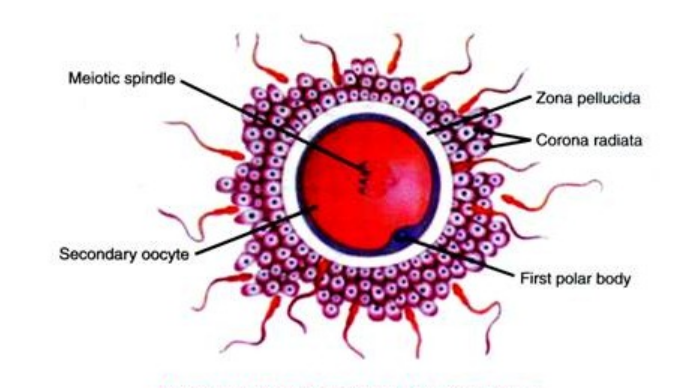
Definition
Fusion of haploid sperm (n) and haploid ovum (n) → diploid zygote (2n).
Steps of Fertilization
Sperm Capacitation
- Sperm gain fertilizing ability in the female reproductive tract
- Changes in membrane permeability and motility
Sperm Penetration
- Penetrates Corona radiata → outer follicular cells
- Penetrates Zona pellucida → acrosomal reaction releases enzymes (hyaluronidase, acrosin)
Fusion of Membranes
- Sperm and ovum plasma membranes fuse
- Sperm nucleus enters ovum cytoplasm
Cortical Reaction
- Prevents polyspermy (entry of multiple sperms)
- Zona pellucida hardens
Formation of Male & Female Pronuclei
- Sperm nucleus → male pronucleus
- Ovum nucleus → female pronucleus
- Both pronuclei fuse → zygote (2n)
Embryo Development up to Blastocyst
A. Cleavage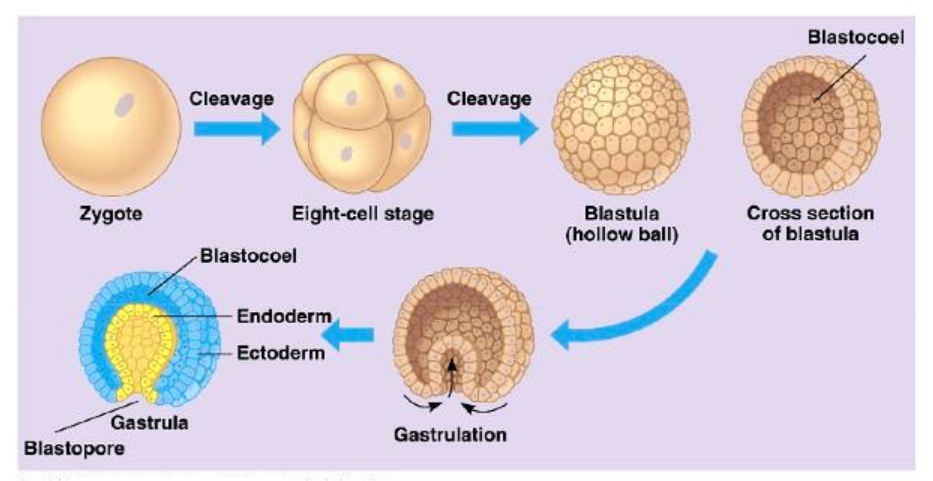
- Rapid mitotic divisions of zygote without growth
- Forms blastomeres
- Occurs during transport through fallopian tube
B. Morula Formation
- After 3–4 days, 16–32 blastomeres form a solid ball → morula
C. Blastocyst Formation (Day 5–6)
- Morula develops a fluid-filled cavity (blastocoel) → becomes blastocyst
- Two distinct cell types:
- Trophoblast → outer layer; contributes to placenta formation
- Inner Cell Mass (ICM) → cluster of cells inside; forms embryo proper
- Zona pellucida breaks down → prepares for implantation (hatching)
Implantation
Definition
Attachment and embedding of blastocyst into the uterine endometrium (~6–7 days after fertilization).
