NEET Biology - Unit 6- Reproductive health- Study Notes - New Syllabus
NEET Biology – Unit 6- Reproductive health- Study Notes – New Syllabus
Key Concepts:
- Reproductive health: Need for reproductive health and prevention of sexually transmitted diseases (STD); Birth control-Need and Methods, Contraception and Medical Termination of Pregnancy (MTP); Amniocentesis; Infertility and assisted reproductive technologies – IVF, ZIFT, GIFT (Elementary idea for general awareness).
Reproductive Health
🌱 Introduction
Reproductive health means complete physical, mental, and social well-being in all matters related to the reproductive system.
It is not just the absence of disease but also the ability to have a safe and satisfying sexual life and the freedom to decide on reproduction.
Need for Reproductive Health
- Ensures safe pregnancy and childbirth
- Prevents reproductive tract infections (RTIs) and sexually transmitted diseases (STDs)
- Promotes responsible sexual behavior
- Reduces infant and maternal mortality
- Improves quality of life and overall health
- Provides awareness about family planning
- Protects adolescents from early/unsafe sexual activity
Prevention of Sexually Transmitted Diseases (STDs)
STDs are infections transmitted through sexual contact.
Common examples: HIV/AIDS, Syphilis, Gonorrhea, Chlamydia, Hepatitis B, Genital herpes.
🌟 Preventive Measures
- Abstinence or delayed sexual activity – Avoid early sexual exposure
- Monogamous relationships – Reduces risk of infection
- Safe sex practices – Use of condoms prevents most STDs
- Avoid sharing needles – Prevents HIV and Hepatitis B
- Regular medical check-ups – Early detection and treatment of STDs
- Vaccination – Hepatitis B and HPV vaccines protect against viral STDs
- Education and awareness – Knowledge about STDs, their symptoms, and prevention is crucial
⚡ Quick Comparison Table: Common STDs
| STD | Causative Agent | Key Symptoms | Prevention |
|---|---|---|---|
| HIV/AIDS | Virus | Weakness, weight loss, frequent infections | Safe sex, avoid sharing needles |
| Syphilis | Bacterium | Sores, rashes | Safe sex, early treatment |
| Gonorrhea | Bacterium | Discharge, burning urination | Safe sex, early treatment |
| Chlamydia | Bacterium | Often asymptomatic, infertility | Safe sex, screening |
| Hepatitis B | Virus | Liver infection, jaundice | Vaccine, safe sex |
| Genital Herpes | Virus | Blisters on genitals | Safe sex, avoid sexual contact during outbreaks |
📝 Quick Recap
Reproductive health → physical, mental & social well-being in reproductive matters
Need → safe sex, safe pregnancy, prevention of RTIs/STDs, family planning awareness
STDs → HIV, Syphilis, Gonorrhea, Chlamydia, Hepatitis B, Herpes
Prevention → abstinence, monogamy, condoms, vaccination, awareness, early treatment
Birth Control and Reproductive Management
🌱 Introduction
Birth control refers to the regulation of conception using preventive methods or devices to limit the number of children.
It is essential to control population growth, improve maternal and child health, and promote responsible parenthood.
