Topic 6: Human physiology
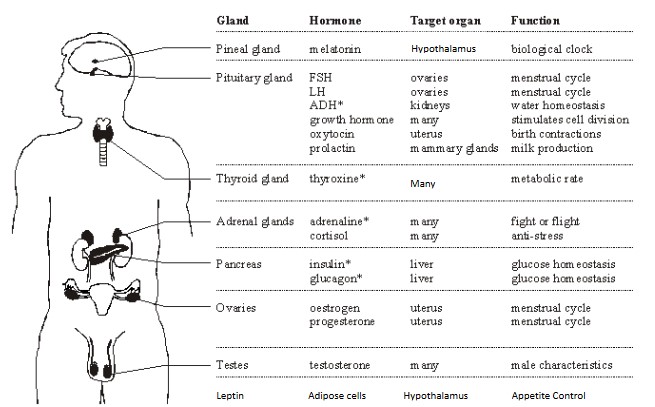
6.6 Hormones, homeostasis and reproduction
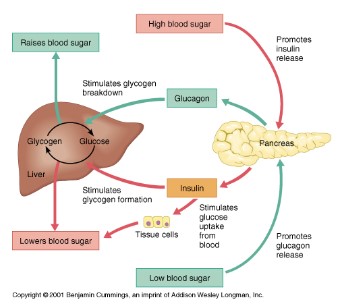
Blood sugar control
- Blood glucose concentration is carefully monitored by negative feedback mechanisms.
- Cellular respiration is constantly lowering blood glucose levels.
- Receptors in the pancreas sense when the blood glucose level is too low.
- Alpha (𝛂) cells in the pancreas secrete glucagon into the bloodstream.
- Glucagon stimulates the liver to breakdown stored glycogen into glucose which is released into the bloodstream.
- Blood glucose levels rise back to their normal limits.
- If the glucose levels get too high, receptors sense the increased glucose levels causing the pancreas to secrete insulin by the Beta cells (𝛃) in pancreas.
- Insulin stimulates the absorption of glucose from the blood into skeletal muscles and fat tissue, and thus allowing the liver to convert glucose into glycogen (animal carbohydrate storage molecule).
- Glucose levels decrease back to the normal range
Type I diabetes
- Is an autoimmune disease characterized by the inability of the pancreas to produce insulin. The insulin producing 𝛃 cells of the pancreas are attacked and destroyed by one’s own immune system.
- This type of diabetes usually develops in children, but can occur at any age.
- Therefore, the body loses the ability to take up glucose into its cells and convert glucose into glycogen.
- People that have type I diabetes must take insulin shots or injections
Type II diabetes
- Occurs when the insulin receptors on certain body cells lose their ability to process or respond to insulin, become insensitive.
- Pancreas still produces insulin.
- Type II diabetes is usually a result of obesity, age, lack of exercise and/or genetic predisposition.
- Type II diabetes is usually considered late onset as it usually occurs later on in life.
- Insulin injections are not needed. Diabetes II can be treated by lifestyle and diet changes.
- Most common form of diabetes.
- There is a strong hereditary relationship.
Metabolic rate regulation
- Thyroxin is a hormone secreted by the thyroid gland of the endocrine system
- Thyroxin contains iodine; therefore, prolonged deficiency to iodine in the diet prevents the production of thyroxin
- Thyroxin is important in the regulation of the body’s metabolic rate
- The body’s metabolic rate is the amount of energy a body uses at rest; combination of the catabolic and anabolic reactions
- Since thyroxin causes an increase in the body’s metabolic rate, there is an increase in oxygen consumption and the hydrolysis of ATP; thereby causing an increase in the body’s temperature
- Increase in thyroxin stimulates the breakdown of lipids and the oxidation of fatty acids
- Thyroxin also stimulates carbohydrate metabolism, including the uptake of glucose and the breakdown of glycogen into free glucose
- In a regular person, if the bodies temperature drops, a release in thyroxin will stimulate heat production causing the body’s temperature to rise
- If there is an excessive amount of thyroxin in the body, hyperthyroidism can occur
- If there is an insufficient amount of thyroxin in the body, hypothyroidism can occur
- Some of the symptoms of hypothyroidism are weight gain, loss of energy, feeling cold all the time, forgetfulness and depression
Appetite control
- Leptin is a hormone made by adipose cells that helps to regulate energy balance by inhibiting hunger.