Steps of Implantation
Apposition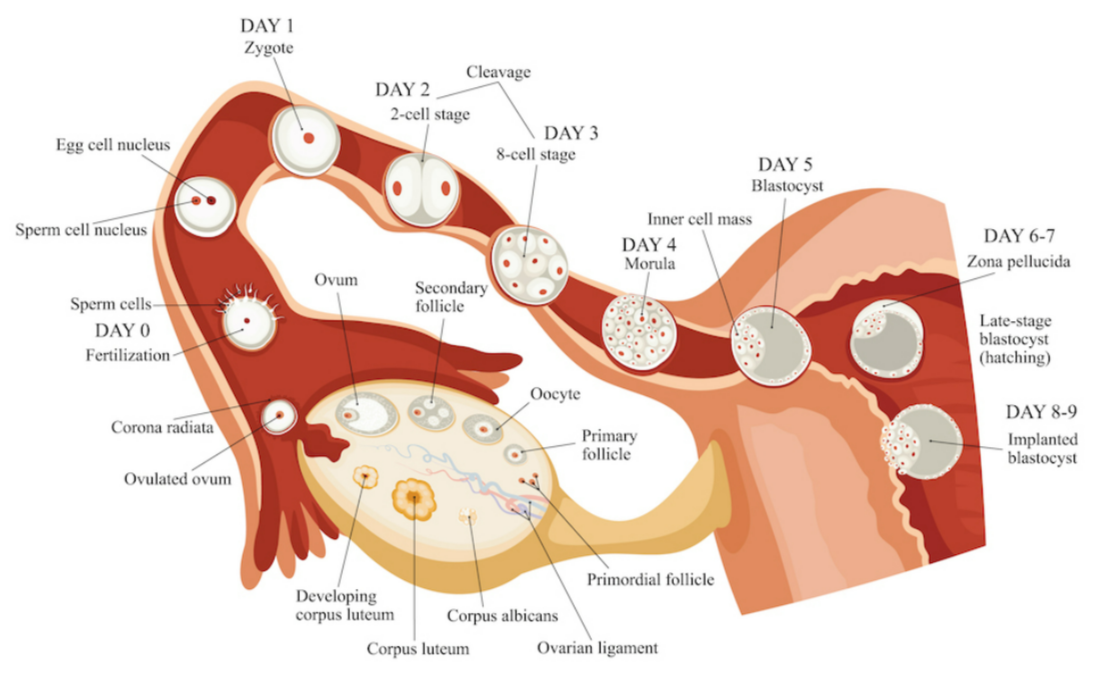
- Blastocyst loosely attaches to endometrium (uterine lining)
Adhesion
- Trophoblast cells adhere more firmly via cell adhesion molecules
Invasion / Embedding
- Trophoblast differentiates into:
- Cytotrophoblast → inner layer
- Syncytiotrophoblast → outer layer, invades endometrium
- Blastocyst burrows into endometrium, establishing maternal-fetal contact
Hormonal Support
- Progesterone (from corpus luteum) → maintains endometrium
- Estrogen → supports vascularization and glandular secretions
Significance
- Ensures nutrient supply for embryo
- Initiates placenta formation
🔑 Quick Recap
Fertilization: fusion of sperm + ovum → zygote
Key steps: capacitation → sperm penetration → membrane fusion → cortical reaction → pronuclei formation
Cleavage → Morula → Blastocyst
Blastocyst: Trophoblast → placenta, ICM → embryo
Implantation: blastocyst embeds into uterine endometrium (~Day 6–7)
Hormonal control: Progesterone & Estrogen maintain endometrium for early embryo survival
Pregnancy and Placenta Formation
🌱 Introduction
Pregnancy (Gestation) → period from fertilization to childbirth (~280 days / 40 weeks in humans).
Begins with implantation of the blastocyst and ends with parturition.
Placenta plays a vital role in fetal nourishment, respiration, and waste removal.