Population Explosion and Birth Control
- Population explosion → Rapid increase in human population over a short time
- Factors affecting population growth: Fertility & natality, Mortality, Migration, Age & sex structure
- Causes: Better health facilities, Improved living conditions, Decline in death rate, MMR & IMR
- Global & Indian context: World population ≈ 6 billion; Indians ≈ 1.3 billion; Growth rate ≈ 1.7%
- Urban population → Majority uneducated, affecting awareness about family planning
Need for Birth Control
- Limits family size and prevents unplanned pregnancies
- Reduces maternal & infant mortality and morbidity
- Prevents overpopulation & population-related social problems
- Promotes healthy spacing between children
- Contributes to economic stability and better quality of life
Contraception
Contraception → Birth control methods that deliberately prevent fertilization.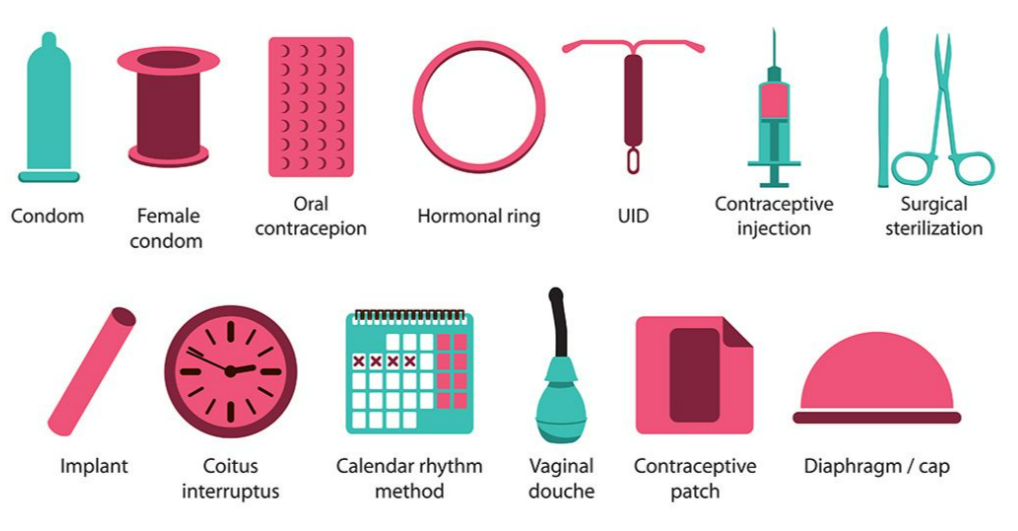
- Temporary (reversible) – Rhythm method, condoms, IUDs, hormonal methods
- Permanent – Tubectomy, vasectomy
Characteristics of an ideal contraceptive:
- User-friendly
- Easily available
- Minimal or no side-effects
- Does not interfere with sexual drive
Methods of Birth Control
| S. No | Method | Action |
|---|---|---|
| 1 | Rhythm Method | No intercourse during woman’s fertile period (day 12–20) |
| 2 | Withdrawal (Coitus Interruptus) | Penis withdrawn before ejaculation |
| 3 | Tubectomy / Tubal Ligation | Fallopian tubes cut and tied, permanently blocking sperm |
| 4 | Vasectomy | Vasa deferentia cut and tied, permanently blocking sperm |
| 5 | Intrauterine Device (IUD) | Small device in uterus prevents implantation; may release copper or hormones |
| 6 | Oral Contraceptive Pills (OCPs) | Synthetic estrogens and progestogens prevent ovulation |
| 7 | Male Condom | Thin rubber sheath collects semen, prevents sperm entry |
| 8 | Female Condom | Plastic pouch inserted into vagina catches semen |
| 9 | Diaphragm | Soft rubber cup covers uterus entrance, holds spermicide |
| 10 | Cervical Cap | Mini diaphragm covers cervix, holds spermicide |
| 11 | Foams, Creams, Jellies | Chemical spermicides inserted before intercourse |
| 12 | Implant (Norplant) | Hormone capsules under skin slowly release hormone to block ovulation |
| 13 | Injectable Contraceptive (Depo-Provera) | Hormonal injection every 3 months prevents ovulation |
Medical Termination of Pregnancy (MTP)
- Definition: Termination of pregnancy by medical or surgical methods within a safe period (up to 20 weeks in India)
- Medical abortion – Drugs like RU-486 (mifepristone) with misoprostol induce abortion in early pregnancy
- Surgical abortion – Suction, curettage, or dilation & evacuation for later stages
- Purpose: Prevent complications from unsafe abortions, reduce maternal mortality, maintain reproductive health
📝 Quick Recap
Birth control → Regulation of conception to control population
Contraception → Prevents fertilization; can be temporary or permanent
Population explosion causes → Better health, low death rate, high fertility