- Leptin acts on the receptors in the arcuate nucleus (collection of neurons) of the hypothalamus to regulate appetite in order to achieve energy homeostasis
- The concentration of leptin in the blood is controlled by food intake and the amount of adipose tissue in the body
- If the amount of adipose tissue in an individual increases, then their concentrations of leptin also increases, leading to long term suppression of appetite and reduced food intake
- In obese individuals a decreased sensitivity to leptin can occur, resulting in an inability to recognize when they are full
- Trials with humans have had mixed response since the physiology of humans is much different than mice
- Since most humans have quite a high leptin concentration, it was determined that the many of obesity cases where caused by a change in the receptor protein for leptin, not in the production of leptin
Circadian rhythms control
- Melatonin is a hormone made by the pineal gland in darkness, a small gland in the brain.
- The secretion of melatonin by the pineal gland is controlled by cells in the hypothalamus
- Light exposure to the retina is relayed to the suprachiasmatic nucleus (SCN) of the hypothalamus. These fibers from the hypothalamus relay a message to the nerve ganglia of the spinal cord which is relayed back to the pineal gland to release melatonin.
- Melatonin helps control your sleep and wake cycles (circadian rhythms).
- Melatonin levels generally begin to rise in the mid to late evening, remaining high for most of the night, and then drop in the early morning hours
Jet lag
- The SCN of the hypothalamus and the pineal gland continually set the circadian rhythm of the place the person is departing from.
- Therefore, when a person lands in a country that is many time zones different than the origin, they feel sleepy in the day and awake at night
- Jet lag will only last a few days, as the body adjusts to the new times when the light is detected by the cells in the retina during a different time period
Sex determination
- The Y chromosome has a gene called the SRY gene that causes the embryonic gonads to become testes and begin secreting testosterone
- SRY codes for a protein called TDF (testis-determining factor) that stimulates the expression of other genes located on the Y chromosome that cause testis development
- If there are two X chromosomes, the gonads develop as ovaries
- TDF is a DNA binding protein, which promotes expression of other gens for the development of testis.
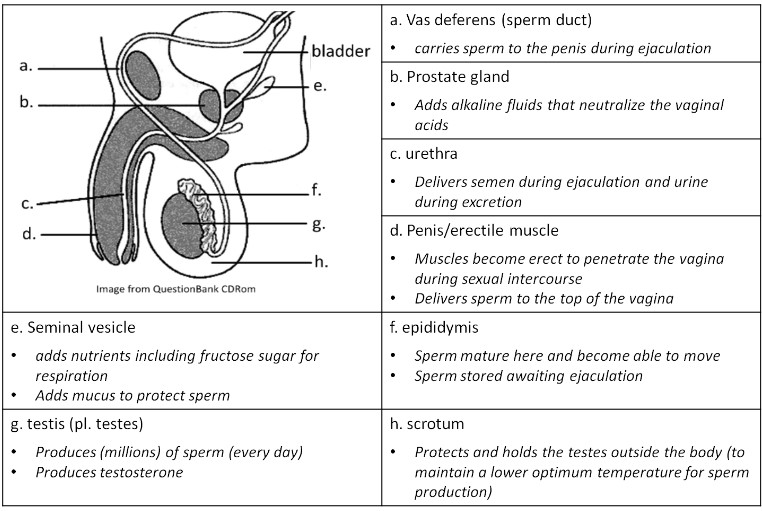
Testosterone
- Secreted in the testes of males or the early stage testosterone-secreting cells that will become testes.
- Aid in the development and maturation of the male genitalia as a fetus at about the 8th to 9th week.
- During puberty, testosterone aids in the development of male secondary sexual characteristics such as pubic and facial hair, enlarged penis, broad shoulders, muscle mass, deepening of voice and bone density.