Pregnancy
Definition
State in which a developing embryo/fetus is maintained in the uterus until it can survive independently.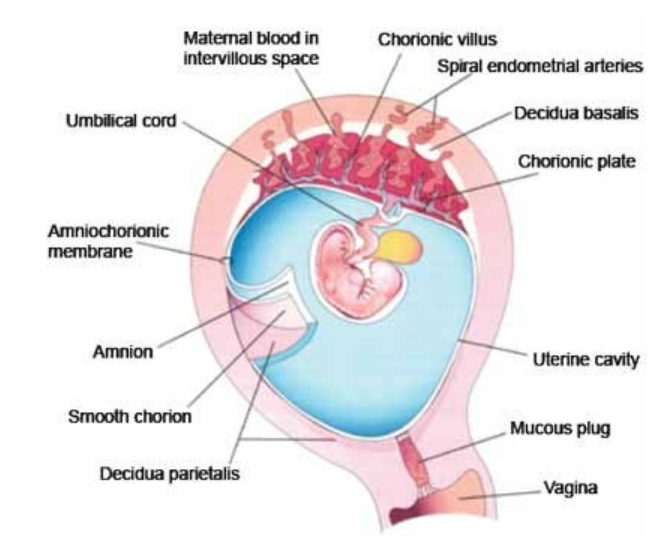
Stages of Pregnancy
- Zygote Stage → fertilization in fallopian tube
- Embryonic Stage (Weeks 1–8)
- Rapid cell division, differentiation
- Formation of major organs and tissues
- Fetal Stage (Weeks 9–40)
- Growth and maturation of organs
- Increase in size, weight, and complexity
Hormonal Support of Pregnancy
- Progesterone → maintains endometrium, inhibits uterine contractions
- Estrogen → promotes uterine growth and blood supply
- hCG (human chorionic gonadotropin) → secreted by trophoblast; maintains corpus luteum in early pregnancy
Placenta Formation
Definition
Placenta → temporary organ connecting fetus and mother, facilitating nutrient, gas, and waste exchange.
Development
Trophoblast Differentiation
- Outer layer of blastocyst → cytotrophoblast + syncytiotrophoblast
- Invades endometrium
Chorionic Villi Formation
- Finger-like projections of trophoblast → increase surface area
- Surrounded by maternal blood lacunae → maternal-fetal exchange
Mature Placenta
- Fully functional by 3rd month
- Fetal part: chorionic villi
- Maternal part: decidua basalis
- Connected to fetus by umbilical cord (2 arteries, 1 vein)
Functions of Placenta
- Exchange of oxygen, CO₂, nutrients, and waste
- Secretion of hormones: hCG, progesterone, estrogen
- Acts as barrier against some harmful substances (not all)
- Supports fetal growth and development
🔑 Quick Recap
Pregnancy: zygote → embryo → fetus → childbirth (~280 days)
Placenta: temporary organ connecting mother & fetus
Trophoblast → Chorionic villi → Placenta
Functions: nutrient & gas exchange, hormone secretion, fetal protection
Hormones: Progesterone & Estrogen → maintain pregnancy, hCG → corpus luteum maintenance
Parturition (Childbirth)
🌱 Introduction
Parturition is the process by which a fully developed fetus is expelled from the uterus through the birth canal.
Marks the end of pregnancy (~280 days in humans).
Requires coordination between fetus, uterus, cervix, placenta, and hormones.
Ensures safe delivery of the baby and preparation of the uterus for involution.