Ideal contraceptive → User-friendly, safe, available, minimal side effects
Methods → Rhythm, Withdrawal, IUD, Condoms, Diaphragm, Hormonal Pills, Implants, Tubectomy, Vasectomy
MTP → Safe termination of pregnancy medically or surgically to protect maternal health
Amniocentesis
🌱 Introduction
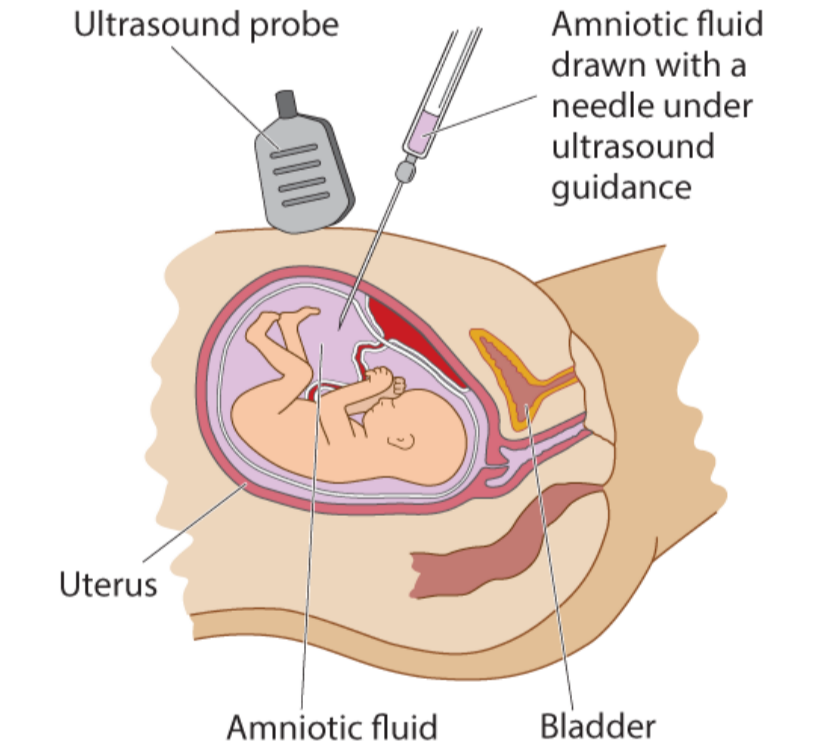
Amniocentesis is a prenatal diagnostic procedure to assess fetal health during pregnancy.
It helps detect genetic, chromosomal, and developmental disorders before birth.
Amniotic Fluid
- Fetus is surrounded by amniotic fluid inside the amniotic sac
- Components:
- Live fetal cells (mainly skin cells)

- Proteins like alpha-fetoprotein (AFP)
- Hormones, enzymes, and metabolic products
- Live fetal cells (mainly skin cells)
- Reflects health and development of the fetus
Purpose of Amniocentesis
- Genetic testing: Detect chromosomal abnormalities (e.g., Down syndrome)
- Neural tube defects: Detect spina bifida
- Metabolic disorders: Identify inherited metabolic diseases
- Fetal lung maturity assessment (late pregnancy)
- Detect infections or other abnormalities
Procedure
- Performed at 14–18 weeks of pregnancy
- Thin needle inserted through mother’s abdomen into amniotic sac under ultrasound guidance
- About 20 mL of amniotic fluid withdrawn carefully
- Fetal cells cultured and analyzed for chromosomal/genetic defects
- AFP and biochemical markers measured
Advantages
- Early detection of genetic or developmental disorders
- Helps parents make informed pregnancy decisions
- Useful in high-risk pregnancies (advanced maternal age, family history)
Limitations / Risks
- Slight risk of miscarriage (~0.1–0.3%)
- Risk of infection or fetal injury if procedure not done carefully
- Cannot detect all abnormalities
- Misuse for sex determination is illegal (prevents female foeticide)
📝 Quick Recap
Amniocentesis → Prenatal test using amniotic fluid to detect fetal health issues
Fluid contains: Fetal cells + alpha-fetoprotein + other substances
Purpose: Genetic testing, neural tube defects, metabolic disorders, lung maturity
Procedure: Needle through abdomen → withdraw fluid → analyze fetal cells & AFP
Risks: Miscarriage, infection, fetal injury; misuse for sex determination illegal
Timing: 14–18 weeks of pregnancy
Infertility & Assisted Reproductive Technologies (ART)
🌱 Introduction
Infertility and ART are key aspects of reproductive health awareness.
They address difficulties in conceiving and the techniques used to help couples have children.
Infertility
- Definition: Inability to conceive or produce children even after 2 years of unprotected sexual cohabitation
- Prevalence: Large number of couples in India face infertility
- Causes:
- Physical defects: blocked fallopian tubes, low sperm count
- Congenital abnormalities
- Diseases or infections
- Drugs or hormonal imbalances
- Immunological factors
- Psychological issues
 Assisted Reproductive Technologies (ART)
Assisted Reproductive Technologies (ART)
Definition: ART includes fertility techniques in which sperms and eggs are handled outside or within the female reproductive system to help couples conceive.