- Stimulates production of sperm and promotes the male libido (sex drive)
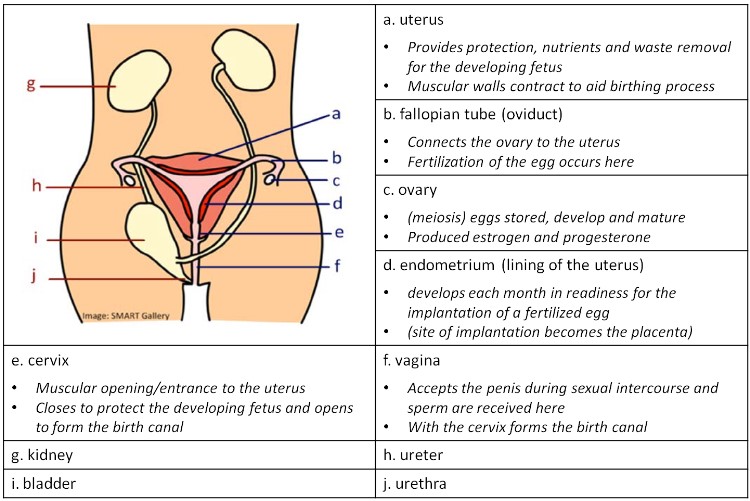
Estrogen and progesterone
- Estrogen and progesterone which are secreted by the mother’s ovaries and then by the placenta, will cause the female reproductive organs to develop in the absence of testosterone
- Absence of fetal testosterone and presence of maternal estrogen and progesterone will lead to the development of female reproductive system
- During puberty, estrogen and progesterone cause the development of secondary sexual characteristics in females, including breast development, menstrual cycle and pubic and armpit hair
Reproductive system
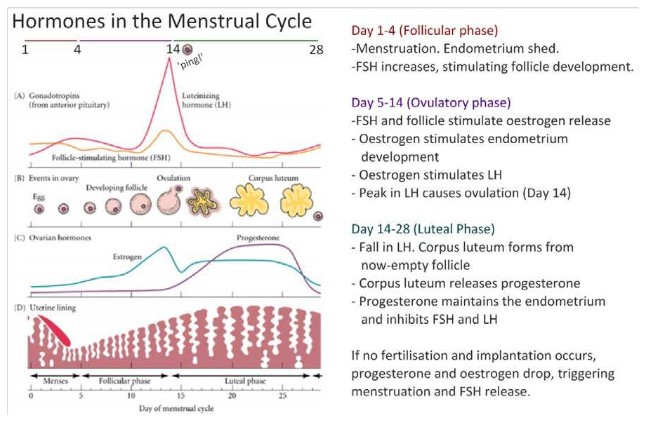
Menstrual cycle
FSH (Follicle stimulating hormone)
- Produced and secreted by the anterior pituitary gland.
- Stimulates the growth of the follicles in the ovaries
- Stimulates egg maturity (egg development)
- Promotes the thickening of the follicle wall.
- Stimulates the secretion of the hormone estrogen.
LH (luteinizing hormone)
- Produced and secreted by the anterior pituitary gland.
- Triggers the release of the egg (ovulation).
- Stimulates the growth of the corpus luteum (secretes estrogen and progesterone).
Estrogen
- Stimulated by FSH
- Produced by the developing follicles in the ovaries and the corpus luteum.
- Promotes the thickening of the uterine wall (endometrium) and the growth of blood vessels, in preparation of egg implantation.
- Stimulates LH in pre-ovulation period
- Inhibits FSH and LH when the estrogen levels are high (around same time as ovulation). This would prevent the development and release of another egg.
Progesterone
- Produced by the ovaries and the corpus luteum.
- Helps maintain the thickening of the uterine wall (endometrium) for egg implantation.
- Inhibit the production of FSH and LH.
IVF (in vitro fertilisation)
- Generally, IVF treatment begins by taking drugs to halt the regular secretion of the hormones FSH and LH. This in turn stops the secretion of progesterone and estrogen and effectively allows the doctor to take control of the timing and egg production of the woman’s ovaries
- The woman is then injected with large amounts of FSH to induce the production of many follicles.
- LH is also injected to promote the release of many ovules (eggs)
- This is called superovulation, which can produce between 10 and 20 eggs
- The eggs are then stimulated to mature by an injections of HCG (Human Chorionic Gonadotrophin), a hormone usually secreted by the developing embryo
- The eggs are surgically removed from the ovary of the woman.
- Sperm is collected from the male individual.
- Many sperm (50,000-100,000) are mixed with the eggs in a petri dish.
- The sperm and eggs in the petri dish are incubated at 37ºC (body temperature).
- The eggs are analyzed for successful fertilization (two nuclei inside the egg).
- Healthy embryos are selected and are transferred into the female uterus for implantation (up to 3 healthy embryos are transferred into the uterus to increase chance of implantation).
- Keep injecting progesterone after implantation
- Pregnancy test is given after about 2 weeks