Prerequisites for Parturition
- Mature fetus: fetal lungs, CNS, and endocrine system ready for independent life
- Placenta and uterus readiness: estrogen increases, progesterone decreases
- Cervical ripening: softening and dilation
- Maternal system readiness: pelvic muscles, ligaments, and birth canal prepared
Stages of Parturition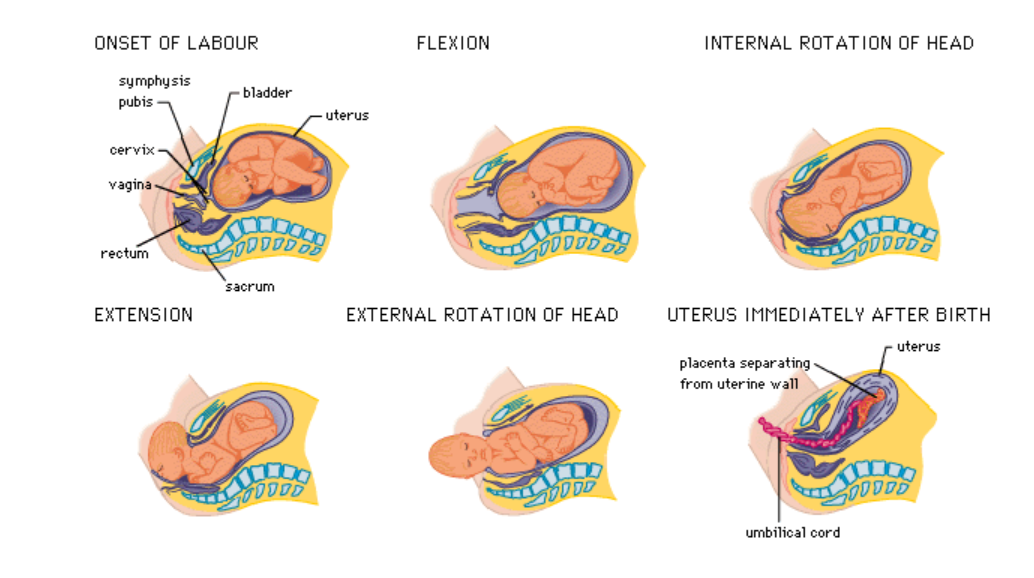
Stage 1: Dilation of Cervix (Preparatory Stage)
- Duration: 6–12 hours (first pregnancy may take longer)
- Events:
- Uterus develops irregular, weak contractions initially → gradually become strong and regular
- Cervix softens and dilates up to 10 cm
- Amniotic sac may rupture → “water breaks”
- Hormonal influence:
- Estrogen ↑ → myometrium more excitable, promotes contractions
- Progesterone ↓ → reduces inhibition of contractions
- Relaxin → softens cervix and ligaments
Stage 2: Expulsion of Fetus (Delivery Stage)
- Duration: 20 minutes–2 hours
- Events:
- Strong, rhythmic uterine contractions push fetus through birth canal
- Fetal positioning: usually cephalic presentation (head first)
- Umbilical cord clamping after delivery of fetus
- Hormonal influence:
- Oxytocin (posterior pituitary) → stimulates myometrial contractions
- Prostaglandins → enhance contractions, cervical ripening
Stage 3: Placental Stage (Afterbirth)
- Duration: 5–30 minutes after delivery
- Events:
- Detachment of placenta and fetal membranes from uterine wall
- Expelled through uterine contractions
- Uterine contraction helps prevent postpartum hemorrhage
- Hormonal influence:
- Oxytocin → continues contractions
- Prostaglandins → facilitate placental expulsion
Hormonal Regulation of Parturition
| Hormone | Source | Role |
|---|---|---|
| Estrogen | Placenta | Increases uterine excitability; upregulates oxytocin receptors |
| Progesterone | Placenta | Falls near term → removes inhibition of contractions |
| Oxytocin | Posterior pituitary | Stimulates strong, rhythmic contractions; positive feedback loop |
| Prostaglandins | Uterus & fetal membranes | Enhance contractions and cervical softening |
| Relaxin | Corpus luteum & placenta | Softens cervix and pelvic ligaments |
| Fetal Cortisol | Fetal adrenal glands | Stimulates estrogen production, initiates labor |
Mechanism of Parturition
- Fetal maturity signals → cortisol secretion ↑
- Cortisol → placental estrogen ↑, progesterone ↓ → uterus prepared
- Estrogen ↑ → myometrium excitable; oxytocin receptors upregulated
- Positive feedback loop: uterine contractions → oxytocin release → stronger contractions
- Cervix dilates → fetus expelled → placenta delivered
Key Points
- Parturition is hormonally controlled, mechanically assisted, and fetus-triggered
- Stages:
- Dilation – cervix softens & opens
- Expulsion – fetus delivered
- Placental – placenta & membranes expelled
- Hormones essential: Estrogen, Progesterone, Oxytocin, Prostaglandins, Relaxin, Fetal cortisol
- Positive feedback loop: contractions → oxytocin → stronger contractions → delivery
🔑 Quick Recap
Parturition = childbirth (expulsion of fetus, placenta, membranes)
Stage 1: Cervical dilation (~6–12 hrs)
Stage 2: Fetal expulsion (20 min–2 hrs)
Stage 3: Placental expulsion (5–30 min)
Hormonal regulation: ↑ Estrogen, ↓ Progesterone → uterus ready
Oxytocin & Prostaglandins → contractions
Fetal cortisol → triggers labor
Significance: Ensures safe delivery and uterine involution
Lactation
🌱 Introduction
Lactation → process of milk secretion by mammary glands in postpartum period.