🌟 Main ART Techniques
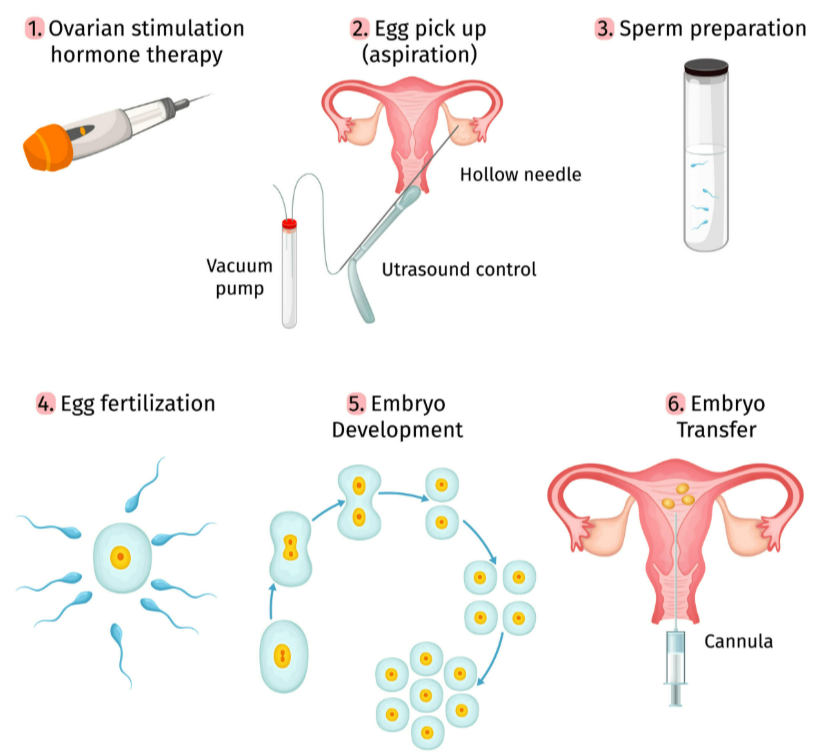
In Vitro Fertilization (IVF)
- Fertilization occurs outside the body under lab conditions (test tube baby programme)
- Eggs collected from wife/donor, sperms from husband/donor
- Fertilization induced in lab to form zygote
- Early embryos transferred into fallopian tube (ZIFT) or uterus
Zygote Intra-Fallopian Transfer (ZIFT)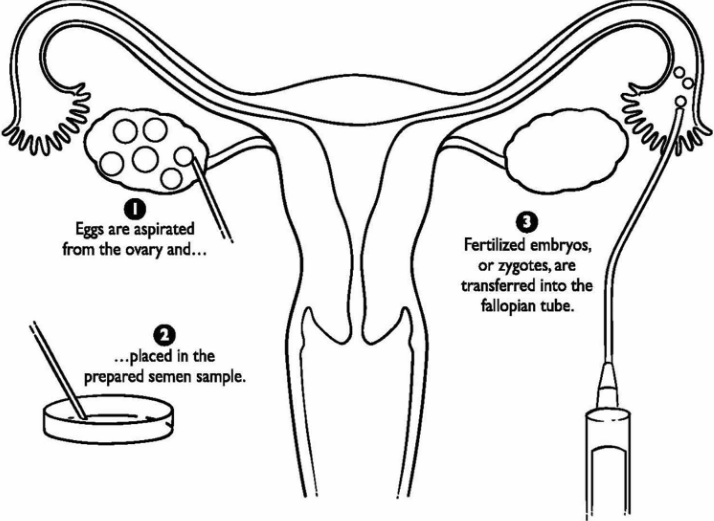
- Similar to IVF, but fertilized embryo transferred into fallopian tube instead of uterus
- Also called Tubal Embryo Transfer (TET)
Intra-Cytoplasmic Sperm Injection (ICSI)
- Single sperm injected directly into mature egg
- Used for male infertility or low sperm quality
- Fertilized egg placed in uterus or fallopian tube
Gamete Intra-Fallopian Transfer (GIFT)
- Eggs collected from donor placed into fallopian tube of recipient female
- Both eggs and sperm introduced via thin catheter using laparoscopy under general anesthesia
Artificial Insemination (AI)
- Used when male partner cannot inseminate naturally or sperm count is very low
- Semen from husband or donor introduced artificially into vagina or uterus (IUI – Intra Uterine Insemination)
📝 Quick Recap
Infertility → No conception after 2 years; causes → physical, congenital, disease, drugs, immunological, psychological
ART → Techniques to help infertile couples → IVF, ZIFT, ICSI, GIFT, AI
IVF → Fertilization outside the body → embryos transferred into uterus/fallopian tube
ZIFT → Fertilized embryo → fallopian tube
ICSI → Single sperm injected into egg → placed in uterus/fallopian tube
GIFT → Eggs + sperm → fallopian tube via laparoscopy
AI → Semen introduced artificially into vagina/uterus