Provides nutrition, immunity, and growth factors to the newborn.
Controlled by hormones and neuroendocrine reflexes.
Mammary Glands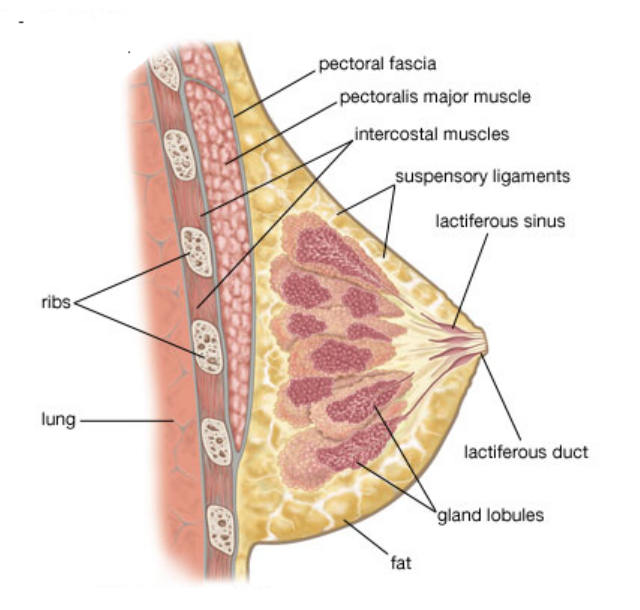
Specialized exocrine glands located in the breast.
- Alveoli → milk-producing sacs lined by secretory epithelial cells
- Myoepithelial cells → contract to eject milk
- Lactiferous ducts → carry milk to nipple
- Milk is stored in alveoli and ducts until suckling occurs
Phases of Milk Secretion
Lactogenesis
- Initiation of milk production post-delivery
- Triggered by drop in progesterone after placenta removal
- Prolactin (anterior pituitary) → stimulates milk synthesis
Galactopoiesis
- Maintenance of milk secretion during breastfeeding
- Prolactin continues to stimulate milk production
- Suckling stimulus → prolactin release
Milk Ejection / Let-down Reflex
- Neuroendocrine reflex triggered by suckling
- Oxytocin (posterior pituitary) → contraction of myoepithelial cells
- Milk is ejected into lactiferous ducts and nipple
Hormonal Regulation of Lactation
| Hormone | Source | Role |
|---|---|---|
| Prolactin | Anterior pituitary | Stimulates milk synthesis (alveolar cells) |
| Oxytocin | Posterior pituitary | Causes milk ejection (let-down reflex) |
| Estrogen | Placenta | Prepares mammary ducts during pregnancy |
| Progesterone | Placenta | Prepares alveoli; drops after delivery to allow lactation |
| Growth Hormone & Cortisol | Anterior pituitary & adrenal | Support milk protein synthesis |
| Insulin | Pancreas | Supports lactose synthesis |
Key Points
- Milk secretion begins immediately after birth (colostrum first 2–3 days)
- Colostrum: rich in antibodies (IgA), proteins, and growth factors
- Suckling reflex maintains milk production (prolactin) and ejection (oxytocin)
- Breastfeeding → provides immunity, nutrition, and bonding between mother and baby
🔑 Quick Recap
Lactation = milk production & ejection from mammary glands
Phases: Lactogenesis → Galactopoiesis → Milk ejection
Hormones: Prolactin → synthesis, Oxytocin → ejection, Estrogen & Progesterone → preparation
Colostrum → first milk, rich in antibodies
Suckling reflex → maintains milk secretion and let-down